Abstract
The Association of Reproductive and Clinical Scientists (ARCS) has long promoted the importance of externally accredited training and assessment of scientific staff within assisted conception centres to ensure professional registration and relevant training at all levels. This not only gives scientific staff the opportunity to empower themselves but also acts to ensure assisted conception centres maintain the highest standards of care and quality for patients whilst meeting HFEA requirements for staffing and training. It also provides assurance to patients that treatment is being delivered by highly trained and competent staff. Clinical embryology practice requires intense concentration, with increasingly complex treatment plans and options coupled with the ever-present consequences of clinical error at the forefront of practitioners’ minds, exhaustion and burn out are very real risks. Overloading embryology teams is likely to lead to increased error rates and serious incidents. This guideline aims to bring the sector in line with other Clinical Science specialities to optimise patient care, increase safety, reduce risk (including the risk of legal action against centres and individuals), ensure the use of recognised job titles with appropriate levels of remuneration, and provide centres with a template to work towards for appropriate levels of scientific staffing.
Keywords:
Introduction
The HFEA Fertility treatment 2019 Trends and Figures report (Human Fertilisation and Embrology Authority, Citation2021) indicated that in the UK, between 1991 and 2019, there were approximately 1.3 million IVF treatment cycles, of which just over 69,000 occurred in 2019 alone. With increasing numbers of patients seeking IVF treatment, scientific staff in both the NHS and private sector are under continued pressure to treat more patients and deliver increasingly complex treatments. It is the responsibility of clinic management to use effective workforce planning strategies to ensure any gaps in the workforce are both identified and resolved. Staff at all levels should be employed with appropriate job titles descriptions, professional registration if available and qualifications for the tasks required (HFEA license conditions T13 and T14 (Human Fertilisation and Embrology Authority, Citation2022). The Association of Reproductive and Clinical Scientists (ARCS) and its predecessor the Association of Clinical Embryologists (ACE) has long promoted the importance of externally accredited training and assessment of scientific staff within assisted conception centres to ensure professional registration and relevant training at all levels. This not only gives scientific staff the opportunity to empower themselves but also acts to ensure assisted conception centres maintain the highest standards of care and quality for patients whilst meeting HFEA requirements for staffing and training. It also provides assurance to patients that treatment is being delivered by appropriately trained and competent staff.
It is important to note that the recommendations made in this guideline relating to career pathways, remuneration, and roles and responsibilities are based on nationally published guidance and frameworks for Clinical Scientists and Healthcare Scientists from external bodies including the National Health Service (NHS), Royal College of Pathologists (RCPath), (Citation2015), Academy for Healthcare Science (AHCS, Citation2021) which apply to all Clinical Science specialties and have been adapted to Clinical Embryology.
Clinical embryology practice requires intense concentration, with increasingly complex treatment plans and options coupled with the ever-present consequences of clinical error at the forefront of practitioners' minds, exhaustion and burn out are very real risks. Overloading embryology teams is likely to lead to increased error rates and serious incidents. Recent publications have highlighted the level of work-related stress and injury in the field, with a high proportion of colleagues suffering from work related musculoskeletal disorders and mental health conditions (Priddle et al., Citation2022). This serves to highlight the need for a U.K. staffing guideline.
This document aims to bring the sector in line with other Clinical Science specialities in order to optimise patient care, reduce risk (including the risk of legal action against centres and individuals), ensure the use of recognised job titles with appropriate levels of remuneration, and provide centres with a template to work towards for appropriate levels of scientific staffing.
Career pathway for scientific staff
Organisational structures may vary from clinic to clinic depending on the services provided. ARCS recognised job titles, qualifications and salaries can be found in . These job titles are based upon national NHS job profiles for Healthcare Scientists (National Health Service, Citation2021). Salaries are described using NHS Agenda for Change (AfC) pay scales (National Health Service, Citation2023). These should be used as a guide by all staff in the public and private sector to ensure that staff are appropriately remunerated at all levels commensurate with their job role, experience and qualifications. Career progression by scientific staff can ultimately lead to Associate Membership or Fellowship of the Royal College of Pathologists (RCPath) and entry to the Academy for Healthcare Science (AHCS) higher specialist register. This should be beneficial to the employee in terms of roles they can apply for, the employer with regards to the skills these members of staff can bring to a service and to the standing of the scientific community as a whole in the multidisciplinary field of assisted conception.
Figure 1. Career pathway for scientific staff within a HFEA licensed centre. ARCS recommended and recognised job titles, qualifications, registration (where applicable) and suggested NHS salaries. Based on nationally recognised NHS job profiles for Healthcare Scientists.
*Staff at band 6 and below can only work under the direct supervision (i.e. on-site) of a registered Clinical Scientist.
Note- An MSc or MSc level qualification (e.g. ACE certificate or Diploma) in addition to a BSc is the minimum qualification appropriate for a Clinical Embryologist. Those entering the HCPC register by any route (e.g. the Association of Clinical Scientists, AHCS equivalence) have met this standard. Consultant level staff attain specialist Doctoral level qualifications through completion of the higher specialist training programme and/or attainment of Fellowship of the RCPath via completion of part 2 exams or acknowledgement of equivalence through admission to the AHCS higher specialist register. Whilst a PhD in the field can be used to fulfil some requirements for FRCPath attainment and entrance to the higher specialist register, a PhD cannot be used as a proxy for these qualifications or entrance to the HSS register. Likewise, FRCPath attainment alone may not fulfill all the standards for entry to the higher specialist register.
Staff in supporting roles may be used to assist the clinical scientific workforce, but it is important to note that they cannot be used as a replacement. A state registered Clinical Scientist must always be on-site to supervise clinical procedures. See Appendix A for Reproductive Science Assistant, Associate and Practitioner job roles.
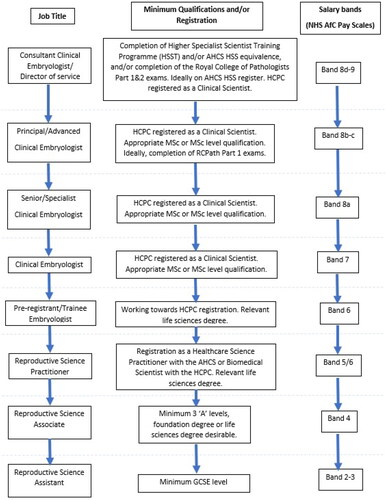
The opportunities for Reproductive Scientists to develop their roles have led to changes in the workforce structure and broadened their roles and responsibilities. There are clear job titles, profiles and career pathways for NHS Clinical Scientists (National Health Service, Citation2021), and historically reproductive scientists have not been properly aligned to these. The structure and roles () clarify responsibilities and align job titles with nationally recognised standards in Clinical Science specialisms.
Roles and responsibilities
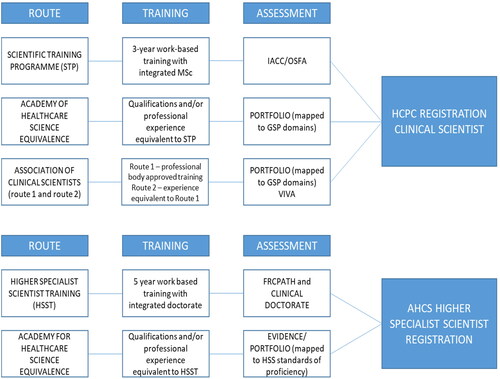
The new training schemes that emerged through the ‘Modernising Scientific Careers’ (MSC) programme represented a monumental change in the way that Reproductive Scientists were trained in the UK. They aimed to standardise the training of Clinical Scientists and Biomedical Scientists in all disciplines and, for the first time, to allow a direct and clear comparison with clear equivalence between the training and qualifications of healthcare scientists and medical doctors. Complementary to this, ARCS is developing programmes for practitioners, assistants and associate level staff. In addition, the Royal College of Pathologists (RCPath) exams are now available to Reproductive Scientists either within the Higher Specialist Scientist Training (HSST) programme or as a standalone route to registration as a higher specialist (Consultant) with the AHCS. At many levels there are also routes to equivalence ().
Consultant embryologist (reproductive scientist)
Assisted conception centres performing IVF in the U.K. should employ a Consultant Clinical Scientist who has undertaken higher specialist training either through completion of the National School of Healthcare Science (NSHCS) HSST programme or equivalence through the AHCS and have gained entry to the AHCS higher specialist register. Both routes of qualification should, ideally, include completion of the Royal College of Pathologists Fellowship examinations although it is recognised that this is not strictly a requirement for the AHCS Equivalence route to HSS. The Consultant Embryologist is responsible for the strategic direction of the scientific elements of the service and the laboratories, this includes research and development. It is important to note that qualification alone does not make an individual a Consultant (i.e. an individual who is not in a consultant post does not become a consultant because they have attained the necessary qualifications unless they are recruited in to a consultant post). As per guidelines from the RCPath (Royal College of Pathologists, Citation2014), job descriptions for new consultant appointments should be submitted to the RCPath for approval prior to job advert. Consultant appointments should be made with advice and input from external assessors in the speciality at the RCPath, this should include an external assessor at interview, as with medical consultants.
The Consultant does not need to be full time, but they should have enough time allocated to be able to effectively oversee all scientific activities in a centre. ARCS recognises that some Consultant appointments will have been made prior to these recommendations and that some individuals working in Consultant posts will not meet these requirements. To address this, ARCS recommends that embryologists historically appointed to Consultant roles apply to the AHCS via the equivalence route for entry to the higher specialist scientist register.
Consultant clinical scientists are directly equivalent to medical Consultant counterparts. In 2012 the Academy of Medical Royal Colleges stated ‘Entry to HSST will require a defined masters degree and successful completion of the STP followed by five years of workplace based training, which is at least as long and arduous as that demanded from medically qualified consultants…’ and ‘there are top-level healthcare scientists currently within the workforce, whose training and expertise justify a status that is equivalent to that enjoyed by medically qualified consultants…’ (Academy of Medical Royal Colleges, Citation2012).
Principal/advanced clinical embryologist (reproductive scientist)
These members of staff act in supporting roles to consultant healthcare scientists and should ideally be undertaking or have completed higher specialist training themselves (this can include those who have attained RCPath part 1 exams or Diplomate (DipRCPath) status). They may in some circumstances deputise, where appropriately trained and qualified, for the consultant in their absence. The principal embryologist will bear greater responsibility for operational elements of laboratory organisation and practice (where the overall responsibility rests with the consultant).
Senior/specialist embryologist (reproductive scientist)
Senior reproductive scientists support consultant and principal scientists in their roles. They will usually have undertaken significant further training after completing their state registration as Clinical Scientists with the Health and Care Professions Council (HCPC). Senior Embryologist (Reproductive Scientist) is usually the highest level achievable by staff who have not started training for or obtained higher specialist scientist (HSS) status.
Embryologist (reproductive scientist)
All Embryologists must be state registered Clinical Scientists with the HCPC. Clinical Scientist is a protected title in the UK. Registration with the HCPC shows both employers and the public that their employee meets set standards in terms of training, education, professional skills and behaviour. Clinical embryology and assisted conception procedures in the laboratory should only be carried out when a registered clinical embryologist (clinical scientist) is on-site. This includes weekend and on-call work.
Trainee/pre-registrant embryologist (reproductive scientist)
Those working towards registration with the HCPC as a Clinical Scientist should be employed on band 6 AfC salaries.
The HFEA Code of Practice (Human Fertilisation and Embrology Authority, Citation2018) states ‘all healthcare scientists working in licensed centres should be registered or show evidence of working towards registration with the Health & Care Professions Council (HCPC)’. Following the closure of the ACE certificate to new applications in September 2013 the main route for training and registration for trainee embryologists has been via the Scientist Training Programme (STP). The first cohort of NHS funded STPs started in 2011. The STP is a three-year fixed term workplace based reproductive science training programme that includes completion of a part time Master’s degree. Upon successful completion of the Master’s degree, an online training portfolio and the observed structured final assessments (OSFAs) or independent assessment of clinical competence (IACC), or equivalent end point assessments, trainees will obtain a Master’s degree from their host university and a certificate of attainment from the Academy for Healthcare Science (AHCS). Trainees are then eligible to apply for registration with the Health Care Professions Council (HCPC) to become registered Clinical Scientists.
In 2018 ACE was involved in developing a new employer funded pilot scheme for STP trainees in Reproductive Science (Embryology or Andrology) with the National School of Healthcare Science (NSHCS). This allowed centres that could not secure funding for STP trainees to fund their own. The programme was designed so that if employers were unable to arrange the required first year rotations trainees could choose to complete the rotational elements via self-directed learning. With ACE developed guidance these trainees could then go on to meet the rotational requirements of the training as well as the other elements of the programme to become HCPC registered.
All STP trainees should be considered supernumerary, with the focus on the training experience, but will inevitably be involved in ongoing service delivery as part of their training. Their training must be supervised by a HCPC registered clinical scientist at all times. Trainees will be learning both the practical skills required in a laboratory and the knowledge and understanding to make clinical decisions and give clinical advice to both patients and other healthcare professionals.
Alternative routes to registration for trainee/pre-registrant embryologists include completion of the Academy for Healthcare Science (AHCS) Certificate of Equivalence to the Scientist Training Programme or the Association of Clinical Scientists (ACS) Certificate of Attainment via route 1 or route 2. International candidates that are fully trained and qualified who have evidence of competently practicing abroad can apply directly to the HCPC via the international entry route.
Staffing levels in the assisted conception unit laboratory
When staffing assisted conception laboratories, consideration should be given to ensuring sufficient numbers of qualified personnel are available to undertake the expected workload, including the need for suitable supervisory support for scientific staff in roles that require it. The number of treatment cycles should be taken into account along with the amount of time needed to perform non-laboratory administrative tasks, training of staff, CPD, quality management and any meetings that may be required to ensure the efficient running of the service. As Clinical Scientists, Embryologists will also engage in significant patient contact during consultations and treatment, this should also be taken into account. The need for on-call and weekend cover should be factored into workforce plans as well as the impact of annual leave or sickness. ARCS recommends that centres should employ one state registered Clinical Scientist (Embryologist) for every 80–100 cycles of treatment undertaken. This number may vary through economies of scale depending on the size of the centre, the number of cycles performed, the availability of support staff and the complexity of the workload. Centres that perform significantly more cycles per embryologist should justify this by, for example, having a higher number of available support staff, significant improvements in efficiency through automation or less complex workloads/cases. Regular (ideally annual) assessment of workforce should be undertaken.
ESHRE guidelines (ESHRE Guideline Group on Good Practice in IVF Labs, De los Santos et al., Citation2016) support the ARCS view, their suggestion being that ‘clinics that perform up to 150 retrievals and/or cryopreservation cycles per year should always have a minimum of two qualified Clinical Embryologists’. ASRM have a similar opinion, adopting a ‘sliding scale’ approach to embryology staffing, recommending an embryologist per 50–75 cycles for the first 150 cycles, per 75–100 cycles up to 300 cycles and per 75–120 cycles up to 600 cycles (Practice Committees of the American Society for Reproductive Medicine (ASRM) and the Society for Reproductive Biologists and Technologists (SRBT), Citation2022). Whilst the ASRM appear to suggest a higher number of cycles per embryologist at the upper end of the 300–600 cycle range, it is important to note that U.K. Embryologists and embryology practice differ from both our European and USA counterparts, with UK embryologists performing a more patient facing role (e.g. consultations) and having a greater regulatory ‘burden’.
Independent groups such as Alikani et al. (Citation2014), Veiga et al. (Citation2022) and Lee et al. (Citation2023) have attempted to calculate the number of staff required to run an Embryology laboratory by undertaking time and motion analysis of work-based tasks. Alikani et al. (Citation2014) concluded that an embryologist was required per 100 cycles, whereas Veiga et al. (Citation2022) concluded that one Embryologist would be required per 102 IVF/ICSI cycles where time lapse is used. These publications are broadly in line with ARCS recommendations despite not taking into account activities such as staff training and teaching, the patient facing role of the embryologist (which is greater in UK practice), or the additional regulatory burden placed on U.K. clinical embryology through the HF&E act and HFEA regulation of the sector. Alikani et al. (Citation2014) assumed 10 days leave in a year, a much lower level than normally allocated in the U.K. Alikani et al. (Citation2014) and Veiga et al. (Citation2022) did not include time allocated to the duties of the laboratory director.
This ARCS staffing guideline is, therefore, in line with national counterparts whilst taking into account the unique and complex aspects of the embryology speciality in the UK, including a well-established and world leading training scheme and career pathway designed to develop highly skilled, qualified and professionally recognised individuals to ensure the highest quality of care for our patients.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Academy for Healthcare Science. (2021). Academy for Healthcare Science (AHCS) Standards for Education and Training and Good Scientific Practice. Retrieved from https://www.ahcs.ac.uk/education-training/standards/ https://nshcs.hee.nhs.uk/wp-content/uploads/2021/04/AHCS-Good-Scientific-Practice-2021.pdf
- Academy of Medical Royal Colleges. (2012). Retrieved from https://www.aomrc.org.uk/wp-content/uploads/2016/05/AOMRC_Statement_2012-03-22-Higher_Specialist_Scientific_Training.pdf
- Alikani, M., Go, K. J., McCaffrey, C., & McCulloh, D. H. (2014). Comprehensive evaluation of contemporary assisted reproduction technology laboratory operations to determine staffing levels that promote patient safety and quality care. Fertility and Sterility, 102(5), 1350–1356. https://doi.org/10.1016/j.fertnstert.2014.07.1246
- ARCS. (n.d.). Retrieved from https://www.arcscientists.org/routes-to-registration/
- ESHRE Guideline Group on Good Practice in IVF Labs, De los Santos, M. J., Apter, S., Coticchio, G., Debrock, S., Lundin, K., Plancha, C. E., Prados, F., Rienzi, L., Verheyen, G., Woodward, B., & Vermeulen, N. (2016). Revised guidelines for good practice in IVF laboratories (2015). Human Reproduction, 31(4), 685–686. https://doi.org/10.1093/humrep/dew016
- Human Fertilisation and Embrology Authority. (2018). HFEA code of practice (9th Ed.). Retrieved from https://portal.hfea.gov.uk/knowledge-base/read-the-code-of-practice/
- Human Fertilisation and Embrology Authority. (2021). HFEA Fertility treatment 2019: Trends and figures. UK statistics for IVF and DI treatment, storage, and donation. Retrieved from https://www.hfea.gov.uk/about-us/publications/research-and- data/fertility-treatment-2019-trends-and-figures/
- Human Fertilisation and Embrology Authority. (2022). Licence Conditions. https://portal.hfea.gov.uk/knowledge-base/licence-conditions/
- Lee, Y. S. L., Catt, S., Cooke, S., Fisk, K., Mackenzie, J., Mullen, J., Pohl, N., Rabbitt, T., Rutherford, T., & Tully, C. (2023). Guidelines for best practice for staffing of ART laboratories and professional development of IVF scientists. Fertility & Reproduction, 05(03), 163–175. https://doi.org/10.1142/S2661318223500160
- National Health Service. (2021). Nationally recognised job profiles for Healthcare Scientists. Retrieved from https://www.nhsemployers.org/system/files/2021-06/healthcare-science-profiles.pdf
- National Health Service. (2023). Pay scales for 2023/24 | NHS Employers. Retrieved from https://www.nhsemployers.org/articles/pay-scales-202324
- Practice Committees of the American Society for Reproductive Medicine (ASRM) and the Society for Reproductive Biologists and Technologists (SRBT). (2022). Comprehensive guidance for human embryology, andrology, and endocrinology laboratories: Management and operations: A committee opinion. Fertility and Sterility, 117(6), 1183–1202. https://doi.org/10.1016/j.fertnstert.2022.02.016
- Priddle, H., Pickup, S., & Hayes, C. (2022). Occupational health issues experienced by UK embryologists: Informing improvements in clinical reproductive science practice. Human Fertility, 25(4), 608–617. https://doi.org/10.1080/14647273.2021.1871782
- Royal College of Pathologists. (2014). Guidance on the appointment of consultant clinical scientists to employing bodies in the UK Sept 2014. Retrieved from rcpath.org
- Royal College of Pathologists. (2015). Royal college of pathologists higher specialist scientist curriculum in reproductive science. Retrieved from https://www.rcpath.org/static/53f12f6d-a304-498f-b5304ffc756b62df/Reproductive-science-HSST-Curriculum.pdf
- Veiga, E., Olmedo, C., Sánchez, L., Fernández, M., Mauri, A., Ferrer, E., & Ortiz, N. (2022). Recalculating the staff required to run a modern assisted reproductive technology laboratory. Human Reproduction, 37(8), 1774–1785. https://doi.org/10.1093/humrep/deac121
Appendix A
Reproductive science practitioners, associates and assistants
In order to meet workforce demands the 2011 ACE future workforce of the embryology laboratory document stated that assisted conception units may seek to recruit laboratory practitioners, associates and assistants. These members of staff will generally undertake protocol driven tasks, they should not be making clinical decisions or giving clinical advice and should always be supervised by a HCPC registered Clinical Scientists. Off-site supervision, for example by telephone, is inappropriate for staff working at these levels.
The 9th edition of the HFEA Code of Practice (CoP) states that all ‘Healthcare scientists employed in roles not yet requiring state registration (e.g. aspirant groups, healthcare science assistants and healthcare science practitioners) should follow an appropriate induction and training programme for the tasks performed’. In the case of healthcare science practitioners, whose roles are described in include tasks that involve the handling of human gametes or embryos for treatment, ARCS strongly recommends that these staff should seek some form of registration as well as evidence of external assessment of competence. details tasks that may be undertaken by more junior assistant and associate roles.
Experienced practitioners who have been trained in house should apply for registration now. This can be done either via the AHCS Certificate of Equivalence to the Practitioner Training Programme or by obtaining registration as a Biomedical Scientist via the Institute of Biomedical Scientists (IBMS) Certificate of Competence by Equivalence. Please see the ARCS website “Routes to Registration” education pages for further details.
Table A1. Roles for reproductive science practitioners in HFEA-licensed centres*.
Table A2. Roles for assistants and associates in HFEA-licensed centres.