Abstract
Male infertility is a global health concern. The effectiveness of interventions developed to improve males’ knowledge of fertility regulation and fertility-related risk factors remains unclear. This systematic review aimed to synthesize and evaluate the evidence for these interventions. Four databases were searched from inception to June 2023. Eligible studies examined interventions to increase fertility knowledge among presumed fertile males aged ≥16 years of age. Conference abstracts, protocols and studies without sex-disaggregated results for males were excluded. A narrative synthesis without meta-analysis was performed. A total of 4884 records were identified. Five studies (reported in six publications), all conducted in high-income countries, were included. Two were randomized control trials, and three were experimental studies. Interventions were delivered in person by a health professional (n = 3), online and via a mobile app. All studies showed a significant improvement in knowledge of fertility or fertility-related risk factors from baseline to follow-up. The largest improvement was observed for secondary and vocational students. A moderate, long-term retainment of knowledge was observed at two-year follow-up in one study. Available evidence suggests interventions to improve males’ fertility knowledge are effective, particularly for younger, less educated males.
Introduction
Infertility is a disorder of the male and female reproductive system defined by the failure to achieve pregnancy after 12 months or more of regular unprotected sexual intercourse (World Health Organization, Citation2021). The prevalence of male fertility issues has been increasing, and there has been a hypothesized decline in sperm quality (Levine et al., Citation2023) which some authors suggest is due in part to modifiable health behaviours such as smoking, alcohol, drug use and caffeine intake (W. Chen et al., Citation2023; Finelli et al., Citation2021; Kovac et al., Citation2015). Male factor infertility is now believed to be a contributing cause in 30–50% of fertility health issues experienced by couples (Agarwal et al., Citation2021; Eisenberg et al., Citation2023; Mannucci et al., Citation2021). Male subfertility and infertility have been described as predictors of future health challenges (Stentz et al., Citation2020) and are associated with cardiovascular disease, diabetes, prostate cancer, testicular cancer and mortality risk (T. Chen et al., Citation2022; Walsh, Citation2011). Improving male knowledge of fertility and fertility-related risk factors may therefore help to improve men’s reproductive health, general health and well-being, as well as their fertility (Harrison et al., Citation2023).
Previous research exploring fertility knowledge has predominantly focused on females (Bretherick et al., Citation2010; Daniluk et al., Citation2012). Where this research has included males, results indicate males may be particularly uninformed (Hviid Malling et al., Citation2022) and have low levels of knowledge of fertility, relative to females (Bunting et al., Citation2012; Hammarberg et al., Citation2017). For example, research suggests males lack knowledge of the steep decline in female fertility with age (Boivin et al., Citation2019) and overestimate the chances of fathering a child at the time of ovulation (Bunting et al., Citation2012). It also suggests males are unaware of the associations between male fertility outcomes and substance use (e.g., smoking), health-related risks such as sexually transmitted infections and sources of excessive heat such as laptops and hot baths (Daumler et al., Citation2016). Poor knowledge of fertility and fertility-related risk factors could lead males to inadvertently expose themselves to risks and delay help-seeking behaviour, assessment and treatment (Harrison et al., Citation2023).
To address the public’s low knowledge of fertility, researchers have developed and implemented interventions to improve knowledge of female fertility and fertility-related risk factors (Conceição et al., Citation2017; García et al., Citation2016). Overall, these efforts have been shown to be effective for males and females. For example, female university students in Canada were found to have a twofold increase in correct answers to a test on fertility following a presentation about fertility (Williamson et al., Citation2014). The fertility knowledge of males and females was also found to increase significantly following the provision of fertility information online (Boivin et al., Citation2018). However, there remains a lack of clarity about the effectiveness of these interventions in improving male knowledge of fertility and fertility-related risk factors, particularly of factors that may affect male fertility. This is because much of the literature including males has not presented sex-disaggregated results (Boivin et al., Citation2018). Moreover, these studies have primarily sampled highly educated individuals (Maeda et al., Citation2020; Stern et al., Citation2013; Williamson et al., Citation2014), couples (Chan et al., Citation2022), people who have undergone fertility treatment and those struggling to conceive (Halleran et al., Citation2022; Mahey et al., Citation2018; Pedro et al., Citation2018). Little is known about the fertility knowledge of presumed fertile males from the general population and the effectiveness of interventions designed to improve this knowledge.
The aim of this systematic review was to describe the existing literature on interventions designed to improve male knowledge of fertility and fertility-related risk factors and evaluate the effectiveness of these interventions.
Materials and methods
The systematic review was prospectively registered with PROSPERO (registration number CRD42023449305) and is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., Citation2021).
Search strategy
We searched three main bibliographic databases - Embase (Ovid), PsycInfo (Ovid) and PubMed – and the Cochrane Database of Systematic Reviews (CDSR), on 05 July 2023, for records published from inception to July 2023. We combined relevant medical subject heading (MeSH) terms and word variants for ‘male’, ‘intervention’, ‘fertility’ and ‘knowledge’ (see Supplementary Table 1 for our search strategy). The reference lists of eligible studies and retrieved systematic reviews were also hand-searched to identify additional relevant articles.
Study selection
The eligibility criteria were informed by the PICO (Population, Intervention, Comparison, Outcome) framework presented in . Eligible studies: (1) were randomized controlled trials (RCTs) or experimental studies that included a pre-post analysis of the intervention; (2) presented sex-disaggregated results for males aged ≥16 years; and (3) reported changes in knowledge of fertility and/or fertility-related risk factors. We excluded animal studies and studies that included females (without presenting sex-disaggregated data), males experiencing sub- or infertility, or children under 16 years.
Table 1. PICO framework.
To identify articles of potential relevance, two reviewers (SK and CH) independently screened the first 10% of titles and abstracts against the eligibility criteria in a pilot phase (McDonagh et al., Citation2008) in Rayyan, a web-based software programme that facilitates systematic reviews (Ouzzani et al., Citation2016). This helped to identify any discrepancies in our interpretation of these criteria. Disagreements were discussed and resolved by consensus. This process was repeated at the full-text screening stage.
Data extraction and synthesis
We extracted data on study author, year of publication, country, design, participants (sex, sample size, mean age), intervention characteristics (study, setting, recruitment, methods) and outcomes pertaining to the improvement of fertility knowledge.
To understand the effectiveness of each included intervention, the change in male knowledge of fertility and fertility-related risk factors from baseline to follow-up (i.e. post-intervention) was extracted, tabulated and narratively synthesized.
Quality assessment
The methodological quality of the included studies was evaluated using the revised Cochrane Risk of Bias 2 tool for randomized trials (Sterne et al., Citation2019) and the ROBINS-I tool for non-randomized intervention studies (Sterne et al., Citation2016). Included studies were evaluated across five domains: (1) bias due to randomization/non-randomization; (2) deviation from the intended intervention; (3) missing outcome data; (4) measurement of outcome; and (5) selection of reported results. Each study was assigned an overall quality rating of low, some or high concern.
Results
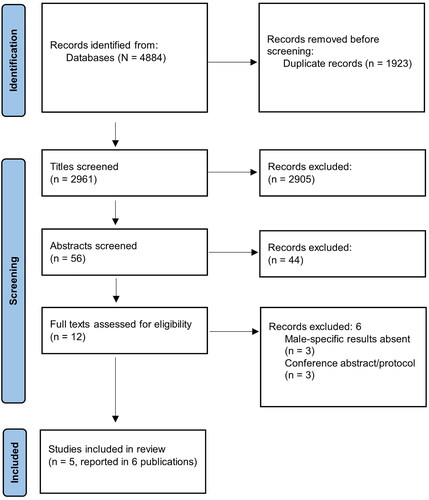
The PRISMA flow diagram in shows we identified 4884 records and screened 2961 unique titles and 56 abstracts. After abstract screening, a further 44 records were excluded. The most common reason for exclusion at this stage was that the literature did not pertain to fertility knowledge or did not include a presumed fertile population. The remaining 12 articles underwent full-text screening and six were excluded because they were conference abstracts or protocols or did not present sex-disaggregated results for males. This resulted in five studies (reported in six publications) being included. No additional relevant literature was identified from searching the references of the included studies and relevant reviews.
Study characteristics
As shown in , the five included studies were published between 2016 and 2021 and were conducted in Canada (n = 2) (Kruglova et al., Citation2021; Thomson et al., Citation2016), Poland (Baczek et al., Citation2020), Sweden (Bodin et al., Citation2018) and Japan (Maeda et al., Citation2016, Citation2018). Two were RCTs (Bodin et al., Citation2018; Maeda et al., Citation2016) and three were experimental studies (Baczek et al., Citation2020; Kruglova et al., Citation2021; Thomson et al., Citation2016). Two studies recruited only students (mean age: 17.5 years (Baczek et al., Citation2020; Thomson et al., Citation2016)) and three studies recruited from the general population (mean age range: 28.4 to 31.5 years). Two studies assessed interventions delivered to males only (Bodin et al., Citation2018; Kruglova et al., Citation2021). The remaining three involved interventions delivered to both males and females.
Table 2. Study characteristics of the included studies.
Interventions included preconception counselling delivered by nurse-midwives during sexual health visits (Bodin et al., Citation2018), the self-guided use of a mobile health app (mHealth app) for two weeks (Kruglova et al., Citation2021), an animated educational video delivered to medical students during a university lecture (Thomson et al., Citation2016), an educational class on human fertility delivered in a school during lesson time by a midwife (Baczek et al., Citation2020) and an educational brochure on infertility facts and risks delivered online (Maeda et al., Citation2016, Citation2018). Interventions targeted participants knowledge of male and female fertility (Baczek et al., Citation2020; Bodin et al., Citation2018), primarily female fertility (Maeda et al., Citation2018; Thomson et al., Citation2016) and male-specific fertility (Bodin et al., Citation2018; Kruglova et al., Citation2021).
All studies used surveys to assess participants’ knowledge of the topics covered by the intervention before and after the intervention’s receipt (i.e. at baseline and follow-up). Follow-up knowledge scores were measured at varying durations across the five studies, from immediately after the implementation of the intervention (Baczek et al., Citation2020) to two years after (Maeda et al., Citation2018).
For most studies, knowledge scores were presented as mean scores and percentages relating to the number of survey items answered correctly at baseline and follow-up. In two of the included studies, the mean scores for the number of items correctly identified by participants as risk factors for infertility were reported (Bodin et al., Citation2018; Kruglova et al., Citation2021). In one of the RCTs (Bodin et al., Citation2018), males were asked to name lifestyle factors that could put male fertility at risk, at baseline and follow-up. The experimental study asked males to identify which factors posed a risk to male fertility from a list of 24 factors (Kruglova et al., Citation2021).
Quality of included studies
The two RCTs (Bodin et al., Citation2018; Maeda et al., Citation2016, Citation2018) and one of the experimental studies (Kruglova et al., Citation2021) were rated to be of low concern for bias (Supplementary Table 2). The risk of bias in the other two experimental studies (Baczek et al., Citation2020; Thomson et al., Citation2016) was rated to be of ‘some concern’ due to a lack of validation for the missing outcome data.
Knowledge of fertility
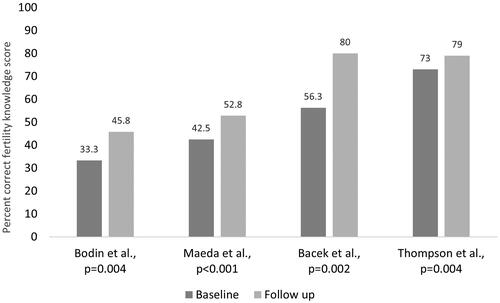
Four studies showed significant improvements in knowledge of fertility from baseline to follow-up (). For fertility knowledge scores, the largest improvement (24%) was observed for an experimental study of an educational class for secondary and vocational students (Baczek et al., Citation2020). The smallest improvement (9.7%) was reported by the experimental study which used educational animations for medical students (Thomson et al., Citation2016). The two-year study of the educational brochure intervention measured both immediate (Maeda et al., Citation2016) and long-term (Maeda et al., Citation2018) changes in knowledge; knowledge gain attenuated from +25.8% to +11.2% between these time points.
Knowledge of fertility-related risk factors
Three studies showed a significant improvement in participants’ knowledge of fertility-related risk factors from baseline to follow up (). The greatest improvement was observed for the intervention involving self-guided use of an mHealth intervention for two weeks (Kruglova et al., Citation2021). Results showed that, on average, males correctly identified six more risk factors at follow up than at baseline. The most commonly identified risk factors in these studies, prior to intervention receipt, were smoking, alcohol consumption (Bodin et al., Citation2018; Kruglova et al., Citation2021), stimulants, having many sexual partners and malformations/injuries of the genital organs (Baczek et al., Citation2020). These risk factors were reported by over 50% of participants in the RCT (Bodin et al., Citation2018) and identified correctly by over 70% of participants in the experimental study (Kruglova et al., Citation2021). Other commonly identified risk factors (>70% of the participants in the experimental study) were drug use, advanced age, pain or injury to the testicles or scrotum, steroid use and cancer treatment. Conversely, less than 30% of participants correctly identified the fertility risks associated with frequent bicycling or riding horses, overuse of electric devices, frequent hot tub use, delayed puberty, testicle size and hernia repair, prior to the intervention (Kruglova et al., Citation2021). After the intervention, the mean percentage of males who correctly identified the assessed risk factors increased from 46.3% to 72.3%. The percentage change in knowledge was over 100% for hernia repair, testicle size, delayed puberty, frequent bicycling or horse riding, overuse of electronic devices, frequent use of a laptop on one’s lap, wearing tight trousers and frequent use of hot tubs.
Table 3. Mean number of fertility-related risk factors identified at baseline and follow-up.
Discussion
The purpose of this systematic review was to summarize the primary literature on interventions to improve male knowledge of fertility and fertility-related risk factors and examine their effectiveness. A limited number of interventions were identified. Intervention design, content and delivery varied but findings were consistent, showing a positive impact on male knowledge of fertility and fertility-related risk factors across all studies.
The findings of our systematic review provide valuable insights into the potential of these interventions. Although limited, the research we reviewed suggests interventions involving counselling, education and mobile apps can all have a positive effect on male fertility knowledge. However, the degree of improvement varied, and some interventions demonstrated greater improvements than others. Several factors may contribute to this variation, including differences in study design, duration from baseline to follow-up, delivery methods and characteristics of the study population. For example, both RCTs demonstrated improvements in knowledge gain (Bodin et al., Citation2018; Maeda et al., Citation2016, Citation2018), and studies measuring knowledge acquisition immediately after receipt of the intervention reported better results than those that did not (Baczek et al., Citation2020). This suggests that long-term fertility knowledge attainment may be more difficult to achieve. Moreover, interventions delivered to individuals with higher levels of education were found to be less effective (Thomson et al., Citation2016). This suggests that educational interventions might be most impactful when targeted at younger, less educated individuals. Our results therefore highlight the potential to enhance fertility knowledge from an early age.
The positive effects observed for younger student populations emphasize the importance of including fertility education in schools as part of relationship and sex education to encourage informed decision-making and safeguard reproductive health. Future research in this area needs to explore the impact of delivering fertility education interventions designed for males and females, in educational settings, with pupils of different ages (Harrison et al., Citation2023).
However, it is important to acknowledge that the long-term sustainability of the knowledge gains demonstrated by the included studies remains uncertain. The RCTs measured knowledge gain over a longer period but only two RCTs were included; longitudinal assessment of knowledge gain is therefore a critical area for future research in this area to comprehensively evaluate the effectiveness of interventions in the context of male fertility knowledge (Daniluk & Koert, Citation2015; Harrison et al., Citation2023). This research would contribute to a deeper understanding of the long-term impact and potential benefits of preconception fertility education for both males and females.
Our systematic review also revealed substantial improvement in participants’ knowledge of fertility-related risk factors. Participants in the mHealth intervention demonstrated a significant improvement in their ability to identify more risk factors at follow-up. This is important for preconception education. The pre-intervention identification of common lifestyle factors such as smoking and alcohol consumption suggests that participants are already aware of these factors. However, the interventions significantly increased knowledge of less commonly recognized risk factors. Results should, however, be interpreted with caution due to the limited number of studies included in the current review.
Our findings point to the need to develop and implement interventions to improve fertility knowledge and highlight their potential benefit for male reproductive health, general health and fertility. However, it is important to recognize current trends in andrology and the inappropriateness of interventions designed to improve knowledge and health behaviours for biological fertility disorders that show no signs of recovery. For example, infertility cases that are not due to hormonal deficiency or physical obstruction, are idiopathic in nature or due to testicular cancer and associated treatments without having engaged with fertility preservation (Bhattacharya et al., Citation2023; Majumdar & Bhattacharya, Citation2013; Tran et al., Citation2022).
Implications, strengths and limitations
The positive impact of counselling, education and mobile app interventions suggests the potential for the development and implementation of interventions in clinical settings. Health care professions could proactively incorporate these educational strategies in routine clinical consultations to stimulate discussions with male patients and enhance male fertility awareness and knowledge. Clinicians could additionally be attentive to identifying high-risk groups or individuals who would particularly benefit from fertility education. Tailoring interventions to specific profiles could also enhance their effectiveness ensuring targeted support. As interventions have a more positive effect for younger student populations, health care professionals could focus on incorporating fertility education into routine healthcare visits for this demographic. The review findings also suggest the need for fertility education to be integrated into existing reproductive health programmes and relationship and sex education in schools. Integrating fertility education in these ways, with a focus given to male, as well as female, fertility could contribute to enhanced informed decision making and reproductive health (Harrison et al., Citation2023). Future research should explore the acceptability of different interventions in health care settings in addition to the feasibility of incorporating these educational strategies as part of routine care.
While the current systematic review provides valuable insights into interventions to improve male knowledge of fertility and fertility-related risk factors, it is not without limitations. Firstly, very few eligible studies were identified. This highlights the need for further research in this area and the potential lack of generalizability of the results. For example, none of the included studies were conducted in low-income countries, indicating a need to replicate this research and explore the impact of interventions in diverse global settings. Understanding the effectiveness of interventions in low-income countries is crucial for addressing disparities in sexual and reproductive health knowledge (Mon Kyaw Soe et al., Citation2018). This need is particularly pertinent as research shows sexual and reproductive health knowledge to be sub-optimal in low-income countries where sexually transmitted infections (STIs) are one of the most common causes of couple infertility (e.g. Mansor et al., Citation2020; Paganella et al., Citation2021). Future research should explore the impact of interventions designed to improve male (and female) knowledge of the associations between STIs and fertility and how to prevent and seek early treatment for these infections. Findings from such research could potentially support initiatives designed to improve sexual and reproductive health, including fertility, in low-, middle- and high-income countries and thus diverse socio-economic contexts. Secondly, the heterogeneity of the included studies makes it difficult to draw definitive conclusions about, for example, the best ways to disseminate fertility educational information and the long-term sustainability of knowledge gain. Future research should focus on longitudinal evaluations to comprehensively evaluate the long-term effectiveness of interventions over extended periods. Future research should also explore the impact of delivering fertility education interventions to both males and females in educational settings, considering pupils of different ages. This research could provide insights into the age-specific acceptability of fertility interventions in addition to educational needs.
Thirdly, we did not search grey literature, where the results of other relevant interventions may be reported. Notwithstanding these limitations, the current systematic review has methodological strengths including a priori registration of the review’s protocol, searching of multiple databases, handsearching of references and two independent researchers screening the identified records.
Conclusion
This systematic review shows the positive impact interventions to improve knowledge of fertility and fertility-related risk factors can have for males, particularly those who are younger and have less educational attainment. Fertility-related interventions are therefore suggested to be important to ensure males are equipped with the information they need to make informed lifestyle and reproductive choices. Future research should focus on assessing the long-term effects of these interventions on male fertility knowledge and their impact on reproductive decision-making and behaviour.
Supplemental Material
Download MS Word (14.3 KB)Supplemental Material
Download MS Word (13.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are underlying this review will be shared on reasonable request made to the corresponding author.
Additional information
Funding
References
- Agarwal, A., Baskaran, S., Parekh, N., Cho, C. L., Henkel, R., Vij, S., Arafa, M., Panner Selvam, M. K., & Shah, R. (2021). Male infertility. Lancet, 397(10271), 319–333. https://doi.org/10.1016/S0140-6736(20)32667-2
- Baczek, G., Padzik, M., Duda, T., & Giermaziak, W. (2020). The youth’s knowledge of human fertility and reproductive age - evaluation of educational and health care programme. Ginekologia i Poloznictwo, 58(4), 9–20.
- Bhattacharya, I., Sharma, S. S., & Majumdar, S. S. (2023). Etiology of male infertility: An update. Reproductive Sciences. Advance online publication. https://doi.org/10.1007/s43032-023-01401-x
- Bodin, M., Tydén, T., Käll, L., & Larsson, M. (2018). Can reproductive life plan-based counselling increase men’s fertility awareness? Upsala Journal of Medical Sciences, 123(4), 255–263. https://doi.org/10.1080/03009734.2018.1541948
- Boivin, J., Koert, E., Harris, T., O'Shea, L., Perryman, A., Parker, K., & Harrison, C. (2018). An experimental evaluation of the benefits and costs of providing fertility information to adolescents and emerging adults. Human Reproduction, 33(7), 1247–1253. https://doi.org/10.1093/humrep/dey107
- Boivin, J., Sandhu, A., Brian, K., & Harrison, C. (2019). Fertility-related knowledge and perceptions of fertility education among adolescents and emerging adults: A qualitative study. Human Fertility, 22(4), 291–299. https://doi.org/10.1080/14647273.2018.1486514
- Bretherick, K. L., Fairbrother, N., Avila, L., Harbord, S. H., & Robinson, W. P. (2010). Fertility and aging: Do reproductive-aged Canadian women know what they need to know? Fertility and Sterility, 93(7), 2162–2168. https://doi.org/10.1016/j.fertnstert.2009.01.064
- Bunting, L., Tsibulsky, I., & Boivin, J. (2012). Fertility knowledge and beliefs about fertility treatment: Findings from the International Fertility Decision-making Study. Human Reproduction, 28(2), 385–397. https://doi.org/10.1093/humrep/des402
- Chan, S. L., Thumboo, J., Boivin, J., Saffari, S. E., Yin, S., Yeo, S. R., Chan, J. K. Y., Ng, K. C., Chua, K. H., & Yu, S. L. (2022). Effect of fertility health awareness strategies on fertility knowledge and childbearing in young married couples (FertStart): Study protocol for an effectiveness-implementation hybrid type I multicentre three-arm parallel group open-label randomised clinical trial. BMJ Open, 12(1), e051710. https://doi.org/10.1136/bmjopen-2021-051710
- Chen, T., Belladelli, F., Del Giudice, F., & Eisenberg, M. L. (2022). Male fertility as a marker for health. Reproductive Biomedicine Online, 44(1), 131–144. https://doi.org/10.1016/j.rbmo.2021.09.023
- Chen, W., Zou, H., Liu, H., Li, B., & Zhao, J. (2023). Lifestyle: An underrated but potentially important influencing factor on semen quality. Clinical Research Communications, 6(3), 17. https://doi.org/10.53388/CRC2023017
- Conceição, C., Pedro, J., & Martins, M. V. (2017). Effectiveness of a video intervention on fertility knowledge among university students: A randomised pre-test/post-test study. The European Journal of Contraception & Reproductive Health Care, 22(2), 107–113. https://doi.org/10.1080/13625187.2017.1288903
- Daniluk, J. C., & Koert, E. (2015). Fertility awareness online: The efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Human Reproduction, 30(2), 353–363. https://doi.org/10.1093/humrep/deu328
- Daniluk, J. C., Koert, E., & Cheung, A. (2012). Childless women’s knowledge of fertility and assisted human reproduction: Identifying the gaps. Fertility and Sterility, 97(2), 420–426. https://doi.org/10.1016/j.fertnstert.2011.11.046
- Daumler, D., Chan, P., Lo, K. C., Takefman, J., & Zelkowitz, P. (2016). Men’s knowledge of their own fertility: A population-based survey examining the awareness of factors that are associated with male infertility. Human Reproduction, 31(12), 2781–2790. https://doi.org/10.1093/humrep/dew265
- Eisenberg, M. L., Esteves, S. C., Lamb, D. J., Hotaling, J. M., Giwercman, A., Hwang, K., & Cheng, Y. S. (2023). Male infertility. Nature Reviews Disease Primers, 9(1), 49. https://doi.org/10.1038/s41572-023-00459-w
- Finelli, R., Mottola, F., & Agarwal, A. (2021). Impact of alcohol consumption on male fertility potential: A narrative review. International Journal of Environmental Research and Public Health, 19(1), 328. https://doi.org/10.3390/ijerph19010328
- García, D., Vassena, R., Prat, A., & Vernaeve, V. (2016). Increasing fertility knowledge and awareness by tailored education: A randomized controlled trial. Reproductive Biomedicine Online, 32(1), 113–120. https://doi.org/10.1016/j.rbmo.2015.10.008
- Halleran, M., Chernoff, A., & Gordon, J. L. (2022). Fertility knowledge among women struggling to conceive without medical intervention: A brief report. Frontiers in Global Women’s Health, 3, 828052. https://doi.org/10.3389/fgwh.2022.828052
- Hammarberg, K., Zosel, R., Comoy, C., Robertson, S., Holden, C., Deeks, M., & Johnson, L. (2017). Fertility-related knowledge and information-seeking behaviour among people of reproductive age: A qualitative study. Human Fertility, 20(2), 88–95. https://doi.org/10.1080/14647273.2016.1245447
- Harrison, C., Greves, G., Barnard, E., Davies, A., McEleny, K., Gordon, U., Lucky, M., Woodward, B., Pacey, A., Heatley, M., & Boivin, J. (2023). The effect of an educational animation on knowledge of testicular health and fertility of adolescents. Human Reproduction, 38(12), 2470–2477. https://doi.org/10.1093/humrep/dead195
- Hviid Malling, G. M., Schmidt, L., Pitsillos, T., Hammarberg, K., Tydén, T., Friberg, B., Jensen, I., & Ziebe, S. (2022). Taking fertility for granted – A qualitative exploration of fertility awareness among young, childless men in Denmark and Sweden. Human Fertility, 25(2), 1–12. https://doi.org/10.1080/14647273.2020.1798516
- Kovac, J. R., Khanna, A., & Lipshultz, L. I. (2015). The effects of cigarette smoking on male fertility. Postgraduate Medicine, 127(3), 338–341. https://doi.org/10.1080/00325481.2015.1015928
- Kruglova, K., Gelgoot, E. N., Chan, P., Lo, K., Rosberger, Z., Bélanger, E., Kazdan, J., Robins, S., & Zelkowitz, P. (2021). Risky business: Increasing fertility knowledge of men in the general public using the mobile health application infotility XY. American Journal of Men’s Health, 15(5), 15579883211049027. https://doi.org/10.1177/15579883211049027
- Levine, H., Jørgensen, N., Martino-Andrade, A., Mendiola, J., Weksler-Derri, D., Jolles, M., Pinotti, R., & Swan, S. H. (2023). Temporal trends in sperm count: A systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Human Reproduction Update, 29(2), 157–176. https://doi.org/10.1093/humupd/dmac035
- Maeda, E., Boivin, J., Toyokawa, S., Murata, K., & Saito, H. (2018). Two-year follow-up of a randomized controlled trial: Knowledge and reproductive outcome after online fertility education. Human Reproduction, 33(11), 2035–2042. https://doi.org/10.1093/humrep/dey293
- Maeda, E., Miyata, A., Boivin, J., Nomura, K., Kumazawa, Y., Shirasawa, H., Saito, H., & Terada, Y. (2020). Promoting fertility awareness and preconception health using a chatbot: A randomized controlled trial. Reproductive Biomedicine Online, 41(6), 1133–1143. https://doi.org/10.1016/j.rbmo.2020.09.006
- Maeda, E., Nakamura, F., Kobayashi, Y., Boivin, J., Sugimori, H., Murata, K., & Saito, H. (2016). Effects of fertility education on knowledge, desires and anxiety among the reproductive-aged population: Findings from a randomized controlled trial. Human Reproduction, 31(9), 2051–2060. https://doi.org/10.1093/humrep/dew133
- Mahey, R., Gupta, M., Kandpal, S., Malhotra, N., Vanamail, P., Singh, N., & Kriplani, A. (2018). Fertility awareness and knowledge among Indian women attending an infertility clinic: A cross-sectional study. BMC Women’s Health, 18(1), 177. https://doi.org/10.1186/s12905-018-0669-y
- Majumdar, S. S., & Bhattacharya, I. (2013). Genomic and post-genomic leads toward regulation of spermatogenesis. Progress in Biophysics and Molecular Biology, 113(3), 409–422. https://doi.org/10.1016/j.pbiomolbio.2013.01.002
- Mannucci, A., Argento, F. R., Fini, E., Coccia, M. E., Taddei, N., Becatti, M., & Fiorillo, C. (2021). The impact of oxidative stress in male infertility. Frontiers in Molecular Biosciences, 8, 799294. https://doi.org/10.3389/fmolb.2021.799294
- Mansor, N., Ahmad, N., & Rahman, H. A. (2020). Determinants of knowledge on sexually transmitted infections among students in public higher education institutions in Melaka state, Malaysia. PLoS One, 15(10), e0240842. https://doi.org/10.1371/journal.pone.0240842
- McDonagh, M., Peterson, K., Raina, P., et al. Avoiding bias in selecting studies. 2013 Feb 20. In: Methods guide for effectiveness and comparative effectiveness reviews [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK126701/
- Mon Kyaw Soe, N., Bird, Y., Schwandt, M., & Moraros, J. (2018). STI health disparities: A systematic review and meta-analysis of the effectiveness of preventive interventions in educational settings. International Journal of Environmental Research and Public Health, 15(12), 2819. https://doi.org/10.3390/ijerph15122819
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Paganella, M. P., da Motta, L. R., Adami, A. G., Sperhacke, R. D., Kato, S. K., & Pereira, G. F. M. (2021). Knowledge about sexually transmitted infections among young men presenting to the Brazilian Army, 2016: A STROBE-compliant national survey-based cross-sectional observational study. Medicine, 100(22), e26060. https://doi.org/10.1097/MD.0000000000026060
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research ed.), 372, n71. https://doi.org/10.1136/bmj.n71
- Pedro, J., Brandão, T., Schmidt, L., Costa, M. E., & Martins, M. V. (2018). What do people know about fertility? A systematic review on fertility awareness and its associated factors. Upsala Journal of Medical Sciences, 123(2), 71–81. https://doi.org/10.1080/03009734.2018.1480186
- Stentz, N. C., Koelper, N., Barnhart, K. T., Sammel, M. D., & Senapati, S. (2020). Infertility and mortality. American Journal of Obstetrics and Gynecology, 222(3), 251.e251–251.e210. https://doi.org/10.1016/j.ajog.2019.09.007
- Stern, J., Larsson, M., Kristiansson, P., & Tydén, T. (2013). Introducing reproductive life plan-based information in contraceptive counselling: An RCT. Human Reproduction, 28(9), 2450–2461. https://doi.org/10.1093/humrep/det279
- Sterne, J. A. C., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A.-W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. T. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919. https://doi.org/10.1136/bmj.i4919
- Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (Clinical Research ed.), 366, l4898. https://doi.org/10.1136/bmj.l4898
- Thomson, A. A., Brown, M., Zhang, S., Stern, E., Hahn, P. M., & Reid, R. L. (2016). Evaluating acquisition of knowledge about infertility using a whiteboard video. Journal of Obstetrics and Gynaecology Canada: JOGC = Journal D'obstetrique et Gynecologie du Canada: JOGC, 38(7), 646–650. https://doi.org/10.1016/j.jogc.2016.03.010
- Tran, K. T. D., Valli-Pulaski, H., Colvin, A., & Orwig, K. E. (2022). Male fertility preservation and restoration strategies for patients undergoing gonadotoxic therapies†. Biology of Reproduction, 107(2), 382–405. https://doi.org/10.1093/biolre/ioac072
- Walsh, T. J. (2011). Male reproductive health and prostate cancer risk. Current Opinion in Urology, 21(6), 506–513. https://doi.org/10.1097/MOU.0b013e32834bdf14
- Williamson, L. E., Lawson, K. L., Downe, P. J., & Pierson, R. A. (2014). Informed reproductive decision-making: The impact of providing fertility information on fertility knowledge and intentions to delay childbearing. Journal of Obstetrics and Gynaecology Canada: JOGC = Journal D'obstetrique et Gynecologie du Canada: JOGC, 36(5), 400–405. https://doi.org/10.1016/S1701-2163(15)30585-5
- World Health Organization. (2021). WHO fact sheet on infertility. Global Reproductive Health, 6(1), e52–e52. https://doi.org/10.1097/GRH.0000000000000052