Abstract
Purpose
This study evaluates the effect of cochlear implantation (CI) on work ability. The influences of quality of life (QOL), age, mental health, and hearing were analyzed.
Methods
Seventy-nine patients undergoing CI surgery were evaluated preoperatively and 12 months postoperatively. Work ability was evaluated using the Work Ability Index (WAI). QOL was assessed with the Nijmegen Cochlear Implant Questionnaire (NCIQ) and the WHOQOL-BREF. Mental health was assessed with the Patient Health Questionnaire.
Results
The WAI was unaffected by CI (Δ 0.8 ± 6.8, p = 0.42). No significant changes in WAI were observed for employees (Δ – 1.1 ± 5.7, p = 0.25) and pensioners (Δ −0.4 ± 7.8, p = 0.73). Patients without elevated depressiveness, stress, or somatoform symptoms had significantly better WAI.
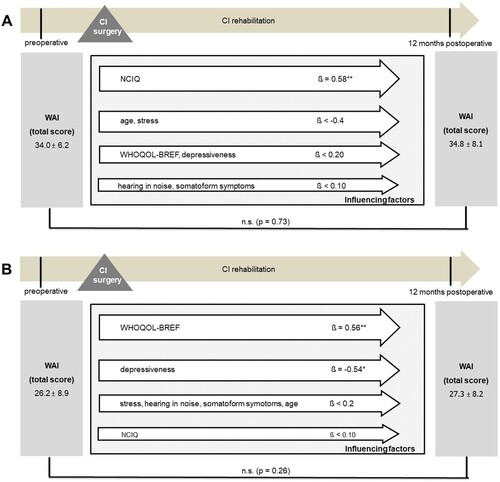
The multiple regression analyses show that WHOQOL-BREF (ß = 0.49, p ≤ 0.001), age (ß = −0.34, p ≤ 0.001), and depressiveness (ß = 0.33, p = 0.04) were significantly associated with WAI. In the employee group, the NCIQ (ß = 0.58, p = 0.008) had the strongest association with the WAI.
Conclusion
Age, mental health, and QOL are predictive factors for work ability. This should be considered in the consultation and the rehabilitation process.
1. Introduction
Currently, the global costs associated with unemployment and early retirement for people with hearing loss are conservatively estimated at $182.5 billion annually (Chadha et al., Citation2021). Due to the demographic shift in the German public, it can be presumed that the economic burden will increase with an aging population. A European study contextualized the relationship between chronic health problems and selection in the workforce, explaining that healthy applicants are more likely to be employed than job candidates with ill health, such as hearing disabilities (Schuring et al., Citation2007). Regardless of the extent of hearing loss, its impact on working life is mainly determined by the efficiency of clinical and rehabilitative interventions (Bolaños-Díaz & Calderón-Cahua, Citation2014; Chadha et al., Citation2021; Wilson et al., Citation2017). As stated in recent research, cochlear implant (CI) treatment increases employment opportunities, career prospects, executive functions, and job satisfaction (Fazel & Gray, Citation2007; Sarant et al., Citation2020). Additionally, the economic benefits of regaining hearing abilities with CI should not be underestimated. According to Clinkard et al., CI users displayed an increase in income more than 6 years postoperatively (Clinkard et al., Citation2015). The same study demonstrated that CI treatment is not only associated with patients’ personal gain but also has a broader economic benefit for society (Clinkard et al., Citation2015).
However, reaching conclusions about individual work ability solely based on functional parameters and how they are influenced by an intervention (e.g. exclusively based on hearing loss and its rehabilitation) does not fully consider the complex construct of work ability. Ilmarinen and Tempel understand work ability as the sum of factors enabling someone in a specific work situation to successfully cope with the work tasks assigned to them (Arbeitsfähigkeit 2010 was können wir tun, damit Sie gesund bleiben?, Citation2002). The Work Ability Index (WAI) was developed in the 1980s as a job-related measure considering the self-assessed work ability in relation to the physical and mental demands of the job as well as the employee’s health and resources (Tuomi et al., Citation1998) to make work ability measurable and thus comparable.
This validated measurement instrument is widely used internationally to address health economic or occupational health issues (Ilmarinen et al., Citation1991; Nygård et al., Citation1991; Tuomi et al., Citation1991). In some studies, the measuring instrument was also used to analyze the impact of specific diseases on the ability to work or the influence of interventions (Chang et al., Citation2020; Tański et al., Citation2022). For individual diseases, individual significant factors influencing the ability to work could be identified using this measurement instrument. In addition to purely functional parameters (Nygård et al., Citation1991), individual well-being and mental health are increasingly becoming the foci of these examinations (Ahlstrom et al., Citation2010; van den Berg et al., Citation2008). Various studies have evaluated the correlation between work ability and quality of life in diverse patient groups, such as those with rheumatoid arthritis (Tański et al., Citation2022) or musculoskeletal disorders (Chang et al., Citation2020; Monteiro et al., Citation2009; van den Berg et al., Citation2008). These studies determined a strong correlation between quality of life (QOL) and work ability. Furthermore, other studies demonstrated a strong association between work ability and physical and social health (Ahlstrom et al., Citation2010; Mateo-Rodríguez et al., Citation2021). Mental comorbidities have been identified as a strong predictor of lower-rated work ability. Depressive and somatoform disorders displayed a strong association with low work ability (Gilmour & Patten, Citation2007). Based on recent studies, not only is work impairment associated with depression and somatoform disorders, but stress also apparently correlates with a working disability (Ervasti et al., Citation2017; Khavanin et al., Citation2018).
Especially in the group of hearing-impaired people, a strong relationship between mental health and working ability can be assumed. The association between mental disorders and hearing loss has been a growing research topic, with multiple studies demonstrating that the prevalence of mental illnesses is higher in hearing-impaired people than those with normal hearing. Various studies associate hearing loss with a strong presence of depressive symptoms, somatoform disorders, and stress symptoms, as well as social isolation and desolation, which subsequently cause clinical depression and somatoform disorders (Bhatt et al., Citation2017; Brüggemann et al., Citation2017; Maharani et al., Citation2019). Moreover, higher stress levels represent a common mental illness associated with hearing impairment (Maharani et al., Citation2019).
Previous studies imply that adequate hearing rehabilitation, for example, through cochlear implantation in higher-degree hearing loss, leads to improved communication and consequently improved mental health (Brüggemann et al., Citation2017; Olze et al., Citation2022). Minimal research exists on the extent to which cochlear implantation can improve the working ability of postlingually deafened patients. Particularly, no studies exist on potential factors influencing the ability to work in this group of patients. Therefore, our study aimed to prospectively assess the influence of cochlear implantation on work ability. Additionally, potential predictors were determined within the framework of a multivariate analysis. The empirical selection of the factors to be considered (age, mental health, QOL, and hearing status) was based on the above-mentioned literature, considering the correlation and dependency structures identified.
2. Patients and methods
All adult patients scheduled for cochlear implantation from June 2020 to July 2021 were screened for participation in the study. Inclusion criteria were age ≥ 18, full legal capacity, German native speaker, and postlingual deafness. The language status was assessed preoperatively by hearing pedagogy. All patients who did not attend the 12-month appointment were excluded from the study. The first psychometric test battery was administered 1 to 2 weeks before surgery. Audiological testing was an important part of the complex outpatient diagnostic process prior to cochlear implantation in our department. The second measurement including audiological and psychometric measurements was taken at the 12-month visit during regular CI rehabilitation.
Institutional review board approval was obtained by the local ethical review committee (EK-247062020). All patients gave their informed consent. The study was conducted in accordance with the Declaration of Helsinki 1964.
2.1. Test battery
2.1.1. Demographic data
Demographic data was obtained preoperatively during the inpatient admission with an anamnesis questionnaire that enquired about the descriptive characteristics of the patient population: gender, age, medical treatment (if any) for the opposite ear, type of CI, implant company, speech processor, current occupation, duration of hearing loss, and professional degree.
2.1.2. Audiological assessment
A matrix test in noise was used with the Oldenburger sentence test (OLSA) to assess everyday speech comprehension as far as possible. The 50% speech reception threshold (SRT) was determined adaptively with a fixed noise level of 65 dB SPL. Under the presentation condition S0N0, speech and noise were displayed from the front at an angle of 0°. The OLSA was performed preoperatively and postoperatively in the bilateral hearing situation.
2.1.3. Psychometric test battery
Work Ability Index (WAI)
Developed in the 1980s by the Finnish Institute of Occupational Health, the WAI is a validated survey that examines the patient’s subjective work ability, defined as the ratio between the individual’s preconditions (health and resources) and the general work demands (Tuomi et al., Citation1998). Thus, the lower the total WAI score, the greater the discrepancy between the individual’s coping skills and the work requirements.
The WAI comprises seven subdomains (). The sums for each subdomain are added to form the total WAI score between 7 (poor working ability) and 49 (excellent working ability). The total WAI score can be grouped into four WAI categories, which additionally define a preventive strategy to either improve low WAI scores or maintain high WAI scores (). Unemployed participants were asked to correlate their working ability to daily life work (e.g. house, garden, or volunteer work).
Patient Health Questionnaire
Table 1 The subdomains of the WAI
Table 2 The four Work Ability Index (WAI) categories and their preventative strategies
The German version of the Patient Health Questionnaire (PHQ-D) was used to assess psychological health (Gräfe K et al., Citationo. J.). The PHQ-D has been developed to screen for mental disorders in primary care. It is based on diagnostic criteria from the fourth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (Guze, Citation1995).
Depressiveness:
The depression module (PHQ-9) of the PHQ-D is a screening tool used in numerous patient populations to quantify the severity of patient-reported depressive symptoms (‘depressiveness’). Patients rate the occurrence of depressive symptoms within the last 2 weeks on a 4-point scale from 0 (‘not at all’) to 3 (‘nearly every day’). The severity of depressive symptoms was analyzed as a continuous score from 0 (none) to 27 (severe).
Stress:
The PHQ stress module measures psychosocial stress during the last month using 10 items, including health, work/financial, social, and traumatic stress. Patients rate the severity of stress on a scale of 0 (‘not at all bothered’) to 2 (‘bothered a lot’). The severity of stress was analyzed on a continuous scale from 0 (none) to 20 (severe).
Somatoform
The ‘somatoform symptoms’ scale score includes 15 somatic symptoms corresponding to the 15 most common physical complaints of outpatients as well as the most important DSM-IV criteria for somatization disorders. This ‘somatoform module’ is also called ‘PHQ-15.’ The PHQ-15 score is formed from the 13 somatoform module items and 2 depression module items. The somatoform module items are marked with 0 (‘not impaired’), 1 (‘slightly impaired’), or 2 (‘strongly impaired’). The scale sum value thus lies between 0 and 30.
According to the PHQ-D manual, a cutoff value of 5 points can be set for each mental disorder. Therefore, scale values below 5 points indicate that the participants display a lack of depressive symptoms, a lack of somatoform symptoms, and a low stress severity level.
Quality of life
WHOQOL-BREF
The WHOQOL-BREF is an abbreviated version of the original WHO-QOL-100. Developed by the World Health Organization (WHO), the questionnaire was validated and translated into over 30 languages (The WHOQOL Group, Citation1998). The questionnaire comprises four domain scores (physical, psychological, social, and environmental health), each representing one aspect of QOL. The mean scores are converted to a 0–100 scale to create a comparable dataset. The total score is calculated from the mean values of all subscores. Higher scores indicate better generic QOL.
Nijmegen Cochlear Implant Questionnaire
The Nijmegen Cochlear Implant Questionnaire (NCIQ) is specifically designed to evaluate the QOL of CI patients (Hinderink et al., Citation2000). The NCIQ has also been validated in German by (Plath et al., Citation2021). It comprises 60 questions divided into three main domains (physical, mental, and social functionality) and six subdomains (basic sound perception, advanced sound perception, speech production, self-esteem, activity limitations, and social interactions). The total NCIQ score is computed as the mean of the six subdomain averages. A higher score reflects a better subjective assessment of disease-specific QOL.
2.2. Statistical analysis
The statistical evaluation was performed with the software IBM SPSS Statistics, Version 28 (New York, United States of America). Data were shown as mean ± standard deviation (SD). In the presence of a normal distribution, the preoperative and postoperative datasets of working ability and the influencing factors were assessed with paired samples t test. The preoperative and postoperative WAI score differences between two groups were determined solely with the unpaired samples t test. Differences between three groups were analyzed by univariate analysis of variance (ANOVA). Multiple linear regression analyses were conducted to determine the effect of psychological health, QOL, age, and hearing status on outcome scores. Bivariate associations were described using the Pearson correlation coefficient (r). The McNemar-Bowker test was used to analyze the pre-postoperative shift in WAI clusters. The significance level was defined at p < 0.05.
3. Results
A total of 101 potential participants were initially admitted to this study, and 79 patients could be fully evaluated preoperatively as well as postoperatively. Consequently, 22 (21.8%) patients were excluded from the data pool due to incomplete datasets. Eleven patients (10.9%) did not want to retake the psychometric measurements for personal reasons, nine patients (8.9%) did not attend the 12-month appointment due to the COVID-19 pandemic, and in two patients (2.0%), the implant had to be changed due to an implant defect. lists the demographic characteristics of the patient population. Based on the current German retirement age of 67, 68.4% of the study’s participants (n = 54) were of working age, whereas 31.6% (n = 35) were above the working age of 67.
Table 3 Demographic data (n = 79)
3.1. Work ability
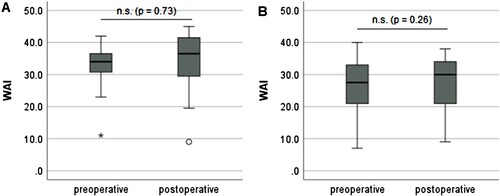
Based on the evaluation of the preoperative (30.2 ± 8.6) and postoperative (31.0 ± 9.1) WAI scores, working ability did not significantly change 12 months after cochlear implantation (Δ 0.8 ± 6.8, p = 0.42, ). Nevertheless, an improvement in the assigned WAI category to a better WAI category after CI surgery was observed in 59.4% (n = 47) of the patients (). However, 11.4% (n = 9) of patients reported a worsening in the WAI category 12 months after cochlear implantation. This frequency change in the WAI classes is significant (p < 0.001).
Figure 1 Comparison of the working ability of all patients (n = 79) before and 12 months after cochlear implantation. Work ability is measured by the Work Ability Index (WAI). Higher values indicate a better work ability. The results show no significant (n.s.) change after cochlear implantation.
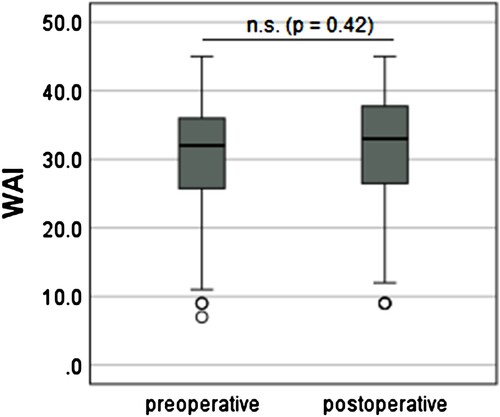
Table 4 Change in Work Ability Index (WAI) clusters pre- to postoperative (p < 0.001). (The patients with an improvement in the WAI cluster are marked in light grey.)
3.2. Potential influencing factors for work ability
3.2.1. Hearing status
The influencing factor speech comprehension in noise, analyzed using the OLSA, showed a significant improvement (Δ −3.1 ± 5.4 dB, p < 0.001) after cochlear implantation (preoperative 3.5 ± 0.9 dB versus postoperative 0.5 ± 0.5 dB). Based on the univariate analysis, no significant association existed between postoperative SRT and WAI score (r = 0.039, p = 0.74).
No significant differences were obtained in the postoperative WAI scores (p = 0.18) stratified for the three types of hearing loss (AHL, SSD, and bilateral hearing). None of these three patient groups showed a significant improvement in work ability after cochlear implantation ().
Table 5 Comparison of pre- and postoperative work ability measures by the Work Ability Index (WAI), stratified by gender, type of hearing loss, psychological comorbidity, professional degree, and working status
3.2.2. Age
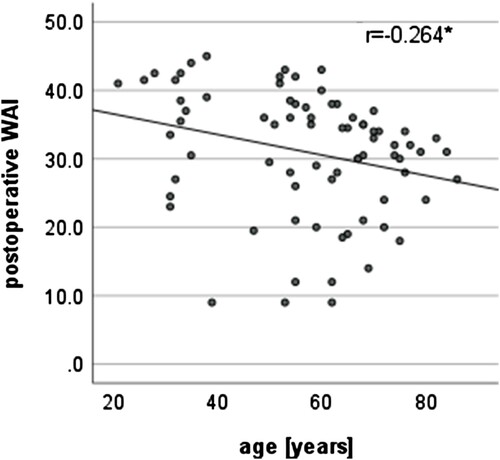
No significant improvement was found in the WAI score in either age group (patients <67 and patients ≥ 67 years) analyzed (). When comparing both age groups, no significant difference was found in the postoperative WAI score (p = 0.19). The correlation analysis displayed a low negative association between postoperative working ability and age, demonstrating that the postoperative working ability significantly decreased as age increased (, r = −0.27, p = 0.02).
3.2.3. Quality of life
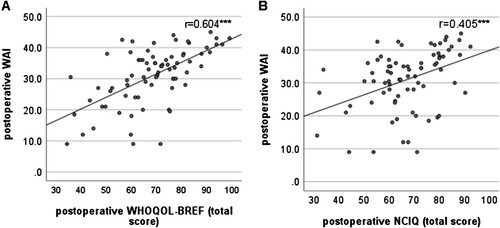
The general QOL measured with the WHOQOL-BREF did not show a significant change 12 months after the CI treatment (68.9 ± 12.6 versus 68.5 ± 14.5 p = 0.72). Based on the univariate analysis, a moderate positive association existed between the postoperative general QOL and postoperative WAI score (A, r = 0.614, p < 0.001). The evaluation of the preoperative and postoperative mean NCIQ total scores displayed a significant improvement (50.1 ± 14.1 versus 67.2 ± 13.6, p < 0.001) 12 months after the CI treatment. A low positive association existed between the postoperative NCIQ total score and WAI score (B, r = 0.41, p < 0.001).
Figure 3 Association of postoperative work ability and (A) postoperative general quality of life (QOL) and (B) disease-specific QOL. Work ability was determined using the Work Ability Index (WAI), general QOL using the WHOQOL-BREF total score and disease-specific QOL using Nijmegen Cochlear Implant Questionnaire (NCIQ), Higher WAI values indicate a better work ability. Higher QOL scores indicate better QOL. ***p < 0.001.
3.2.4. Psychological comorbidities
Regarding PHQ-D scores, no significant change occurred in patients’ depressiveness (5.4 ± 4.3 versus 4.9 ± 3.9, p = 0.12, somatization 6.3 ± 4.8 versus 7.0 ± 4.8, p = 0.08, and stress perception 3.8 ± 3.5 versus 4.1 ± 3.4, p = 0.49) after cochlear implantation. Significant associations existed between these psychological comorbidity scores and postoperative WAI scores (A–C).
Figure 4 (A - C) Correlation of postoperative work ability (expressed by WAI total score) and mental health (depressiveness, stress, somatoform symptoms), (D) comparison of patients with preoperative non-minimal depressive symptoms (PHQ-9 < 5) versus patients with depressive symptoms (PHQ-9 ≥ 5); (E) comparison of patients with minimally pronounced psychosocial stressors (PHQ stress module < 5) versus patients with more pronounced stressors (PHQ stress module ≥ 5); (F) comparison of patients without pronounced somatoform symptoms (PHQ-15 < 5) versus patients with more somatoform symptoms (PHQ-15 ≥ 5); WAI, Work Ability Index, PHQ, Patient Health Questionnaire, Higher WAI values indicate a better work ability. Higher PHQ scores indicate worse mental health. ***p < 0.001, ** p < 0.01, *p ≤ 0.05
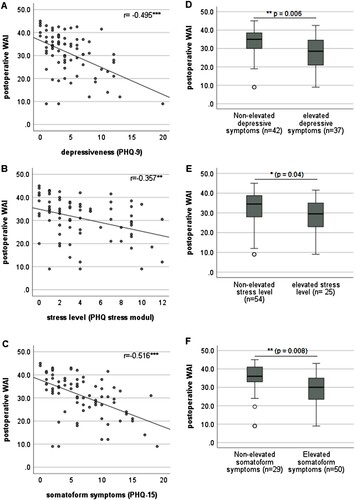
Participants with high stress severity levels, present somatoform symptoms, and relevant depressive symptoms rated their postoperative working ability significantly worse (E–F) than patients with a low stress severity level (Δ 3.9 ± 2.2, p = 0.04) and a lack of somatoform (Δ 5.48 ± 2.01, p = 0.008) or depressive symptoms (Δ 5.73 ± 2.04, p = 0.006).
3.2.5. Working status
Working ability was further analyzed regarding the two predominant occupational subpopulations of this study: employed patients and pensioners (including old age pensioners and disability pensioners). When comparing the postoperative working abilities of employees and pensioners, the analysis revealed a significant difference between the two postoperative WAI scores (p < 0.001, ). However, the analysis of pre- and postoperative WAI scores for both employed and pensioned participants did not show a significant change after the CI treatment (A, employed patients: mean difference −1.1 ± 5.7, p = 0.25, B pensioned participants: mean difference −0.4 ± 7.8, p = 0.73).
Figure 5 Comparison of the working ability of all patients stratified by different working status, (A) employees (n = 39) and (B) pensioners (n = 37), The results show no significant (n.s.) change after cochlear implantation. WAI, Work Ability Index. Higher WAI values indicate a better work ability.
Furthermore, the ability to work was stratified according to the type of professional degree. A distinction was made between patients with a degree from a university or university of applied sciences (n = 32) and patients with vocational training (n = 44). The patients with university degrees tended to show better postoperative work ability than the patient group with vocational training (). However, the difference (Δ 4.0 ± 2.1, p = 0.06) was not significant. No significant improvement in WAI due to cochlear implantation was demonstrated for any of these patient groups.
3.2.6. Multivariate analyses
Multivariate analyses for postoperative WAI were performed with explanatory variables including generic QOL (WHOQOL-BREF total score), disease-specific health-related QOL (NCIQ total score), age, hearing status (OLSA), and psychological comorbidities (stress perception, depressiveness, and somatoform symptoms). The results of the multiple regression analyses showed that in the total patient group, even when adjusting for these factors, generic QOL, age, and depressiveness remained significantly associated with higher WAI scores (). Multivariate analysis was additionally stratified by working status. In the employees’ group (A) the postoperative disease-specific QOL (postoperative NCIQ scores) was the strongest influencing factor. When evaluating the influences of these factors on the postoperative WAI in the pensioner group (B), generic QOL and depressiveness had the strongest influences on WAI when adjusted for the possible influencing factors listed.
Figure 6 Multiple regression analysis of factors influencing postoperative work ability (overall group, n = 79); WAI, Work Ability Index. Mental Health (depressiveness, somatoform symptoms, stress) were evaluated by Patient Health Questionnaire (PHQ-D), general QOL using the WHOQOL-BREF total score and disease-specific QOL using Nijmegen Cochlear Implant Questionnaire (NCIQ), hearing in noise by the Oldenburger sentence test. Data shown are mean ± SD; ß regression coefficient; ***p ≤ 0.001, *p ≤ 0.05, n.s. not significant.
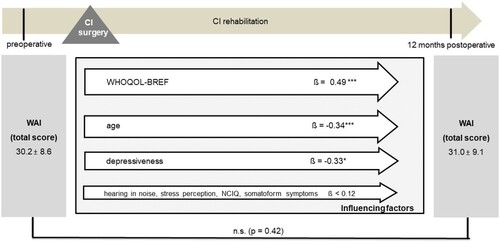
Figure 7 Multiple regression analysis of factors influencing postoperative NCIQ, stratified by working status, (A) employees (n = 39), (B) pensioners (n = 31), WAI, Work Ability Index. Mental Health (depressiveness, somatoform symptoms, stress) were evaluated by Patient Health Questionnaire (PHQ-D), general QOL using the WHOQOL-BREF total score and disease-specific QOL using Nijmegen Cochlear Implant Questionnaire (NCIQ), hearing in noise by the Oldenburger sentence test. Data shown are mean ± SD; ß regression coefficient; ***p ≤ 0.01, *p ≤ 0.05.
4. Discussion
Unaddressed hearing loss can negatively impact many aspects of daily life: communication, the development of language and speech in children, cognition, education, employment, mental health, and interpersonal relationships (Chadha et al., Citation2021). Therefore, it is understandable that hearing disorders can also decisively influence the ability to work of those affected.
Numerous studies have demonstrated the positive effect of cochlear implantation on audiological performance (Daher et al., Citation2023; Ma et al., Citation2023) and QOL, but also on psychological comorbidities (Brüggemann et al., Citation2017; Häußler et al., Citation2020; Ketterer et al., Citation2020; Olze et al., Citation2022). This generated the hypothesis that a cochlear implant can contribute to improved work ability by improving speech comprehension and QOL. To date, only sporadic studies exist on the impact of cochlear implantation on working life (Goh et al., Citation2016). Work ability has not been addressed in a standardized way in these studies so far.
When comparing the mean postoperative WAI with the German public, the patient cohort of this study had an average postoperative WAI score of 31.0 ± 9.1, whereas the German reference group displayed a mean score of 40.2 ± 6.2 (Freyer, Citation2019). Therefore, based on the evaluation with the WAI categories, CI users of our analysis estimated their postoperative work ability only as ‘moderate,’ which appears much lower than that of most Germans who assessed their work ability as ‘good.’ These findings reaffirm the negative correlation between hearing disability and work ability (Gupta et al., Citation2023). Regarding the age distribution of the participants, 68.4% of the patients (n = 54) were of working age between 18 and 67. Consequently, less than one-third of the participants (31.6%, n = 35) were above the German retirement age of 67. However, when analyzing the occupations of the study cohort, less than half of the participants (49.4%, n = 39) were employed, and more than one-third of the patients (39.2%, n = 31) were pensioners. This leads to the conclusion that a substantial discrepancy exists between the number of hearing-impaired participants who should hypothetically be working and the number of people actively employed. Moreover, our study established that work ability did not significantly improve after CI treatment. However, a significant increase in ‘good’ and ‘very good’ work ability postoperatively was discerned when comparing preoperative and postoperative WAI categories. Similar findings were presented in a study from New Zealand, which also identified a positive influence of CI treatment on employment; however, the outcome lacked statistical significance (Goh et al., Citation2016).
Adaptation processes could be one cause of the lack of improvement in the ability to work (Boothroyd, Citation2007). Some of the long-term hearing-impaired patients may have found jobs with lower communication requirements or have developed strategies to cope with the demands of working life despite their hearing loss. It is also notable that, on average, the patients in this study were aged 57.7 ± 16.0. Considering that older people are less likely to acquire new habits and skills, the overall demographic of CI patients could display lower levels of ambition to improve their work ability to attain a promotion or higher job position (Monteiro et al., Citation2009; von Bonsdorff et al., Citation2012). Another reason for the lack of evidence of improvement will be the short follow-up period of 1 year. Health economic studies on measures to improve working ability often show only very small effects after long observation periods (Oakman et al., Citation2018).
Consistent with studies from other medical fields, our study also showed a significant association of QOL with work ability (Chang et al., Citation2020; Tański et al., Citation2022). While the disease-specific QOL primarily influenced the ability to work in our group of employed people, the general QOL was decisive for assessing the ability to work in the group of pensioners. Notably, at this point, a bidirectional relationship can be assumed between the factors QOL and work ability, which should be analyzed in more detail in further studies. Speech comprehension did not correlate with work ability in our study. This is consistent with other studies, which also showed no correlation of hearing with the patient-reported outcome measures (Capretta & Moberly, Citation2016; Lailach et al., Citation2018, Citation2021; Vasil et al., Citation2020). Mental health was found to be another important factor influencing the ability to work in our study. Patients with increased depressiveness, increased expression of somatoform symptoms, and high stress perception showed a significantly poorer ability to work. In our multivariate analysis, the significant influence remained in the total group and the group of pensioners, even after adjustment for the other potential influencing factors. In our study, 46.8% of the patients had relevant depressive symptoms. The high rate of depressive symptoms in hearing-impaired people has been documented in previous studies. Earlier studies showed depression rates of 40%–60% in hearing-impaired people or a rate almost five times higher than the general population (Knutson & Lansing, Citation1990; Sherbourne et al., Citation2002; Thomas, Citation1984). In our study, 31.6% reported increased stress levels, representing only a slight increase compared to the general European population during the COVID-19 pandemic (27.41%) (Mahmud et al., Citation2021). In our study, 50 out of 79 patients (63%) had somatoform symptoms. Meta-analyses have found a lifetime prevalence of 40% for somatoform disorders (Haller et al., Citation2015). Our study thus indicates an increased prevalence of somatoform disorders in patients with profound hearing loss.
Overall, the results of our study suggest that the purposeful modulation of mental comorbidities during CI (re)habilitation can lead to an improvement in work ability after CI treatment. In addition to screening and primary psychological counseling as part of CI (re)habilitation, additional psychotherapy is recommended for patients with psychological comorbidities. It is therefore crucial to incorporate psychological and psychosomatic guidance during CI (re)habilitation to comprehensively promote and maintain work ability after CI treatment (Brüggemann et al., Citation2017). The expansion of the therapy spectrum and multiprofessionality, including psychological support, is now established in many centers to fully consider the biopsychosocial concept (Tucker et al., Citation2011). Psychological counseling and guidance throughout the CI rehabilitation process significantly influence the patient’s motivation and basic attitude towards therapeutic work as well as hearing impairment generally. Moreover, hearing-impaired people benefit tremendously from workplace accommodations and welfare to promote their work ability (Hua et al., Citation2015; Svinndal et al., Citation2018). It is therefore essential to incorporate these services during CI (re)habilitation to develop strategies for job modifications and inclusivity at the workplace for patients adapting to CI. CI (re)habilitation should also include a psychosocial approach to overcome present stigmas and teach CI users psychological facilitators for work life with a CI. This would expedite the transition from working with hearing impairment to restored hearing abilities with the CI and could simultaneously maximize the improvement in the patients’ work ability.
An important consideration is that the COVID-19 pandemic has created profound changes in work life, reshaping how people work, communicate, and collaborate. One of the most notable shifts during the pandemic was the rapid adoption of remote work. Furthermore, the pandemic accelerated the digital transformation in the workplace. Companies that had previously relied heavily on in-person interactions were forced to rapidly adapt to the digital landscape (Galanti et al., Citation2021). These changes, along with smaller work groups and progressively important mail traffic, could have unintentionally improved the work ability of hearing-impaired people.
The outcome parameter of this study was evaluated with the WAI questionnaire, which is not specifically designed for assessing the work ability of hearing-impaired people. This can also lead to low responsiveness. Likewise, pensioners were evaluated with the WAI rather than using a questionnaire focusing on evaluating work ability specifically for pensioners. Consequently, a questionnaire evaluating disease-specific work ability for CI users for different age groups could enhance the assessment of the outcome parameter of this study and emphasize the differential influences of various work ability parameters between pensioned and employed CI patients. Additionally, the WHOQOL-BREF was used for all age groups. The additional use of the WHOQOL-OLD would have led to an additional time burden for the elderly patients.
The present study explored factors influencing the ability to work in CI patients, which are known from other areas of medicine, for the first time. However, further disease-specific and non-disease-specific factors are required when considering the complex construct of work ability. For example, the effect of tinnitus and dizziness on work ability should be analyzed. Furthermore, factors such as coping strategies, work environment, work community, management, values, attitudes, motivation, competences, and work experiences should be assessed. Furthermore, the operational environment (e.g. social networks, infrastructure, and labor market) should be integrated into the assessment of work ability (Ilmarinen, Citation2009, Citation2019; Ilmarinen et al., Citation2005). Additionally, it must be considered that an inhomogeneous patient group was analyzed in the current study. The patients showed inhomogeneity in hearing situation, age, and occupational status. However, splitting the total group into small subgroups showed significant differences only for the two occupational groups (employers/pensioners). Work ability assessment in a larger homogeneous group would be desirable. This explorative study can provide a basis for this.
5. Conclusion
Cochlear implantation does not improve work ability after 12 months. Patients undergoing CI treatment should receive preliminary counseling to inform them about realistic expectations. The development of strategies to help patients with CI improve their ability to work is urgently needed. Additionally, among the covariates, mental health and QOL were salient factors associated with work ability. Health promotion programs to improve the mental health of CI patients could be another means to increase their work ability.
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest None.
Ethical standards All procedures performed in studies involving human participants were in accordance with the ethical standards of local ethical review committee (EK 166042017) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all the participants.
Data availability statement The data that support the findings of this study are available on request from the corresponding author (SL).
Additional information
Notes on contributors
Susen Lailach
Susen Lailach is a specialist physician for otorhinolaryngology and phoniatrics and pediatric audiology at the ORL-HNS Department of the University Hospital Dresden.
Johanna Martin
Johanna Martin graduated in dentistry, a PhD student at the ORL-HNS Department of the University Hospital Dresden.
Paula Stephan
Paula Stephan graduated in dentistry, a PhD student at the ORL-HNS Department of the University Hospital Dresden.
Dominique Kronesser
Dominique Kronesser is a Speech and Language Therapist (M. A.) and therapeutic director of the Saxonian Cochlear Implant Centre Dresden.
Thomas Zahnert
Thomas Zahnert since 2004 he has been the director of the ORL-HNS Department of the University Hospital Dresden.
Marcus Neudert
Marcus Neudert is a medical director of the Ear Research Center in Dresden (ERCD) and a senior physician at the ORL-HNS Department of the University Hospital Dresden.
References
- Ahlstrom, L., Grimby-Ekman, A., Hagberg, M., Dellve, L. 2010. The work ability index and single-item question: associations with sick leave, symptoms, and health–a prospective study of women on long-term sick leave. Scandinavian Journal of Work, Environment & Health, 36(5): 404–412. doi:10.5271/sjweh.2917.
- Arbeitsfähigkeit 2010 was können wir tun, damit Sie gesund bleiben? 2002. VSA-Verl. https://d-nb.info/963477366/04.
- Bhatt, J.M., Bhattacharyya, N., Lin, H.W. 2017. Relationships between tinnitus and the prevalence of anxiety and depression. The Laryngoscope, 127(2): 466–469. doi:10.1002/lary.26107.
- Bolaños-Díaz, R., Calderón-Cahua, M. 2014. Cefprozil versus amoxicillin/clavulanate for the treatment of acute otitis media in children: meta-analysis of efficacy and safety. Pharmacology & Pharmacy, 5(4): Article 4. doi:10.4236/pp.2014.54046.
- Boothroyd, A. 2007. Adult aural rehabilitation: what is it and does it work? Trends in Amplification, 11(2): 63–71. doi:10.1177/1084713807301073.
- Brüggemann, P., Szczepek, A.J., Klee, K., Gräbel, S., Mazurek, B., Olze, H. 2017. In patients undergoing cochlear implantation, psychological burden affects tinnitus and the overall outcome of auditory rehabilitation. Frontiers in Human Neuroscience, 11: 226. doi:10.3389/fnhum.2017.00226.
- Capretta, N.R., Moberly, A.C. 2016. Does quality of life depend on speech recognition performance for adult cochlear implant users? The Laryngoscope, 126(3): 699–706. doi:10.1002/lary.25525.
- Chadha, S., Kamenov, K., Cieza, A. 2021. The world report on hearing, 2021. Bulletin of the World Health Organization, 99(4): 242–242A. doi:10.2471/BLT.21.285643.
- Chang, Y.-F., Yeh, C.-M., Huang, S.-L., Ho, C.-C., Li, R.-H., Wang, W.-H., Tang, F.-C. 2020. Work ability and quality of life in patients with work-related musculoskeletal disorders. International Journal of Environmental Research and Public Health, 17(9): 3310. doi:10.3390/ijerph17093310.
- Clinkard, D., Barbic, S., Amoodi, H., Shipp, D., Lin, V. 2015. The economic and societal benefits of adult cochlear implant implantation: a pilot exploratory study. Cochlear Implants International, 16(4): 181–185. doi:10.1179/1754762814Y.0000000096.
- Daher, G.S., Kocharyan, A., Dillon, M.T., Carlson, M.L. 2023. Cochlear implantation outcomes in adults With single-sided deafness: a systematic review and meta-analysis. Otology & Neurotology, 44(4): 297–309. doi:10.1097/MAO.0000000000003833.
- Ervasti, J., Joensuu, M., Pentti, J., Oksanen, T., Ahola, K., Vahtera, J., et al. 2017. Prognostic factors for return to work after depression-related work disability: a systematic review and meta-analysis. Journal of Psychiatric Research, 95: 28–36. doi:10.1016/j.jpsychires.2017.07.024.
- Fazel, M.Z., Gray, R.F. 2007. Patient employment status and satisfaction following cochlear implantation. Cochlear Implants International, 8(2): 87–91. doi:10.1179/cim.2007.8.2.87.
- Freyer, M. 2019. Eine Konstruktvalidierung des Work Ability Index anhand einer repräsentativen Stichprobe von Erwerbstätigen in Deutschland. doi:10.21934/BAUA:BERICHT20190529.
- Galanti, T., Guidetti, G., Mazzei, E., Zappalà, S., Toscano, F. 2021. Work from home during the COVID-19 outbreak: the impact on employees’ remote work productivity, engagement, and stress. Journal of Occupational and Environmental Medicine, 63(7): e426–e432. doi:10.1097/JOM.0000000000002236.
- Gilmour, H., Patten, S.B. 2007. Depression and work impairment. Health Reports, 18(1): 9–22.
- Goh, T., Bird, P., Pearson, J., Mustard, J. 2016. Educational, employment, and social participation of young adult graduates from the paediatric southern cochlear implant programme, New Zealand. Cochlear Implants International, 17(1): 31–51. doi:10.1179/1754762815Y.0000000018.
- Gräfe, K., Zipfel, S., Herzog, W., Löwe, B. o. J. Screening psychischer Störungen mit dem Gesundheitsfragebogen für Patienten (PHQ-D). 50, 171–181.
- Gupta, S., Jaiswal, A., Sukhai, M., Wittich, W. 2023. Hearing disability and employment: a population-based analysis using the 2017 Canadian survey on disability. Disability and Rehabilitation, 45(11): 1836–1846. doi:10.1080/09638288.2022.2076938.
- Guze, S.B. 1995. Diagnostic and statistical manual of mental disorders, 4th ed. (DSM-IV). American Journal of Psychiatry, 152(8): 1228–1228. doi:10.1176/ajp.152.8.1228.
- Haller, H., Cramer, H., Lauche, R., Dobos, G. 2015. Somatoforme störungen und medizinisch unerklärbare symptome in der primärversorgung. Deutsches Ärzteblatt International, 112(16): 279–287.
- Häußler, S.M., Köpke, V., Knopke, S., Gräbel, S., Olze, H. 2020. Multifactorial positive influence of cochlear implantation on patients with single-sided deafness. The Laryngoscope, 130(2): 500–506. doi:10.1002/lary.28007.
- Hinderink, J.B., Krabbe, P.F., Van Den Broek, P. 2000. Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngology–Head and Neck Surgery, 123(6): 756–765. doi:10.1067/mhn.2000.108203.
- Hua, H., Anderzén-Carlsson, A., Widén, S., Lyxell, B. 2015. Conceptions of working life among employees with mild-moderate aided hearing impairment: a phenomenographic study. International Journal of Audiology, 54(11): 873–880. doi:10.3109/14992027.2015.1060640.
- Ilmarinen, J. 2009. Work ability—A comprehensive concept for occupational health research and prevention. Scandinavian Journal of Work, Environment & Health, 35(1): 1–5.
- Ilmarinen, J. 2019. From work ability research to implementation. International Journal of Environmental Research and Public Health, 16(16): 2882. doi:10.3390/ijerph16162882.
- Ilmarinen, J., Tuomi, K., Eskelinen, L., Nygård, C.H., Huuhtanen, P., Klockars, M. 1991. Summary and recommendations of a project involving cross-sectional and follow-up studies on the aging worker in Finnish municipal occupations (1981-1985). Scandinavian Journal of Work, Environment & Health, 17(Suppl 1): 135–141.
- Ilmarinen, J., Tuomi, K., Seitsamo, J. 2005. New dimensions of work ability. International Congress Series, 1280: 3–7. doi:10.1016/j.ics.2005.02.060.
- Ketterer, M.C., Häussler, S.-M., Hildenbrand, T., Speck, I., Peus, D., Rosner, B., et al. 2020. Binaural hearing rehabilitation improves speech perception, quality of life, tinnitus distress, and psychological comorbidities. Otology & Neurotology, 41(5): e563–e574. doi:10.1097/MAO.0000000000002590.
- Khavanin, A., Malakouti, J., Gharibi, V., Khanjani, N., Mokarami, H., Ebrahimi, M.H. 2018. Using work ability index and work-related stress to evaluate the physical and mental fitness of Iranian telecom tower climbers. Journal of Injury & Violence Research, 10(2): 105–112. doi:10.5249/jivr.v10i2.996.
- Knutson, J.F., Lansing, C.R. 1990. The relationship between communication problems and psychological difficulties in persons with profound acquired hearing loss. The Journal of Speech and Hearing Disorders, 55(4): 656–664. doi:10.1044/jshd.5504.656.
- Lailach, S., Langanke, T., Zahnert, T., Garthus-Niegel, S., Neudert, M. 2021. Impact of depressive disorders on quality of life after middle ear surgery in patients with chronic otitis media. European Archives of Oto-Rhino-Laryngology, 278(9): 3217–3225. doi:10.1007/s00405-020-06397-7.
- Lailach, S., Schenke, T., Baumann, I., Walter, H., Praetorius, M., Beleites, T., et al. 2018. Living with otosclerosis: disease-specific health-related quality-of-life measurement in patients undergoing stapes surgery. European Archives of Oto-Rhino-Laryngology, 275(1): 71–79. doi:10.1007/s00405-017-4798-y.
- Ma, C., Fried, J., Nguyen, S.A., Schvartz-Leyzac, K.C., Camposeo, E.L., Meyer, T.A., et al. 2023. Longitudinal speech recognition changes after cochlear implant: systematic review and meta-analysis. The Laryngoscope, 133(5): 1014–1024. doi:10.1002/lary.30354.
- Maharani, A., Pendleton, N., Leroi, I. 2019. Hearing impairment, loneliness, social isolation, and cognitive function: longitudinal analysis using English longitudinal study on ageing. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 27(12): 1348–1356. doi:10.1016/j.jagp.2019.07.010.
- Mahmud, S., Hossain, S., Muyeed, A., Islam, M.M., Mohsin, M. 2021. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: a rapid systematic review and meta-analysis. Heliyon, 7(7): e07393. doi:10.1016/j.heliyon.2021.e07393.
- Mateo-Rodríguez, I., Knox, E., Daponte-Codina, A., esTAR group. 2021. Factors associated with workability in spanish health centre workers. Occupational Medicine (Oxford, England), 71(1): 12–19. doi:10.1093/occmed/kqaa206.
- Monteiro, M.S., Alexandre, N.M.C., Ilmarinen, J., Rodrigues, C.M. 2009. Work ability and musculoskeletal disorders among workers from a public health institution. International Journal of Occupational Safety and Ergonomics: JOSE, 15(3): 319–324. doi:10.1080/10803548.2009.11076813.
- Nygård, C.H., Eskelinen, L., Suvanto, S., Tuomi, K., Ilmarinen, J. 1991. Associations between functional capacity and work ability among elderly municipal employees. Scandinavian Journal of Work, Environment & Health, 17(Suppl 1): 122–127.
- Oakman, J., Neupane, S., Proper, K.I., Kinsman, N., Nygård, C.-H. 2018. Workplace interventions to improve work ability: a systematic review and meta-analysis of their effectiveness. Scandinavian Journal of Work, Environment & Health, 44(2): 134–146. doi:10.5271/sjweh.3685.
- Olze, H., Ketterer, M.C., Péus, D., Häußler, S.M., Hildebrandt, L., Gräbel, S., Szczepek, A.J. 2022. Effects of auditory rehabilitation with cochlear implant on tinnitus prevalence and distress, health-related quality of life, subjective hearing and psychological comorbidities: comparative analysis of patients with asymmetric hearing loss (AHL), double-sided (bilateral) deafness (DSD), and single-sided (unilateral) deafness (SSD). Frontiers in Neurology, 13: 1089610. doi:10.3389/fneur.2022.1089610.
- Plath, M., Sand, M., van de Weyer, P.S., Baierl, K., Praetorius, M., Plinkert, P.K., et al. 2021. [Validity and reliability of the Nijmegen Cochlear Implant Questionnaire in German]. HNO. doi:10.1007/s00106-021-01114-0.
- Sarant, J., Harris, D., Busby, P., Maruff, P., Schembri, A., Lemke, U., Launer, S. 2020. The effect of hearing aid use on cognition in older adults: can we delay decline or even improve cognitive function? Journal of Clinical Medicine, 9(1): 254. doi:10.3390/jcm9010254.
- Schuring, M., Burdorf, L., Kunst, A., Mackenbach, J. 2007. The effects of ill health on entering and maintaining paid employment: evidence in European countries. Journal of Epidemiology and Community Health, 61(7): 597–604. doi:10.1136/jech.2006.047456.
- Sherbourne, K., White, L., Fortnuni, H. 2002. Intensive rehabilitation programmes for deafened men and women: an evaluation study. International Journal of Audiology, 41(3): 195–201. doi:10.3109/14992020209077183.
- Svinndal, E.V., Solheim, J., Rise, M.B., Jensen, C. 2018. Hearing loss and work participation: a cross-sectional study in Norway. International Journal of Audiology, 57(9): 646–656. doi:10.1080/14992027.2018.1464216.
- Tański, W., Dudek, K., Adamowski, T. 2022. Work ability and quality of life in patients with rheumatoid arthritis. International Journal of Environmental Research and Public Health, 19(20): 13260. doi:10.3390/ijerph192013260.
- Thomas, A.J. 1984. Acquired hearing loss: psychological and psychosocial implications. London: Academic Press.
- Tucker, D., Compton, M., Mankoff, L., Rulison, K. 2011. Cochlear implant connections: a biopsychosocial audiologic rehabilitation program for late-deafened adults With cochlear implants. Perspectives on Aural Rehabilitation and Its Instrumentation, 18: 23. doi:10.1044/arii18.1.23.
- Tuomi, K., Ilmarinen, J., Eskelinen, L., Järvinen, E., Toikkanen, J., Klockars, M. 1991. Prevalence and incidence rates of diseases and work ability in different work categories of municipal occupations. Scandinavian Journal of Work, Environment & Health, 17(Suppl 1): 67–74.
- Tuomi, K., Ilmarinen, J., Jahkola, A., Katajarinne, L., Tulkki, A. 1998. Work ability index (Bd. 19). Helsinki: Finnish Institute of Occupational Health.
- van den Berg, T.I.J., Alavinia, S.M., Bredt, F.J., Lindeboom, D., Elders, L.a.M., Burdorf, A. 2008. The influence of psychosocial factors at work and life style on health and work ability among professional workers. International Archives of Occupational and Environmental Health, 81(8): 1029–1036. doi:10.1007/s00420-007-0296-7.
- Vasil, K.J., Lewis, J., Tamati, T., Ray, C., Moberly, A.C. 2020. How does quality of life relate to auditory abilities? A subitem analysis of the Nijmegen cochlear implant questionnaire. Journal of the American Academy of Audiology, 31(4): 292–301. doi:10.3766/jaaa.19047.
- von Bonsdorff, M.B., Seitsamo, J., Ilmarinen, J., Nygård, C.-H., von Bonsdorff, M.E., Rantanen, T. 2012. Work ability as a determinant of old age disability severity: evidence from the 28-year Finnish longitudinal study on municipal employees. Aging Clinical and Experimental Research, 24(4): 354–360. doi:10.3275/8107.
- The WHOQOL Group. 1998. Development of the world health organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3): 551–558. doi:10.1017/s0033291798006667.
- Wilson, B.S., Tucci, D.L., Merson, M.H., O’Donoghue, G.M. 2017. Global hearing health care: new findings and perspectives. Lancet (London, England), 390(10111): 2503–2515. doi:10.1016/S0140-6736(17)31073-5.