Abstract
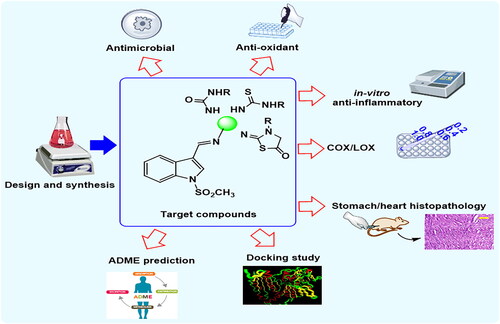
Three novel series of N-methylsulfonylindole derivatives 3a&b, 4a–e, and 5a–e were synthesised. Different biological activities of the synthesised compounds were studied. Antimicrobial activity showed that, compounds 4b, 4e and 5d had selective antibacterial activity against the Gram-negative bacteria, Salmonella enterica and/or E. coli. The anti-oxidant activity of the synthesised compounds was evaluated by DPPH radical scavenging activity. In vitro anti-inflammatory activity was estimated. Compounds 4d, 4e, 5b, and 5d showed the highest anti-inflammatory activity. The COX-1, COX-2 and 5-LOX inhibitory activities were measured using enzyme immune assay (EIA) kits. Due to the dual COX-2/5-LOX inhibitory activity of compound 5d, its cardiovascular profile was determined by measuring cardiac biomarkers (LDH, CK-MB, and Tn-I). Besides, the histopathological study of the heart muscle and stomach were examined for the most active COX-2 inhibitors 4e and 5d. Finally, a molecular modelling study and pharmacokinetic properties were obtained using different computational methods.
Introduction
Pathogens, damaged cells and irritants are harmful stimuli that lead the body to make a complex response known as inflammationCitation1,Citation2.
Inflammation is important for the tissue repair process, but in the case of its chronic form, it causes negative effects on the body. Anti-inflammatory agents aim to relieve inflammatory symptoms such as pain, redness, heat and swellingCitation3,Citation4.
Non-steroidal anti-inflammatory drugs (NSAIDs) are the most common method of treatment of inflammatory symptoms. They act through inhibition of biotransformation of arachidonic acid (AA), a membrane bound phospholipid, to prostaglandins (PGs), prostacyclines (PGI2) and thromboxane A2 (TXA2) by the action of cyclooxygenase (COX) enzymes (COX-1, 2, 3)Citation5–7. COX-pathway inhibition leads to unwanted side effects such as ulcerogenicity, hepatic and renal toxicity, which have arisen due to COX-1 inhibitors and cardiovascular disorders caused by COX-2 inhibitors. Both NSAIDs that could inhibit both COX-1 and COX-2 enzymes, such as aspirin, phenazone and indomethacin, (), as well as selective COX-2 inhibitors, especially like, roficoxib and valdecoxib, () can increase the cardiovascular risks specially in patients with pre-existing cardiovascular disease. This can be caused by the imbalance in PGI2 (potent vasodilator and antithrombotic)/TXA2 (prothrombotic) ratio. Consequently, most drugs have been used in a restricted manner or even withdrawn from the marketCitation8–10. This leads to a search for new compounds that act in another way to metabolise AA. Liopoxygenase (LOX) enzymes (5-, 8-, 12- and 15-LOX) convert AA to leucotrienes. 5-LOX is the one associated with inflammation, bronchoconstriction, allergy and asthmaCitation11–13.
As a result, designing new compounds with dual COX-2/5-LOX inhibitory activity might solve the problem by offering new options for developing anti-inflammatory agents with the advantages of selective COX-2 inhibition and at the same time have better cardioprotective profileCitation2,Citation14,Citation15.
Several biomarkers were reported to be used for the assessment of heart function such as sera containing aspartate aminotransferase (AST), alkaline phosphatase (ALP), lactate dehydrogenase (LDH), troponin (Tn-I) and creatine kinase-MB (CK-MB) in addition to tumour necrosis factor-α (TNF-α), a key player in the inflammatory response and cardiac depression, interleukin-6 (IL-6) and interleukin-1β (IL-1β) as the decrease in their level indicates low risk of cardiovascular toxicityCitation16–18.
Besides, tissue including glutathione (GSH) acts as an anti-oxidant in cardiac tissue. It was reported that chronic administration of celecoxib resulted in an increase in lipid peroxidation via elevation of oxidative stress markers, which in turn increases oxidative kidney damage, leading to a decrease in GSH levelCitation19.
Moreover, one of the most important issues related to inflammation is with bacterial infections, which can be considered a primary cause of inflammation area as well as a second complication due to the accumulation of fluid inside the injured areaCitation20.
Resistance is a serious medical problem that has been observed in the currently used antibacterial agents. It makes the treatment of infectious diseases very difficult. So, the discovery of novel antibacterial agents might be the best way to overcome this episodeCitation21,Citation22.
Celecoxib, (), the drug of choice as a COX-2 inhibitor, was investigated as an antimicrobial agent as well. It showed potent effects in the reversal of multidrug resistance in MRSA, besides the increased sensitivity of M. smegmatis and S. aureus to antibioticsCitation23.
Another way that affects inflammation is the free radical formation which causes cell damage and inflammation. So, anti-oxidant agents are taken side by side with anti-inflammatory drugs in most casesCitation24,Citation25.
Searching the literature, it was found that indole is a nucleus of choice as a multi-target scaffold for the treatment of inflammation besides its antimicrobial and anti-oxidant activitiesCitation26–29.
This lead scaffold is a universal constituent in pharmacologically active natural products as well as synthetic drugsCitation30.
Thus, indole thiosemicarbazide derivatives showed both anticancer and anti-oxidant activityCitation26, indole alkaloids obtained from Alstonia scholaris and Topsentia sponge showed antibacterial activityCitation4,Citation31. Indomethacin, the indole derivative, is considered one of the most promising synthetic drugs as an anti-inflammatory and analgesic agentsCitation8.
Moreover, it was reported that the indole-thiazolidinone hybrid, (), showed equal potency as antimicrobial and antifungal activity (MIC <0.98 µg/ml) if compared to standard drug ciprofloxacin (MIC <3.90 µg/ml)Citation27. Additionally, N-arylsulfonyl indoles, (), exerted remarkable inhibitory activity against Gram-Positive bacteria including multidrug resistance clinical isolatesCitation21.
On the other hand, carbazones (semi/thiosemi), (), are reported to have potential biological activities as antiviral, antimycobacterial, antitrypanosomal, anticonvulsant, antituberculosis, anticancer, anti-inflammatory, antimicrobial, and anti-oxidantCitation29,Citation31–35.
Taking into consideration the various reported biological activities associated with indole, carbazones, and thiazolidinone skeletons, it was worth incorporating these moieties together in a single frame “privileged medicinal scaffolds” to obtain a more potent and biologically active multi-target drug with fewer side effects and a high safety profile.
The design of our newly suggested compounds using the active multi-target drug strategy, (), depends on; (i) the main scaffold is indole as indomethacin, the lead compound, (ii) COX-2 pharmacophore, SO2Me, from rofecoxib structure, (iii) electron donating substituent on p-position of the phenyl ring, to mimic celecoxib, the selective COX-2 inhibitor drug, (iv) introducing carbazone (semi/thiosemi) moieties with reported anti-inflammatory, anti-oxidant and antimicrobial activities on indole C-3, (v) merging thiazolidinone ring with indole scaffold comes from 5-LOX inhibitors drabufelone and tenidap, respectivelyCitation3.
The structure and stereochemical configuration of three series of target compounds 3&b, 4a–e and 5a–e were confirmed. In vitro anti-inflammatory activities through the determination of TNF-α inhibition in RAW264.7 macrophages, COX-1/2 and 5-LOX inhibitory activities were evaluated. The gastrointestinal and cardiovascular evaluation was determined. The plausible binding interactions inside COX-2 and 5-LOX active sites were explored using a molecular modelling study. Moreover, anti-oxidant and antimicrobial activities were investigated. Finally, ADME prediction and drug-likeness parameters were investigated.
Experimental
Chemistry
Melting points were determined using the Griffin apparatus and were uncorrected. Values of IR spectra were measured using Shimadzu IR-435 spectrophotometer with KBr discs and represented in cm−1. 1H NMR and 13C NMR were carried out using the Bruker instrument at 400 MHz for 1H NMR and 100 MHz for 13C NMR spectrophotometer, (Faculty of Pharmacy, Beni-Suef University, Beni-Suef, Egypt), in DMSO-d6 (as a solvent), D2O using TMS as an internal standard and chemical shifts were recorded in ppm on the δ scale using DMSO-d6 (2.5) as a solvent. Coupling constant (J) values were estimated at Hertz (Hz). Splitting patterns were designated as follows: s, singlet; d, doublet, t, triplet; q, quartette; m, multiplet. Hewlett Packard 5988 spectrometer (Palo Alto, CA) was used to record the electron impact (EI) mass spectra (Microanalytical centre, Cairo University). Microanalysis was performed for C, H, and N on Perkin-Elmer 2400 at the Microanalytical Centre, Cairo University, Egypt and was within ±0.4% of theoretical values. Analytical thin-layer chromatography (TLC), pre-coated plastic sheets, 0.2 mm silica gel with UV indicator (Macherey-Nagel) was employed routinely to follow the course of reactions and to check the purity of products. All other reagents, solvents and compound 1 were purchased from the Aldrich Chemical Company (Milwaukee, WI) and were used without further purification.
General method for preparation of compounds 3a&b and 4a-e
A mixture of indole derivative 2 (2.23 g, 0.01 mol) and the appropriate semicarbazone or thiosemicarbazone derivative (0.01 mol) in absolute ethanol (20 ml) containing drops of DMF, was heated under reflux for 2–4 h. The obtained solid was filtered, dried, and crystallised from 95% of ethanol to give compounds 3a&b and 4a-e.
(E)-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}hydrazinecarboxamide (3a)
Yield 79%; white crystals; mp 238–240ᵒC; IR. (cm−1): 3404–3122 (NH2 and NH), 3122 (NH), 1696 (C = O), 1227, 1165 (SO2); 1H NMR (DMSO-d6) δ 3.49 (s, 3H, SO2CH3), 6.40 (s, 2H, NH2, D2O exchangeable), 7.37–7.48 (m, 2H, indole H-5, H-6), 7.87 (d, J = 8.0 Hz, 1H, indole H-7), 7.97 (s, 1H, indole H-2), 8.11 (s, 1H, N = CH), 8.35 (d, J = 7.6 Hz, 1H, indole H-4), 10.22 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 41.51 (SO2CH3), 113.25, 117.51, 123.57, 124.39, 125.87, 127.07, 128.87, 135.37, 135.46, 157.10 (C = O); Anal. Calcd for C11H12N4O3S (280.06): C, 47.13; H, 4.32; N, 19.99. Found: C, 47.44; H, 4.07; N, 19.82.
(E)-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}-N-phenylhydrazinecarboxamide (3b)
Yield 72%; white crystals; mp 234–236ᵒC; IR. (cm−1): 3219 and 3123 (2NH), 1673 (C = O), 1238, 1166 (SO2); 1H NMR (DMSO-d6) δ 3.52 (s, 3H, SO2CH3), 6.94–6.98 (m, 3H, phenyl H-3, H-4, H-5), 7.24–7.28 (m, 2H, indole H-5, H-6), 7.31 (d, J = 7.6 Hz, 2H, phenyl H-2, H-6), 7.50 (d, J = 8.0 Hz, 1H, indole H-7), 8.11 (s, 1H, indole H-2), 8.23 (d, J = 8.0 Hz, 1H, indole H-4), 8.70 (s, 1H, N = CH), 9.77 (s, 1H, NH, D2O exchangeable), 10.67 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 41.81 (SO2CH3), 113.54, 117.18, 118.95, 120.23, 122.33, 123.14, 124.59, 125.94, 127.17, 129.16, 135.42, 136.59, 140.15, 156.50 (C = O); EIMS (m/z): 356.98 (M+, 35.15%), 192.46 (100.00%); Anal. Calcd for C17H16N4O3S (356.40): C, 57.29; H, 4.52; N, 15.72. Found: C, 57.46; H, 4.37; N, 15.68.
(E)-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}-hydrazine-1-carbothioamide (4a)
Yield 82%; white crystals; mp 178–180ᵒC; IR. (cm−1): 3435 and 3324 (NH2), 3171 (NH), 1230, 1166 (SO2), 1129 (C = S); 1H NMR (DMSO-d6) δ 3.52 (s, 3H, SO2CH3), 7.37–7.49 (m, 2H, indole H-5, H-6), 7.65 (s, 1H, NH, D2O exchangeable), 7.87 (d, J = 8.4 Hz, 1H, indole H-7), 8.22 (s, 1H, indole H-2), 8.32 (s, 2H, NH2, D2O exchangeable), 8.37 (s, 1H, N = CH), 8.39 (d, J = 7.6 Hz, 1H, indole H-4), 11.43 (s, 1H, SH, D2O exchangeable); 13C NMR (DMSO-d6) δ 41.63 (SO2CH3), 113.25, 116.80, 123.72, 124.50, 126.00, 126.78, 130.55, 135.41, 138.71, 177.94 (C = S); Anal. Calcd for C11H12N4O2S2 (296.37): C, 44.58; H, 4.08; N, 18.90. Found: C, 44.75; H, 3.89; N, 19.13.
(E)-N-Ethyl-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}-hydrazinecarbothioamide (4b)
Yield 73%; white fluffy crystals; mp 240–242ᵒC; IR. (cm−1): 3278 and 3149 (2NH), 1306, 1207 (SO2), 1058 (C = S); 1H NMR (DMSO-d6) δ 1.18 (t, J = 7.6 Hz, 3H, CH2CH3), 3.56 (s, 3H, SO2CH3), 3.69 (q, J = 7.6 Hz, 2H, CH2CH3), 7.41–7.50 (m, 3H, indole H-5, H-6 and NH, D2O exchangeable), 7.88 (d, J = 8.0 Hz, 1H, indole H-7), 8.18 (d, J = 7.6 Hz, 1H, indole H-4), 8.22 (s, 1H, indole H-2), 8.35 (s, 1H, N = CH), 11.40 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 15.17 (CH3), 38.91 (CH2), 41.64 (SO2CH3), 113.33, 116.81, 123.37, 124.47, 126.00, 126.88, 130.10, 135.39, 138.11, 176.88 (C = S); Anal. Calcd for C13H16N4O2S2 (324.42): C, 48.13; H, 4.97; N, 17.27. Found: C, 48.44; H, 5.09; N, 17.31.
(E)-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}-N-phenylhydrazinecarbothioamide (4c)
Yield 79%; white crystals; mp 220–222ᵒC; IR. (cm−1): 3333 and 3122 (2NH), 1270, 1198 (SO2), 1129 (C = S); 1H NMR (DMSO-d6) δ 3.51 (s, 3H, SO2CH3), 7.23–7.40 (m, 5H, indole H-5, H-6 and phenyl H-3, H-4, H-5), 7.44 (d, J = 8.4 Hz, 2H, phenyl H-2, H-6), 7.61 (d, J = 7.2 Hz, 1H, indole H-7), 8.21 (s, 1H, indole H-2), 8.35 (d, J = 7.6 Hz, 1H, indole H-4), 8.45 (s, 1H, N = CH), 9.80 (s, 1H, NH, D2O exchangeable), 11.78 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 41.69 (SO2CH3), 113.36, 116.65, 123.22, 124.47, 125.78, 126.00, 126.20, 126.98, 128.36, 130.43, 135.38, 138.87, 139.71, 176.18 (C = S); Anal. Calcd for C17H16N4O2S2 (372.07): C, 54.82; H, 4.33; N, 15.04. Found: C, 54.56; H, 4.19; N, 14.89.
(E)-2{[1-(methylsulfonyl)-1H-indol-3yl]methylene}-N-(p-tolyl)hydrazinecarbothioamide (4d)
Yield 81%; white crystals; mp 237–239ᵒC; IR. (cm−1): 3341 and 3129 (2NH), 1200, 1163 (SO2), 1127 (C = S); 1H NMR (DMSO-d6) δ 3.33 (s, 3H, CH3), 3.54 (s, 3H, SO2CH3), 7.19 (d, J = 8.4 Hz, 2H, p-tolyl H-3, H-5), 7.39–7.47 (m, 4H, indole H-5, H-6 and p-tolyl H-2, H-6), 7.89 (d, J = 8.0 Hz, 1H, indole H-7), 8.20 (s, 1H, indole H-2), 8.34 (d, J = 7.6 Hz, 1H, indole H-4), 8.43 (s, 1H, N = CH), 9.75 (s, 1H, NH, D2O exchangeable), 11.75 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 21.07 (CH3), 41.68 (SO2CH3), 113.36, 116.67, 123.18, 124.46, 126.00, 126.24, 126.99, 129.10, 130.31, 135.02, 135.37, 137.12, 138.69, 176.26 (C = S); EIMS (m/z): 386.60 (M+, 42.55%), 261.41 (100.00%); Anal. Calcd for C18H18N4O2S2 (386.09): C, 55.94; H, 4.69; N, 14.50. Found: C, 56.16; H, 4.78; N, 14.23.
(E)-N-(4-Methoxyphenyl)-2{[1-(methylsulfonyl)-1H-indol 3yl]methylene}hydrazinecarbothioamide (4e)
Yield 80%; white crystals; mp 214–216ᵒC; IR. (cm−1): 3431 (broad, 2NH), 1248, 1167 (SO2), 1127 (C = S); 1H NMR (DMSO-d6) δ 3.54 (s, 3H, SO2CH3), 3.78 (s, 3H, OCH3), 6.95 (d, J = 8.8 Hz, 2H, p-methoxyphenyl H-3, H-5), 7.39–7.42 (m, 4H, indole H-5, H-6 and p-methoxyphenyl H-2, H-6), 7.44 (d, J = 8.0 Hz, 1H, indole H-7), 8.89 (s, 1H, indole H-2), 8.36 (d, J = 7.6 Hz, 1H, indole H-4), 8.43 (s, 1H, N = CH), 9.69 (s, 1H, NH, D2O exchangeable), 11.74 (s, 1H, NH, D2O exchangeable); 13C NMR (DMSO-d6) δ 41.68 (SO2CH3), 55.70 (OCH3), 113.34, 113.82, 116.70, 123.26, 124.43, 125.98, 127.00, 128.10, 130.25, 132.61, 135.37, 138.58, 157.50, 176.61 (C = S); Anal. Calcd for C18H18N4O3S2 (402.08): C, 53.71; H, 4.51; N, 13.92. Found: C, 53.98; H, 4.65; N, 13.73.
General method for preparation of compounds 5a–e
A mixture of the appropriate indole derivative 4a–e (0.0025 mol), ethyl chloroacetate (0.30 g, 0.0025 mol), and sodium acetate (0.82 g, 0.01 mol) in absolute ethanol (20 ml) containing drops of DMF, was heated under reflux for 4–6 h. The obtained solid was filtered, dried, and crystallised from 95% of ethanol to give compounds 5a–e.
(E)-2-(E)-{[1-(methylsulfonyl)-1H-indol-3yl)methylene]hydrazono}thiazolidin-5-one (5a)
Yield 72%; white crystals; mp >300ᵒC; IR. (cm−1): 3429 (NH), 1712 (C = O), 1255, 1172 (SO2); 1H NMR (DMSO-d6) δ 3.55 (s, 3H, SO2CH3), 3.93 (s, 2H, CH2), 7.42–7.51 (m, 3H, indole H-5, H-6 and NH, D2O exchangeable), 7.90 (d, J = 8.0 Hz, 1H, indole H-7), 8.15 (s, 1H, indole H-2), 8.36 (d, J = 8.4 Hz, 1H, indole H-4), 8.63 (s, 1H, N = CH); 13C NMR (DMSO-d6) δ 33.53 (CH2), 41.71 (SO2CH3), 113.50, 117.32, 123.50, 124.59, 126.10, 127.25, 131.77, 135.51, 151.43, 164.07, 172.52 (C = O); Anal. Calcd for C13H12N4O3S2 (336.04): C, 46.42; H, 3.60; N, 16.66. Found: C, 46.28; H, 3.46; N, 16.37.
(E)-3-Ethyl-2-(E)-{[1-(methylsulfonyl)-1H-indol-3yl)methylene]hydrazono}thiazolidin-5-one (5b)
Yield 68%; white crystals; mp 230–232ᵒC; IR. (cm−1): 1715 (C = O), 1239, 1166 (SO2); 1H NMR (DMSO-d6) δ 1.19 (t, J = 7.2 Hz, 3H, CH2CH3), 3.59 (s, 3H, SO2CH3), 3.78 (q, J = 7.2 Hz, 2H, CH2CH3), 4.01 (s, 2H, CH2), 7.42–7.52 (m, 2H, indole H-5, H-6), 7.90 (d, J = 7.2 Hz, 1H, indole H-7), 8.17 (s, 1H, indole H-2), 8.38 (d, J = 7.6 Hz, 1H, indole H-4), 8.69 (s, 1H, N = CH); 13C NMR (DMSO-d6) δ 12.85 (CH2CH3), 32.66 (CH2), 38.26 (CH2CH3), 41.74 (SO2CH3), 113.53, 117.21, 123.46, 124.64, 126.13, 127.22, 131.99, 135.52, 152.55, 164.07, 172.52 (C = O); EIMS (m/z): 364.65 (M+, 18.87%), 173.17 (100.00%); Anal. Calcd for C15H16N4O3S2 (364.07): C, 49.43; H, 4.43; N, 15.37. Found: C, 49.22; H, 4.66; N, 15.09.
(E)-2-(E)-{[1-(methylsulfonyl)-1H-indol-3yl)methylene]hydrazono}-3-phenylthiazolidin-5-one (5c)
Yield 79%; white crystals; mp 260–262ᵒC; IR. (cm−1): 1620 (C = O), 1242, 1165 (SO2); 1H NMR (DMSO-d6) δ 3.56 (s, 3H, SO2CH3), 4.12 (s, 2H, CH2), 7.41–7.56 (m, 7H, indole H-5, H-6 and phenyl H-2, H-3, H-4, H-5, H-6), 7.90 (d, J = 8.0 Hz, 1H, indole H-7), 8.06 (s, 1H, indole H-2), 8.42 (d, J = 8.4 Hz, 1H, indole H-4), 8.53 (s, 1H, N = CH); 13C NMR (DMSO-d6) δ 32.83 (CH2), 41.75 (SO2CH3), 111.94, 113.34, 123.42, 126.13, 127.18, 128.58, 128.75, 129.13, 129.60, 131.96, 134.50, 135.50, 141.58, 152.45, 172.51 (C = O); Anal. Calcd for C19H16N4O3S2 (412.07): C, 55.32; H, 3.91; N, 13.58. Found: C, 55.53; H, 4.17; N, 13.87.
(E)-2-(E)-{[1-(methylsulfonyl)-1H-indol-3yl)methylene]hydrazono}-3-(p-tolyl)phenylhiazolidin-5-one (5d)
Yield 76%; white crystals; mp 271–273ᵒC; IR. (cm−1): 1621 (C = O), 1241, 1164 (SO2); 1H NMR (DMSO-d6) δ 2.39 (s, 3H, CH3), 3.55 (s, 3H, SO2CH3), 4.12 (s, 2H, CH2), 7.28 (d, J = 8.4 Hz, 2H, p-tolyl H-3, H-5), 7.32 (d, J = 8.4 Hz, 2H, p-tolyl H-2, H-6), 7.45–7.50 (m, 2H, indole H-5, H-6), 7.89 (d, J = 8.0 Hz, 1H, indole H-7), 8.09 (s, 1H, indole H-2), 8.39 (d, J = 8.0 Hz, 1H, indole H-4), 8.51 (s, 1H, N = CH); 13C NMR (DMSO-d6) δ 21.23 (CH3), 32.59 (CH2), 42.03 (SO2CH3), 113.38, 117.08, 123.45, 126.13, 127.12, 128.49, 130.16, 132.00, 132.83, 135.33, 138.74, 149.81, 152.69, 165.40, 172.45 (C = O); Anal. Calcd for C20H18N4O3S2 (426.08): C, 56.32; H, 4.25; N, 13.14. Found: C, 56.18; H, 4.36; N, 12.89.
(E)-3–(4-Methoxyphenyl)-2-(E)-{[1-(methylsulfonyl)-1H-indol-3yl)methylene]hydrazono}-hiazolidin-5-one (5e)
Yield 74%; white crystals; mp 273–275ᵒC; IR. (cm−1): 1620 (C = O), 1248, 1166 (SO2); 1H NMR (DMSO-d6) δ 3.56 (s, 3H, SO2CH3), 3.83 (s, 3H, OCH3), 4.12 (s, 2H, CH2), 7.33 (d, J = 8.8 Hz, 2H, p-methoxyphenyl H-3, H-5), 7.44 (d, J = 8.8 Hz, 2H, p-methoxyphenyl H-2, H-6), 7.47–7.52 (m, 2H, indole H-5, H-6), 7.90 (d, J = 7.6 Hz, 1H, indole H-7), 8.10 (s, 1H, indole H-2), 8.41 (d, J = 7.2 Hz, 1H, indole H-4), 8.53 (s, 1H, N = CH); 13C NMR (DMSO-d6) δ 32.71 (CH2), 41.74 (SO2CH3), 55.89 (OCH3), 113.53, 114.80, 117.17, 123.47, 124.65, 126.12, 127.20, 128.12, 129.84, 131.95, 135.49, 152.64, 159.66, 165.55, 172.69 (C = O); Anal. Calcd for C20H18N4O4S2 (442.08): C, 54.28; H, 4.10; N, 12.66. Found: C, 54.49; H, 4.37; N, 12.46.
Biological evaluation
Antimicrobial activity screening
All compounds were screened for their antimicrobial activity at the Microbiology and Immunology Department, Faculty of Pharmacy, Beni-Suef University. The antimicrobial activity screening was carried out using the disc diffusion method, as described earlierCitation36–38, with some adjustments.
The compounds were evaluated for their bioactivity against the Gram-positive bacteria, Staphylococcus aureus (ATCC 43300), Listeria monocytogenes (ATCC 7644) and Enterococcus faecalis V853, as well as the Gram-negative bacteria, Escherichia coli (E. coli) (ATCC 25922), Pseudomonas aeruginosa (ATCC 27853) and Salmonella enterica (ATCC 14028) in addition to the yeast, Candida albicans (ATCC 60193).
For each indicator microbe, a solution of half McFarland turbidity was prepared in sterile saline, followed by surface streaking of the strains on Mueller-Hinton agar with a sterile cotton swab. Then, sterile filter paper discs (5 mm diameter) preloaded with 100 µg of each compound were applied to the surface of the pre-inoculated plates. Then, the plates were chilled at 4 °C for 100 min before being incubated overnight at the proper temperature for microbial growth. Finally, the diameter of the inhibition zones around each disc was measured to evaluate the antimicrobial activity of the compounds. Ciprofloxacin was used as a standard antibacterial agent at a concentration of 20 µg/disc. Furthermore, DMSO-loaded discs were used as a negative control.
Anti-oxidant activity
Preparation of samples was occurred at the following concentrations: Samples 3a, 4a, 5b, 5d and 5e at final concentrations of 0.5 mg/ml in methanol: DMSO 9:1 v/v. Samples 4b and 4d at final concentrations 0.025 mg/ml in methanol: DMSO 9:1 v/v, sample 5a at final concentrations 0.25 mg/ml in methanol: DMSO 9:1 v/v, Sample 4c, 5c and 4e at final concentrations 0.05 mg/ml in methanol: DMSO 9:1 v/v, sample 3b at final concentration 0.75 mg/ml methanol: DMSO 9:1 v/v. A stock solution of 100 µM concentration of Trolox, a standard used in this experiment, was prepared in methanol from which seven concentrations were prepared, including 50, 40, 30, 20, 15, 10 and 5 µM.
The DPPH (2,2-diphenyl-1-picryl-hydrazyl-hydrate) free radical assay was carried out according to the method of Boly et al. 2016Citation39. Briefly, freshly prepared DPPH reagent (100 µl, 0.1% in methanol) was added to 100 µl of the sample on 96 well plates (n = 6). The reaction was incubated at room temp for 30 min in the dark. After completion of the incubation time, the reduction in DPPH colour intensity was measured at 540 nm. Data obtained was represented as means ± SD, according to the following equation, percentage inhibition = [(Average absorbance of blank – average absorbance of the test)/(Average absorbance of blank)] *100. The results were recorded using a microplate reader, FluoStar Omega.
Microsoft Excel® was used to analyse the obtained results. The IC50 values were calculated using Graph pad Prism 6® by converting the concentrations to their logarithmic value and selecting the non-linear inhibitor regression equation (log (inhibitor) vs. normalised response – variable slope equation). The methods used and the final test report (R-SO7320) were obtained from Nawah Scientific.
Anti-inflammatory activity
Measurements of TNF-α in RAW264.7 macrophage cells
Reagents and chemicals
Both Lipopolysaccharides (LPS) and hispidin were purchased from Sigma (Sigma-Aldrich, St. Louis, MO, USA)Citation40. The foetal bovine serum (FBS) and Dulbecco’s modified Eagle’s medium (DMEM) were purchased from Hyclone (General Electric Healthcare Life Sciences, Mississauga, Canada), penicillin streptomycin (P/S) was purchased from Solarbio (Solarbio life sciences, Beijing, P. R. China). Results of all in vitro anti-inflammatory screening were obtained from the confirmatory diagnostic unit, VACSERA, Egypt.
Cell culture
DMEM was used to cultivate the macrophage cells RAW264.7 (Shanghai BOGO Industrial Co., Ltd., Shanghai, China), and supplemented with 10% FBS and 1% P/S (100 U/ml and 100 mg/ml, respectively). The cells were maintained in DMEM at 37 °C and 5% CO2. They were treated with various concentrations of hispidin, then with 1 μg/ml LPS for the indicated time.
Cell viability assay
The RAW264.7 macrophage cells were seeded into 96 well plates at a concentration of 4 × 103 cells per well, with different concentrations (100 to 0.4 μg/ml) of hispidin treated 24 h. In the next step, to each well, a solution of 5 mg/ml 3–(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT; Sigma-Aldrich,) was added and incubated (37 °C, 5% CO2) for 4 h. After that, the supernatant was removed and DMSO was added to dissolve formazan. Finally, the absorbance was measured at 490 nm using a UV MAX and kinetic microplate reader (Molecular Devices, LLC).
Preparation of reverse transcription quantitative PCR (RT-qPCR) -ready cell lysates
PBS (1 ml/well) was used to wash the cells in 24-well plates. Then, cell monolayers were exposed to 200 ml/well of Bio-Rad iScript (Bio-Rad SPR; 170–8898) to prepare cell lysates (cell-Lysis, CL). The final formulation of CL buffer consisted of 10 mM Tris-HCl, pH 7.4, 0.25% Igepal CA-630, and 150 mM NaCl. CL Buffer was freshly prepared from the following stock solutions: 1 M Tris-HCl (T2194; Sigma), 10% Igepal CA-630 (I8896; Sigma); and 5 M NaCl (351–036-100; Quality Biological, Inc.). For the experiments, CL Buffer included MgCl2 (M1028; Sigma) or RNasin Plus RNase Inhibitor (N2615; Promega). Before use, both Bio-Rad SPR and CL buffer were equilibrated to room temperature. Cells were exposed for 2 min to Bio-Rad SPR and 5 min to CL buffer. Carefully, the resulting lysates were collected and either analysed immediately or stored frozen (220 or 280uC).
Reverse transcription quantitative PCR (RT-qPCR) gene expression
RT-qPCR analysis was performed in one-step SYBR Green RT-qPCR. Each reaction contained: 1 ml of cell lysate, iScript One-Step SYBR Green RT-PCR Supermix (170–8893; Bio-Rad), 600 nM of each primer, and nuclease-free water to 10 ml. A CFX96 real-time PCR instrument (Bio-Rad) was used under the following protocol: 50uC for 10 min, 95uC for 5 min, 95uC for 10 s/61uC for 15 s/72uC for 30 s.
After the 72 °C extension step, data collection occurred. Total RNA purified from cells was used as an RT-qPCR quantification standard.
In vitro cyclooxygenase (COX-1 and COX-2)
Enzyme immune assay (EIA) kits (Catalog no. K548-100, Cayman Chemical, Ann Arbour, MI) were used to test the ability of the prepared compounds to specifically inhibit ovine COX-1 and COX-2 (IC50 value, µM), according to reported methodsCitation41–43. The COX-2 S.I. values were calculated from the ratio (COX-1 IC50)/(COX-2 IC50) and compared with that of celecoxib, as a selective COX-2 inhibitor.
In vitro lipoxygenase (5-LOX) inhibition assay
The ability of the test compounds to inhibit the 5-LOX enzyme (IC50 value, μM) was detected using the Cayman Human Lipoxygenase Inhibitor Screening Assay (EIA) kit (catalog no. K980-100, Cayman Chemical). The IC50 values of test compounds were measured in µM according to the manufacturer’s instructions and reported methodCitation43.
Evaluation of ulcerogenic effect
Ulcerogenic liability
Chemicals, kits, celecoxib, and indomethacin were purchased from Sigma-Aldrich (St. Louis, MO, USA). CK-MB, Troponin-I, and LDH were purchased from Thermo Fisher Scientific (USA).
Animal and ethics statement
In this study, adult male Wister albino rats weighing 160–180 g were used. Before any experimental procedure, rats were given 14 days to acclimate. These rats were maintained in a controlled setting with food and water available. All experiments were conducted in accordance with laboratory animal care guidelines. All experimental procedures were carried out in accordance with the regulations of the Committee of Ethics for Scientific Research on Living Organisms, Faculty of Pharmacy, Nahda University, Beni-Suef (NUB). The approval number was (NUB-019–025).
Ulcerogenic liability
Ulcerogenic susceptibility was assessed for the most selected candidates (5b and 4e) and compared to indomethacin using celecoxib as a standard. Before drug administration, rats were fasted for 18 h and then separated into four groups. The control group received a suspension of the vehicle (10% DMSO in saline was given P.O (100 mg/kg) once daily). Other groups were given candidates, celecoxib, and indomethacin, in accordance with the described methodologyCitation44. Rats were given the required dose for three consecutive days. Following the last dose, the stomachs of each rat were dissected and opened via the greater curvature and rinsed with saline. For investigation, the dissected stomach was stretched with pins on a cork board. Through illuminated magnifying lenses, the stomach mucosa was examined for the existence of ulcers. Cho and Ogle’s methodCitation45,Citation46 was used to calculate the ulcer index.
Histopathological examination of stomach
Histopathological tests were performed to evaluate the effects of chemicals (5b and 4e) on the stomach on those of celecoxib and indomethacin, which served as a positive control. In brief, the stomachs of each animal group’s rat were fixed in 10% neutral buffered formalin for 48 h. The sections were then dehydrated, cleared, fixed in paraffin, sectioned (5 m), and stained with H&E stain.
Cardiovascular evaluation
Eighteen rats were divided into three groups at random (6 animals in each group). The first group was given a vehicle and served as normal control. For two weeks, a suspension of the studied compound 5b and celecoxib in a 10% DMSO in saline was given P.O (100 mg/kg) once daily. Ketamine (100 mg/kg) was used to anaesthetise the animals on the 15th day. Blood samples were obtained from the retro orbital, allowed to clot, centrifuged at 1000 g for 15 min, and utilised to examine heart function biomarkers (LDH, CK-MB, and troponin). The abdomen of each rat was opened, and the heart was extracted and washed in ice-cold physiological saline before being harnessed for histological investigation.
Assessment of the cardiac function biomarkers
Troponin, LDH, and CK-MB activities were measured in rats’ sera by spectrophotometer using commercial kits in accordance with manufacturers’ instructions to assess the effect of compound 5d on cardiac function biomarkers in rat serum and then compared to celecoxibCitation47–49.
Histopathological studies of heart
A histopathological examination was conducted to compare the effect of compound 5b on the heart to that of celecoxib. In brief, the hearts of rats given compound 5b and celecoxib, as a control, were fixed in 10% neutral buffered formalin for 48 h. The sections were then dehydrated, cleared, fixed in paraffin, sectioned (5 m), and stained with H&E stainCitation46,Citation50.
Molecular docking study
Molecular Operating Environment (MOE, 2014.0901) software was used in this study for docking analysis. The crystal structure of both COX-2 bound to its ligand celecoxib and 5-LOX with its ligand arachidonic acid were downloaded from the protein data bank (PDB: 3LN1, https://www.rcsb.org/structure/3LN1 and PDB: 3V99, https://www.rcsb.org/structure/3V99, respectively), with the resolution of 2.40 Ǻ for COX-2 isozyme and 2.25 Ǻ for 5-LOX enzyme. For two enzymes, the crystallised ligands were docked and the binding energy scores, amino acid interactions and relative mean square deviation (rmsd) were calculated. The well fitted and the least energetic poses were selected. The same docking protocol was operated for the synthesised compounds inside both COX-2 and 5-LOX active sites. For each docked compound, the most superposed conformer with the ligand with binding interactions resembling that of the ligand was chosen. The energy binding scores (Kcal/mol) and bond length values (Ǻ) were recorded. 2D and 3D pictures of the most predicted active compounds were taken.
Computational analysis
Molecular properties and drug-likeness
Molinspiration (2018.02 version)Citation51 was used to calculate molecular properties such as molecular weight (MW), the number of hydrogen-bond acceptors (HBA), number of hydrogen-bond donors (HBD), partition coefficient (MlogP), number of rotable bonds (nrotb), topological polar surface area (TPSA), and Violation of Lipinski’s rule of five (n-violation). Drug-likeness scores were also determined for all target compounds 3a&b, 4a–e and 5a–e.
Bioactivity prediction
Bioactivity properties of the target compounds 3a&b, 4a–e and 5a–e were checked. The obtained results of a G-protein coupled receptor (GPCR) ligand, ion channel modulator, a kinase inhibitor, nuclear receptor ligand, protease inhibitor, and enzyme inhibitor using molinspirationCitation51 were also recorded.
In silico ADME prediction
To predict in silico ADME properties of the synthesised compounds 3a&b, 4a–e and 5a–e. PreADME online surverCitation52 was used. Human intestinal absorption (HIA), cell permeability of CaCo-2 cell and Madin-Darby Canine Kidney (MDCK) cell, plasma protein binding (PPB), blood brain barrier (BBB) and skin permeability (SP) were calculated.
Metabolism prediction
The most important parameters used to measure metabolism and excretion were cytochrome P450 (CYP) isoforms. Metabolism prediction parameters for the tested compounds 3a&b, 4a-e and 5a–e were examined using the Swissadme online serverCitation53.
Statistical analysis
The obtained data was represented as means ± standard deviations (SD). Significant results were considered when *p˂0.05 or **p˂0.005 using a student’s t-test compared to reference drugs. The obtained values were represented as a result of triple independent experiments.
Results and discussion
Chemistry
General chemistry information
The synthetic procedures for semicarbazone derivatives 3a&b, thiosemicarbazone derivatives 4a–e and thiazolidinone derivatives 5a–e were performed as depicted in Scheme 1.
Scheme 1. Synthetic routes for preparation of indole semicarbazide 3a&b, thiosemicarbazide 4a–e and thiazolidinone 5a–e derivatives.

Starting from indole-3-carboxaldehyde (1), N-methylsulfonylindole carboxaldehyde derivative 2 was prepared through an N-alkylation reaction using a strong base such as sodium hydrideCitation54. The synthesised key intermediate 2, reacted with semi/thiosemicarbazides in the presence of absolute ethanol containing a few drops of DMF to obtain semi/thiosemicarbazone derivatives 3a&b/4a–e via a condensation reaction. Afterward, the obtained thiosemicarbazone derivatives 4a– were cyclized using ethyl chloroacetate and sodium acetate to provide the respective thiazolidinone derivatives 5a–e at good yields ranging from 68 to 79%.
To confirm the chemical structure of the synthesised compounds 3a&b, 4a–e, and 5a–e, 1H NMR, 13C NMR (DEPT-Q), mass spectral data and elemental analysis were determined.
IR spectra of compounds 3a&b, and 4a–e displayed stretching of NH and C = O/or C = S bonds at (3431–3122), (1696 and 1673), or (1129–1058) cm−1, respectively. Additionally, 1H NMR spectra for semi/thiosemicarbazone derivatives 3a&b/4a–e displayed signals at δ 3.49–3.54 and 8.11–8.70 ppm corresponding to -SO2CH3 and azomethine –CH = N– protons, sequentially. Moreover, two D2O exchangeable singlet signals were observed at δ 7.50–11.78 ppm attributed to NH protons of compounds 3a&b and 4a–e.
13C NMR spectra of 3a&b and 4a–e showed peaks at δ (41.51–41.81), (156.50 and 157.10) or (176.18–177.94) ppm owing to carbons of SO2CH3, C = O or C = S, in a sequent.
On the other hand, the structure of thiazolidinone derivatives 5a–e was confirmed using IR spectra through the appearance of an absorption band at 3429 cm−1 attributed to thiazolidinone NH in compound 5a and a band in the range of 1620–1715 cm−1 characteristic of C = O in 5a–e. Additionally, the disappearance of the NH group of the parent compounds in all derivatives 5a–e confirmed the cyclisation process.
Another evidence for ring closure in compounds 5a–e was obtained from 1H NMR spectra, in which a new singlet signal appeared at the range of δ 3.93–4.12 ppm attributed to CH2 protons, in addition to the disappearance of D2O exchangeable singlet signals for their parent compounds 4a–e, while, the appearance of thiazolidinone NH proton of compound 5a at δ 7.51 ppm.
Similarly, the 13C NMR spectra of 5a–e showed chemical shifts for carbons of CH2 and C = O groups in a region of δ 32.59–33.53 ppm and δ 172.45–172.69 ppm, respectively. Additionally, mass spectral data for compound 5b exerted its molecular ion peak at m/z 364.65 by intensity equals 18.87%.
Reagents & conditions
(i) CH3SO3Cl, NaH, DMF, RT, 3 h; (ii) semicarbazone derivatives for 3a&b/or thiosemicarbazone derivatives for 4a–e, abs. EtOH/drops DMF, reflux, 2–4 h; (iii) ClCH2COOEt, NaAc, abs. EtOH/drops DMF, reflux, 4–6 h.
(Z/E) stereochemical determination
To detect the relative configuration (E or Z) for the synthesised indole derivatives 3a&b, 4a–e and 5a–e, 2D NMR NOESY (Nuclear Over Hauser Effect Spectroscopy) experiment was performed.
Compound 4b, as a representative example, was chosen for the NOESY experiment and data obtained revealed the spatial correlation between = N–NH– proton at δ 7.43 ppm and azomethine –CH = N– proton at δ 8.35 ppm (Bond length of NOESY correlating bonds = 1.7 Å in E-form), and between indole H-2 at δ 8.22 ppm and azomethine proton (Bond length of NOESY correlating bonds = 4.5 Å in E-form). While, no spatial interaction was observed between azomethine proton/NH or azomethine proton/indole H-2 in Z-form (Bond length of NOESY correlating bonds >6 Å in Z-form). The obtained results suggested the E-configuration for the synthesised indole derivatives.
Moreover, a theoretical method was performed to confirm the E-configuration for the synthesised derivatives using Chem3D Ultra 12.0 and MM2 properties. Total energy, the sum of stretch, bending, stretch-bend, torsion, non-1,4 Van Der Waals, 1,4 Van Der Waals, and dipole/dipole interactions, was calculated for each Z-/E-conformer. It was noticed that the total energy of the E-form exceeded that of the Z-form for all the target compounds, ( and ).
Figure 2. (A) 2D structure of 4b Z- and E-forms with predicted correlations, (B) 3D structures of 4b Z- and E-forms, (C) NOESY for compound 4b.

Table 1. Predicted total energy for Z- and E-forms of the target compounds 3a&b, 4a–e and 5a–e.
Biological evaluation
Antimicrobial activity screening
All tested compounds were subjected to antimicrobial screening against Gram-positive bacteria, Gram-negative bacteria, and yeast fungus. The obtained data revealed that the ethylthiosemicarbazide derivative, 4b, and p-methoxyphenylthiosemicarbazide compound, 4e showed selective antibacterial activity against the Gram-negative bacteria, E. coli, and Salmonella enterica. Whereas, p-tolylthiazolidinone derivative 5d exclusively exhibited bioactivity against E. coli with diameters ranging from 8 to 15 mm at 100 µg/disc concentration compared to the standard ciprofloxacin which had inhibition zones against all tested Gram-positive and Gram-negative bacteria with diameters’ range from 34 to 48 mm at a concentration of 20 µg/disc. Although our bioactive compounds showed modest antibacterial activity compared to the ciprofloxacin standard, further modifications to their structures could help increase their bioactivity or even broaden their antimicrobial spectrum of activity. On the other hand, the other nine compounds did not display antifungal or antibacterial activity, . The result obtained was in accordance with what was reported about indole derivatives and their antimicrobial activityCitation4,Citation31. Thus, indole derivatives bearing thiazolidinone part and an aliphatic group such as Me or OEt showed the highest antimicrobial activity against both Gram-positive bacteria and Gram-negative bacteriaCitation27. Additionally, indole-hydrazone scaffold and methoxyphenyl substitution exhibited promising antibacterial activity, as reported by Nassar et alCitation31.
Anti-oxidant activity using DPPH radical scavenging activity
The in vitro antioxidant activity of semicarbazides 3a&b, thiosemicarbazides 4a–e and thiazolidinone derivatives 5a, 5c and 5e were determined by measuring the reduction capacity of DPPH radicals spectrophotometrically at 540 nm. Trolox, a water-soluble analog of vitamin E, was used as a standard. By inspecting data in , it was found that the highly anti-oxidant compound between all the tested derivatives was phenylthiazolidinone 5c with a value of 707.52 µM Trolox equivalent/mg. generally, thiosemicarbazide derivatives 4b and 4d showed high scavenging activity on DPPH with values of 426.65 and 389.82 µM Trolox equivalent/mg, in a sequent. Whereas, their thiazolidinone analogs, 5b and 5d, didn’t dissolve in DMSO nor in methanol. The turbidity of these samples hinders their appropriate measurement.
Table 2. DPPH free radical assay results of indole derivatives 3a&b, 4a–e and 5a–e relative to Trolox.
Phenylthiazolidinone derivative 4c showed an increase in anti-oxidant activity of about 263.29 µM Trolox equivalent/mg. Moreover, p-methoxyphenylthiosemicarbazide derivative 4e exerted very high anti-oxidant activities (161.20 µM Trolox equivalent/mg) if compared to its thiazolidinone analogs 5e (13.22 µM Trolox equivalent/mg).
The lowest scavenging activity on DPPH was observed in semicarbazone derivatives 3a and 3b, thiosemicarbazide derivative 4a, its thiazolidinone derivative 5a and p-methoxyphenylthiazolidinone derivative 5e with values ranging from 24.55 to 5.91 µM Trolox equivalent/mg.
It is worth mentioning that between all tested series, thiosemicarbazide moiety increased the antioxidant activity except for phenylthiazolidinone derivative 5c.
Anti-inflammatory activity
In vitro measurements of TNF-α in RAW264.7 macrophage cells
The synthesised compounds were evaluated for their in vitro anti-inflammatory activity using RAW264.7 macrophage cells. The excellent anti-inflammatory activity was obtained by decreasing TNF-α fold, which indicates inhibition of TNF-α production in RAW264.7 cells.
The obtained results represented in revealed that compounds 4d, 4e, 5b, and 5d showed the highest anti-inflammatory activity by decreasing TNF-α to reach 0.19, 0.26, 0.18, and 0.21, respectively, relative to that of indomethacin (0.22) and celecoxib (0.16). The rest of the compounds showed fold changes ranging from 0.35 to 0.53. Both the phenyl semicarbazone derivative, 3b and thiazolidinone derivative, 5a exerted the lowest activity, showing fold changes equal to 0.71 and 0.66, respectively.
COX-1, COX-2 and 5-LOX inhibitory activity determination
All of the synthesised compounds 3a&b, 4a–e and 5a–e were evaluated for their in vitro COX-1, COX-2, and 5-LOX inhibitory activities. Indomethacin, celecoxib, and zileuton were used as reference drugs for COX-1, COX-2, and 5-LOX, respectively. Colorimetric enzyme immunoassay (EIA) kits were done to screen for the isozyme-specific inhibition. To evaluate the effectiveness of the synthesised compounds against COX-1, COX-2, and 5-LOX enzymes, a minimum dose that causes 50% inhibition (IC50) was determined using serial concentrations (100, 10, 1, and 0.1 μM) for each compound. The COX-2 selectivity index values (S.I.) were calculated as [IC50 (COX-1)/IC50 (COX-2)] and compared to the standard drugs, indomethacin (a non-selective COX-inhibitor) and celecoxib (a selective COX-2 inhibitor).
From the obtained data, (), it was observed that all the tested compounds might be of good safety profile as they could inhibit the COX-1 enzyme at higher concentrations (IC50 = 3.95–32.02 uM) than indomethacin (IC50 = 0.38 uM).
Table 3. In vitro COX-1, COX-2 and 5-LOX inhibitory activity results and S.I. of the newly synthesised compounds 3a&b, 4a–e and 5a–e with indomethacin, celecoxib, and ziluton as reference drugs.
On the other hand, the p-methoxyphenylthiosemicarbazide derivative 4e and p-tolylthiazolidinone derivative 5d showed high potency towards COX-2 enzyme inhibition with IC50 = 0.81 and 0.67 μM, sequentially, compared to celecoxib (IC50=0.46 μM). While compounds 4a, 4c, 4d, 5a, 5c, and 5d exerted moderate potency towards COX-2 enzyme inhibition with IC50 values ranging from 1.60 to 8.06 μM. The least activity was observed in ethylthiosemicarbazide derivative 4b and its thiazolidinone derivative 5b with IC50 = 86.15 and 89.22 μM, in a sequent.
Regarding COX-2 selectivity index values, all tested compounds exhibited COX-2 selectivity over COX-1 enzyme (S.I = 0.23–30.17) higher than that of indomethacin (S.I = 0.03). The thiosemicarbazide derivative, 4e, showed a superior S.I. value (30.17) towards COX-2 over COX-1 enzyme than that of celecoxib (S.I.=15.65).
Moreover, compounds containing a thiazolidinone ring with electron donating groups (CH3/OCH3), 5d and 5e, had good COX-2 S.I values (8.59 and 9.72, in order). As a result, compounds 4e, 5d, and 5e might have a safe gastric profile more than or nearly equal to that of celecoxib.
Concerning 5-LOX inhibitory activity results, compound 5d (p-tolylthiazolidinone derivative) was the only one among all tested compounds that showed inhibitory activity against 5-LOX enzyme (IC50 = 1.10 μM) if compared to zileuton, the reference drug, (IC50 = 0.57 μM). Additionally, good to moderate 5-LOX inhibitory activity was observed in compounds 4a, 4c, 4e, 5a, and 5e (IC50 = 2.31–9.23 μM). Dual COX-2/5-LOX inhibitory activity was achieved mainly by compound 5d, from which, it might be expected to have anti-inflammatory activity as well as cardioprotective effect.
Evaluation of ulcerogenic effect
Ulcerogenic liability
The most selective compounds, 4e and 5d, were shown to have an ulcerogenic impact when compared to the reference drug celecoxib and the ulcerogenic non-selective COX-2 inhibitor indomethacin, utilising a 50 mg/kg dosage for three consecutive days to show their gastrointestinal safety profile. The acquired findings are depicted in (). Our findings suggested that all tested compounds had a lower ulceration impact than celecoxib and indomethacin, the reference drugs, as evidenced by an ulcer index range (U.I. = 0.2–1.3) as compared to celecoxib (U.I. = 3.79) and indomethacin (U.I. = 6.8). The most selective molecule, p-methoxyphenyl thiosemicarbazide derivative 4e, was also the least ulcerogenic (U.I. = 0.2). In addition, the p-tolylthiazolidinone derivative 5d, demonstrated an excellent ulcer index (1.3) as compared to celecoxib (U.I. = 3.97).
Table 4. Ulcerogenic liability for the highest S.I. 4e, 5d and reference drugs celecoxib and indomethacin.
Stomach histopathological examination
In order to compare the severity of lesions to those caused by the reference drugs celecoxib and indomethacin as well as to the lesions in the control negative group, evaluation of the ulcerogenic effect of tested compounds on various stomach portions through examination of variable histopathological lesions was carried out. Normal control rats showed normal gastric mucosa with a normal pattern and architecture of the gastric gland (H & E X 200) (); another view showed normal gastric mucosa with normal pattern and architecture of gastric gland with preservation of parietal cells (yellow arrow) and chief cells (red arrow) (H & E X 400) (). On the other hand, celecoxib group showed gastric tissue with superficial mucosal erosion showing disrupted mucous layer (black arrow), degenerated mucosal epithelial cells, decrease number of parietal cells (orange arrow) in superficial mucosa, average number of parietal and chief cells (yellow arrow) in deep mucosa and average muscularise mucosa (red arrow) (H & E X 200) (); another view indicated mucosal ulceration showing destructed mucus layer, degenerated mucosal epithelial cells in the base of the ulcer, absence of parietal cells and chief cells in the base of the ulcer with decreasing number in adjacent mucosa, and average muscularise mucosa (red arrow) (H & E X 200) (); Also the view in deep mucosa revealed marked mucosal ulceration showing completely destructed mucous layer, complete loss of parietal and chief cells, marked inflammations and beginning of fibrosis in ulcer bases (increase thickening of muscularis mucosa), devitalised mucosal epithelial cells (green arrow) in ulcer margins and adjacent mucosa, with decreasing number of parietal cells and chief cells in adjacent mucosa (H & E X 200) (). In conclusion, celecoxib administration resulted in multiple complete ulcers and superficial mucosal erosions with disrupted mucous layer, average number of parietal and average chief cells in deep mucosa with average muscularise mucosa, degenerated mucosal epithelial cells in the base of the ulcer, marked inflammations and beginning of fibrosis in ulcer bases, and devitalised mucosal epithelial cells in ulcer margins and adjacent mucosa.
Figure 5. Effects of celecoxib, indomethacin, and the highest selective compounds 4e and 5d on the stomach histology (H & E X 400 & 200).

While indomethacin administration viewed gastric tissue with superficial mucosal erosion showing disrupted mucous layer (black arrow), degenerated mucosal epithelial cells, edoema and decrease number of parietal cells (orange arrow) in superficial mucosa, average number of parietal and chief cells (yellow arrow) in deep mucosa and average muscularise mucosa (red arrow) (H & E X 200) (); another view showed gastric tissue with marked mucosal ulceration showing marked congested vessels in the base of the ulcer, decreasing number of parietal cells in adjacent mucosa, and inflamed thickened muscularise mucosa (red arrow) (H & E X 200) (); another view showed ulcer bases with perforated mucosal ulcer (black star) showing marked inflammations, edoema (red star), beginning of fibrosis, devitalised mucosal epithelial cells in ulcer base and adjacent mucosa, with decreasing number of parietal cells and chief cells in adjacent mucosa, inflamed thickened muscularise mucosa (H & E X 200) (). In conclusion, indomethacin administration resulted in multiple complete and perforating ulcers and superficial erosions, marked mucosal ulceration showing marked congested vessels in the base of the ulcer, decreasing number of parietal cells in adjacent mucosa, and inflamed thickened muscularise mucosa as well as ulcer bases with a perforated mucosal ulcer with marked inflammations, edoema, beginning of fibrosis, devitalised mucosal epithelial cells in ulcer base and adjacent mucosa, with decreasing number of parietal cells and chief cells in adjacent mucosa, inflamed thickened muscularise mucosa.
Scanning the stomach of the rats treated with the tested compounds 4e and 5d showed the following:
For compound 4e: gastric tissue showed retaining of the mucous layer (black arrow), regenerated mucosal epithelial cell layers, preserved a number of parietal cells (orange arrows) and chief cells (yellow arrow), with minimal mucosal, submucosal edoema, inflammations and average muscularis mucosa (red arrow) (H & E X 200 & 400) (–3D)). In conclusion, administration of the p-methoxythiosemicarbazide derivative 4e resulted in partial loss of mucous layer with mild superficial erosions accompanied by mucosal epithelial cell layers’ regeneration, preserved parietal cells and chief cells in superficial and deep mucosa, minimal mucosal, submucosal edoema, inflammations and average muscularis mucosa.
For compound 5d: gastric tissue showing minimally disrupted mucous layer (black arrow), regenerated mucosal epithelial cells layers with minimal residual surface epithelial erosions, preserved number of parietal cells (orange arrows) and chief cells (yellow arrow), with mild mucosal, submucosal edoema and inflammations and minimally decrease thickening of muscularis mucosa (red arrow) (H & E X 200) ()). In conclusion, administration of the p-tolylthiazolidinone derivative 5b resulted in partial loss of the mucous layer with mild, superficial erosions, preserved number of parietal cells and chief cells in superficial and deep mucosa, mild mucosal, submucosal edoema and inflammations and minimally decrease thickening of muscularis mucosa.
Cardiovascular evaluation
Assessment of the cardiac function biomarkers
It has been previously noted that celecoxib has cardio-toxicity in experimental ratsCitation55. Heart function indicators such as Troponin I, Creatine kinase-MB (CK-MB), and lactate dehydrogenase (LDH) were assessed in the current investigation to determine how the heart responded to the most active and most selective target compound, 5d. Additionally, a comparison of the assessed compound 5d to celecoxib as a reference standard was done regarding the study its histopathological changes. All of the findings were displayed in (). The findings showed that the injection of celecoxib caused a significantly higher level of the serum cardiac biomarkers Troponin I, CK-MB, and LDH when compared to normal control rats. Contrarily, animals treated with thiazolidinone derivative, 5d, had substantially lower serum levels of these indicators than rats treated with celecoxib. These findings demonstrated that, in comparison to celecoxib, compound 5d carries a considerably lower risk of cardiovascular damage.
Table 5. Cardiac effects of compound 5d and the reference drug celecoxib.
Histopathological examination of the heart
Histopathological examination of the heart muscle of the control group shows a normal pattern of cardiac muscle fibres with normal cigar shaped nuclei (red arrows) and normally arranged blood vessels (yellow arrows) (H & E X 200 & X 400) ( and ). On the contrary, the heart section obtained from celecoxib group showed markedly inflamed cardiac muscle fibres with vacuolar degenerated myocytes (yellow arrow), edoema and dilated ectatic blood vessels containing plasma fluid (red arrow) (H & E X 200) (); another view revealed markedly inflamed cardiac muscle fibres with vacuolar degenerated myocytes (yellow arrow), degenerated myocytes with brown pigmentation (black arrow) edoema, inflammatory cells (orange arrow) and dilated ectatic blood vessels containing plasma fluid (red arrow) (H & E X 400) (). In conclusion, prolonged administration of celecoxib resulted in scattered inflamed cardiac muscle fibres with vacuolar degenerated myocytes with brown pigmentation, edoema as well as markedly congested and dilated ectatic blood vessels containing plasma fluid in the heart muscle. Alternatively, cardiac histopathological examination of the thiazolidinone derivative 5d treated group revealed little or no toxic effects on the heart and showed viable cardiac muscle fibres retained to their normal pattern with regenerated myocytes and normal arranged blood vessels (yellow arrows) (H & E X 200) (); another view revealed cardiac muscle fibres retained to their normal pattern with regenerated myocytes, normal cigar shape nuclei (red arrow) and normal arranged blood vessels (yellow arrows) (H & E X 400) ().
Molecular docking study
In this study, the mode of action of N-methylsulfonyl indole derivatives 3a&b, 4a–e, and 5a–e as novel COX‐2, and 5-LOX inhibitors were determined via molecular docking studies. Docking of COX-2 ligand, celecoxib, and 5-LOX ligand, arachidonic acid, inside the binding site of COX‐2 (Protein Data Bank code: 3ln1) and 5-LOX (Protein Data Bank code: 3V99) was performed to compare between the key structural features for both ligands and the designed candidates. The docking energy affinity (Kcal/mol), interactions and amino acid residues indicated the binding mode for the developed new compounds such as COX‐2 and/or 5-LOX inhibitors.
Regarding the COX-2 docking study, the docking study of celecoxib, a selective COX-2 inhibitor, showed a binding energy of −7.52 Kcal/Mol. It formed three hydrogen bonding interactions with Gln178, Ser339 and Arg499 amino acid residues with NH2 and SO2 groups and one arene-H interaction with P-SO2NH2Ph moiety, (, ).
Figure 7. Binding mode of celecoxib inside COX-2 active site, (A) 3D visualisation of co-crystallised celecoxib ligand (yellow colour) superimposed with redocked celecoxib (cyan colour), indicating good fitting inside the pocket, (B) 2D binding mode of celecoxib inside COX-2 active site showing three H-bonding interactions with Arg499, Gln178, and Ser339 amino acid residues and one arene-H interaction with Ser339 amino acid residue.

Table 6. Results of molecular docking study for synthesised indole derivatives ligands of COX-2 and 5-LOX enzymes.
Additionally, docking studies for testing derivatives revealed that the energy of binding interactions ranged from −6.44 to −2.40 Kcal/Mol, and formed one to five binding interactions or without any interactions at all. The most active COX-2 inhibitors, p-methoxyphenylthiosemicarbazide derivative, 4e and p-tolylthiazolidinone derivative, 5d showed the highest energy scores of −6.37 and −6.44 Kcal/Mol and formed five and one binding interaction(s), respectively, with Ser516, Phe504, His75 and Ser339 amino acid residues with indole ring (phenyl and pyrrole), C = S and SO2CH3 pharmacophores, in addition to a p-tolyl moiety in compound 5d, ( and , ).
Figure 8. Binding mode of 4e inside COX-2 active site, (A) 3D visualisation of 4e (yellow colour) superimposed with celecoxib (cyan colour), indicating good fitting inside the pocket, (B) 2D binding mode of 4e inside COX-2 active site showing two H-bonding interactions with Ser516 and Phe504 amino acid residues and three arene-H interactions with Ser339 and His75 amino acid residues.

Figure 9. Binding mode of 5d inside COX-2 active site, (A) 3D visualisation of 5d superimposed with celecoxib, indicating good fitting inside the pocket, (B) 2D binding mode of 5d inside COX-2 active site showing one arene-H interaction with Ser339 amino acid residue.

On the other hand, the last two derivatives, as COX-2 inhibitors, were ethyl derivatives of thiosemicarbazide, 4b, and thiazolidinone, 5b. They revealed binding energy scores of −2.62 and −2.4026, sequentially. Compound 4b didn’t form any type of binding interaction, while compound 5b exerted one arene-hydrogen interaction between the pyrrole ring of indole and Ser339 amino acid residue, ().
Concerning docking studies inside the 5-LOX enzyme, data obtained revealed that the active site of the enzyme formed two hydrogen bonding interactions between His432 and His600 amino acid residues and a –(-COO-) group of arachidonic acid, the redocked co-crystallised ligand compound with a binding energy score of −7.82 Kcal/Mol (, ).
Figure 10. Binding mode of arachidonic acid inside 5-LOX active site, (A) 3D visualisation of co-crystallised arachidonic acid (yellow colour) superimposed with redocked arachidonic acid (cyan colour), indicating good fitting inside the pocket, (B) 2D binding mode of arachidonic acid inside 5-LOX active site showing two H-bonding interactions with His432 and His600 amino acid residues.

The most active p-tolyl thiosemicarbazide derivative as a 5-LOX inhibitor, 5d, had the highest binding energy score of −9.91 Kcal/Mol, higher than that of the ligand. It had two hydrophobic interactions between the phenyl of the indole ring and His432 and His600 amino acid residues (the same as that of the ligand) (, ).
Figure 11. Binding mode of 5d inside 5-LOX active site, (A) 3D visualisation of 5d (yellow colour) superimposed with redocked arachidonic acid (cyan colour), indicating good fitting inside the pocket, (B) 2D binding mode of 5d inside 5-LOX active site showing two H-bonding interactions with His432 and His600 amino acid residues.

Moreover, most of the tested derivatives showed energy binding interactions nearly equal to the ligand from −7.78 to −7.19 Kcal/Mol and formed binding interactions of one to two with Gln363, Asn554, His600, His432, His367, and His372 amino acid residues, ().
On the other hand, semicarbazide derivatives 3a&b, ethylthiosemicarbazide derivative 4b, p-tolylthiosemicarbazide 4d, and ethyl or phenyl thiazolidinone derivatives 5b&c showed energy binding interactions between −6.96 to −6.03 Kcal/mol, formed one or two binding interaction(s) with His367, Gln557, His432, and Lys 409 amino acid residues or without any binding interactions as in 3a, 4b, and 5b, ().
In conclusion, the molecular docking study results of COX-2 and 5‐LOX enzymes indicated that the p-methoxy derivative of thiosemicarbazide 4e had COX-2 binding activity, while the p-tolyl derivative of thiazolidinone 5d, showed dual COX-2/5-LOX binding affinities. Both of them contain an electron-donating group in the para position of the phenyl ring.
Computational analysis
Molecular properties and drug-likeness
Lipiniski’s rule of five (RO5) analysis was used in this study to predict the biochemical properties of the synthesised target compounds. All compounds achieved Lipinisk’s rule of five standard values with a violation number of zero, (). Thus, the molecular weight of the target derivatives ranged from 280–442 g/Mol. That means less than the standard value of 500 g/Mol. Also, both hydrogen-bond acceptor and donor of tested compounds were in the range of 4 − 7 and 0–3, respectively, they didn’t exceed the acceptable values (No. HBA <10 and No. HBD <5). Moreover, the number of rotatable bonds, which indicate molecular flexibility, was from 3 to 5 (standard value <10). Lipophilic indicator LogP (octanol/water) partition co-efficient was evaluated for the target compounds. All showed high to moderate membrane permeability with partition co-efficient values in the range of 0.74–3.13 (within the acceptable range, <5).
Table 7. Molecular properties and drug-likeness results for the synthesised indole derivatives 3a&b, 4a–e and 5a–e.
Prediction of oral bioavailability was determined from polar surface area (PSA) which should be less than 140 Ǻ. This was achieved by the target compounds (75 − 106 Ǻ). On the other hand, drug-likeness scores were acceptable for the target compounds, especially those containing semicarbazone moiety 3a (-0.07) and for p-methoxyphenyl thiosemicarbazide derivative 4e (-0.04).
Bioactivity prediction
Interaction between synthesised compounds and certain drug targets might be a tool for their bioactivity prediction. From these drug targets, a G-protein coupled receptor (GPCR), an ion channel modulator, a kinase inhibitor, a nuclear receptor ligand, and protease inhibitor were studied. To consider the activity of the synthesised compounds, they should possess values >0.00 to be good lead structure, −0.50 to 0.00 as moderately bioactive, or < −0.50 to be inactive.
By inspecting the results obtained (), it was found that semicarbazone derivatives 3a and 3b showed good lead structures for G-protein coupled receptor (GPCR), while the rest of the compounds had moderate bioactivity.
Table 8. Bioactivity prediction for the synthesised indole derivatives 3a&b, 4a–e and 5a–e.
All tested derivatives were inactive as ion channel modulators and protease inhibitors. Compounds 3b, 4c, and 4e bearing phenyl semicarbazone/thiosemicarbazone or p-methoxyphenylthiosemicarbazone scaffolds were moderately active as kinase inhibitors and nuclear receptor ligand, in addition to semicarbazone derivative 3a and p-tolylthiosemicarbazone derivative 4d that might be considered as kinase inhibitors.
In silico ADME prediction
Pharmacokinetic properties (absorption, distribution, metabolism and excretion) for the synthesised compounds were predicted using in silico ADME prediction.
The obtained results were recorded in . All the target compounds showed high intestinal absorption with values ranging from 93.40 to 99.66% and reached 100% in the case of thiazolidinone derivative 5e. Low to moderate permeability results were observed for in vitro CaCo-2 and MDCK cells in the range 0.58–24.16 and 0.04–19.81 nm/sec, respectively. Most of the compounds exerted a strong binding effect on plasma proteins higher than 90% except semicarbazone derivative 3a and thiosemicarbazone derivatives 4a and 4b. They possessed plasma binding values of 57.14, 79.56, and 86.83%, sequentially.
Table 9. ADME prediction for the synthesised indole derivatives 3a&b, 4a–e and 5a–e.
Moreover, all the synthesised compounds exerted low absorption into the CNS. They couldn’t penetrate it. They had values in the range of 0.01–0.21 (i.e. <0.40, the standard value). Consequently, all the synthesised targets might be a good lead for the transdermal delivery systems. They showed maximum skin permeability with logKp values ranging from −2.88 to −1.74 cm/h.
Metabolism prediction
Metabolism prediction was obtained by studying phase I metabolism parameters. Data in shows that most of the compounds could inhibit the cytochrome P450 isoform CYP-2C9. While none of them could inhibit other cytochrome isoforms such as CYP-2C19, CYP-2D6 and CYP-3A4.
Table 10. Metabolism prediction for the synthesised indole derivatives 3a&b, 4a-e and 5a-e.
Conclusion
A novel series of N-methylsulfonyl indole derivatives fused with semicarbazone 3a&b, thiosemicarbazone 4a–e, and thiazolidinone 5a–e scaffolds were synthesised and evaluated for their biological activities. The antimicrobial screening revealed that thiosemicarbazide derivatives, 4b and 4e showed selective antibacterial activity against the Gram-negative bacteria, E. coli and Salmonella enterica. Whereas thiazolidinone derivative 5d exhibited bioactivity against E. coli only. On the other hand, the tested compounds did not display antifungal activity. The in vitro antioxidant activity of the target compounds showed that phenylthiazolidinone derivative 5c had the highest anti-oxidant activity among all the tested derivatives with a value of 707.5 µM Trolox equivalent/mg. For most thiosemicarbazide derivatives, their anti-oxidant activity was higher than their thiazolidinone analogs. The lowest scavenging activity on DPPH was observed in semicarbazone derivatives 3a and 3b, unsubstituted thiosemicarbazide derivative 4a, its thiazolidinone analog 5a and p-methoxyphenylthiazolidinone derivative 5e. The in vitro anti-inflammatory results by measuring TNF-α in RAW264.7 macrophage cells revealed that compounds 4d, 4e, 5b and 5d had the highest anti-inflammatory activity, while, phenyl semicarbazone derivative, 3b and thiazolidinone derivative, 5a exerted the lowest activity. Furthermore, the synthesised compounds were tested against COX-1, COX-2 and 5-LOX enzymes. Compound 4e could be classified as a selective COX-2 inhibitor and compound 5d had dual COX-2/5-LOX inhibitory activity. As a result, measuring cardiac biomarkers (LDH, CK-MB and Tn-I) for compound 5d elicited low levels. A histopathological study affirmed the cardioprotective profile for the target compound 5d. Additionally, for both derivatives, 4e and 5d, ulcerogenic liability and the histopathological study confirmed their safety effect on the gastric mucosa. Moreover, a docking study for the target compounds inside COX-2 and 5-LOX active sites was performed to explain their plausible binding mode. Finally, an ADMET study and pharmacokinetic properties were applied and proved the promising activity of the new compounds. In conclusion, the newly developed compounds represent biologically active multi-target candidates with fewer side effects. Structure-activity relationship (SAR) is represented in the following .
Supplemental Material
Download Zip (944.7 KB)Acknowledgement
The authors would like to thank the Deanship of Scientific Research at Umm Al-Qura University for supporting this work using Grant Code: (23UQU4290565DSR100).
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
The data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Additional information
Funding
References
- Meshram MA, Bhise UO, Makhal PN, Kaki VR. Synthetically-tailored and nature-derived dual COX-2/5-LOX inhibitors: structural aspects and SAR. Eur J Med Chem. 2021;225:113804–113831.
- P JJ, Manju SL, Ethiraj KR, Elias G. Safer anti-inflammatory therapy through dual COX-2/5-LOX inhibitors: a structure-based approach. Eur J Pharm Sci. 2018;121:356–381.
- Lamie PF, Ali WAM, Bazgier V, Rárová L. Novel N-substituted indole Schiff bases as dual inhibitors of cyclooxygenase-2 and 5-lipoxygenase enzymes: synthesis, biological activities in vitro and docking study. Eur J Med Chem. 2016;123:803–813.
- Archana K, Singh RK. Medicinal chemistry of indole derivatives: current to future therapeutic prospectives. Bioorg Chem. 2019;89:103021–103056.
- Sehajpal S, Prasad DN, Singh RK. Prodrugs of non-steroidal anti-inflammatory drugs (NSAIDs): a long march towards synthesis of safer NSAIDs. Mini Rev Med Chem. 2018;18(14):1199–1219.
- Perrone MG, Scilimati A, Simone L, Vitale P. Selective COX-1 inhibition: a therapeutic target to be reconsidered. Curr Med Chem. 2010;17(32):3769–3805.
- Sehajpal S, Prasad DN, Singh RK. Novel ketoprofen-antioxidants mutual codrugs as safer nonsteroidal anti-inflammatory drugs: synthesis, kinetic and pharmacological evaluation. Arch Pharm. 2019; 352(7):e1800339.
- Huang Y, Zhang B, Li J, Liu H, Zhang Y, Yang Z, Liu W. Design, synthesis, biological evaluation and docking study of novel indole-2-amide as anti-inflammatory agents with dual inhibition of COX and 5-LOX. Eur J Med Chem. 2019;180:41–50.
- Shaaban MA, Kamal AM, Faggal SI, Farag NA, Aborehab NM, Elsahar AE, Mohamed KO. Design, synthesis, and biological evaluation of new pyrazoloquinazoline derivatives as dual COX‐2/5‐LOX inhibitors. Arch Pharm. 2020;353(11):2000027–2000044.
- Lamie PF, Philoppes JN, Azouz AA, Safwat NM. Novel tetrazole and cyanamide derivatives as inhibitors of cyclooxygenase-2 enzyme: design, synthesis, anti-inflammatory evaluation, ulcerogenic liability and docking study. J Enzyme Inhib Med Chem. 2017;32 (1):805–820.
- Bray MA, Ford AW, Smith MJH. Leukotriene B4: an inflammatory mediator in vivo. Prostaglandins. 1981;22(2):213–222.
- Penrose JF, Austen KF, Lam BK, editors. Inflammation. Basic Princ Clin Correl. 1999:361–372.
- Lamie PF, Philoppes JN, Rárová L. Design, synthesis, and biological evaluation of novel 1, 2‐diaryl‐4‐substituted‐benzylidene‐5(4H)‐imidazolone derivatives as cytotoxic agents and COX‐2/LOX inhibitors. Arch Pharm Chem Life Sci. 2018;351(3–4):1700311–1700322.
- Morphy R, Rankovic Z. Medicinal chemistry approaches for multitarget drugs. Burger Med Chem Drug Discov. 2003:249–274.
- Charlier C, Michaux C. Dual inhibition of cyclooxygenase-2 (COX-2) and 5-lipoxygenase (5-LOX) as a new strategy to provide safer non-steroidal anti-inflammatory drugs. Eur J Med Chem. 2003;38(7–8):645–659.
- Sandes SMS, Heimfarth L, Brito RG, Santos PL, Gouveia DN, Carvalho AMS, Quintans JSS, da Silva-Júnior EF, de Aquino TM, França PHB, et al. Evidence for the involvement of TNF-α, IL-1β and IL-10 in the antinociceptive and anti-inflammatory effects of indole-3-guanylhydrazone hydrochloride, an aromatic aminoguanidine, in rodents. Chem Biol Interact. 2018;286:1–10.
- Kwon TH, Yoon IH, Shin J-S, Lee YH, Kwon BJ, Lee K-T, Lee YS. Synthesis of indolyl-3-acetonitrile derivatives and their inhibitory effects on nitric oxide and PGE2 productions in LPS-induced RAW 264.7 cells. Bioorg Med Chem Lett. 2013;23(9):2571–2574.
- Abdelazeem AH, El-Saadi MT, Safi El-Din AG, Omar HA, El-Moghazy SM. Design, synthesis and analgesic/anti-inflammatory evaluation of novel diarylthiazole and diarylimidazole derivatives towards selective COX-1 inhibitors with better gastric profile. Bioorg Med Chem. 2017;25(2):665–676.
- Gupta S, Sarotra P, Aggarwal R, Dutta N, Agnihotri N. Role of oxidative stress in celecoxib-induced renal damage in Wistar rats. Dig Dis Sci. 2007;52(11):3092–3098.
- Lamie PF, Azmey AF. Synthesis and biological evaluation of tetrazole derivatives as TNF-α, IL-6 and COX-2 inhibitors with antimicrobial activity: computational analysis, molecular modeling study and region-specific cyclization using 2D NMR tools. Bioorg Chem. 2019; 92:103301–103317.
- Song M, Wang S, Wang Z, Fu Z, Zhou S, Cheng H, Liang Z, Deng X. Synthesis, antimicrobial and cytotoxic activities, and molecular docking studies of N-arylsulfonylindoles containing an aminoguanidine, a semicarbazide, and a thiosemicarbazide moiety. Eur J Med Chem. 2019;166:108–118.
- Gupta A, Singh R, Sonar PK, Saraf SK. Novel 4-thiazolidinone derivatives as anti-infective agents: synthesis, characterization, and antimicrobial evaluation. Biochem Res Int. 2016;2016:8086762–8086769.
- Arunasree MK, Rizvi A. Inhibition of bacterial multidrug resistance by celecoxib, a cyclooxygenase-2 inhibitor. Antimicrob Agents Chemother. 2011;55(1):439–442.
- Pham-Huy LA, He H, Pham-Huy C. Free radicals, antioxidants in disease and health. Int J Biomed Sci. 2008;4(2):89–96.
- Lamie PF, Phillopes JN, El-Gendy AO, Rarova L, Gruz J. Design, synthesis and evaluation of novel phthalimide derivatives as in vitro anti-microbial, anti-oxidant and anti-inflammatory agents. Molecules. 2015;20(9):16620–16642.
- Kumari M, Singh RK. Synthesis, molecular docking and biological evaluation of N-substituted indole derivatives as potential anti-Inflammatory and antioxidant agents. Chem Biodivers. 2022;19(9):202200290.
- Abo-Ashour MF, Eldehna WM, George RF, Abdel-Aziz MM, Elaasser MM, Abdel Gawad NM, Gupta A, Bhakta S, Abou-Seri SM. Novel indole-thiazolidinone conjugates: design, synthesis and whole- cell phenotypic evaluation as a novel class of antimicrobial agents. Eur J Med Chem. 2018;160:49–60.
- Kumari A, Singh RK. Synthesis, molecular docking and ADME prediction of 1H-indole/5-substituted indole derivatives as potential antioxidant and anti-inflammatory agents. MC. 2022;18.
- Garg V, Maurya RK, Thanikachalam PV, Bansal G, Monga V. An insight into the medicinal perspective of synthetic analogs of indole: a review. Eur J Med Chem. 2019;180:562–612.
- Choppara P, Prasad YV, Rao CV, Hari Krishna K, Trimoorthulu G, Maheswara Rao GU, Venkateswara Rao J, Bethu MS, Murthy YLN. Design, synthesis of novel N prenylated indole-3-carbazones and evaluation of in vitro cytotoxicity and 5-LOX inhibition activities. Arab J Chem. 2019;12 (8):2328–2335.
- Liu L, Chen Y-Y, Qin X-J, Wang B, Jin Q, Liu Y-P, Luo X-D. Antibacterial monoterpenoid indole alkaloids from Alstonia scholaris cultivated in temperate zone. Fitoterapia. 2015;105:160–164.
- Cihan-Üstündağ G, Gürsoy E, Naesens L, Ulusoy-Güzeldemirci N, Çapan G. Synthesis and antiviral properties of novel indole-based thiosemicarbazides and 4-thiazolidinones. Bioorg Med Chem. 2016;24(2):240–246.
- Sevinçli ZŞ, Duran GN, Özbil M, Karalı N. Synthesis, molecular modeling and antiviral activity of novel 5-fluoro-1H-indole-2,3-dione 3-thiosemicarbazones. Bioorg Chem. 2020;104:104202–104214.
- Güze Ö, Karalı N, Salman A. Synthesis and antituberculosis activity of 5-methyl/trifluoromethoxy-1H-indole-2,3-dione 3-thiosemicarbazone derivatives. Bioorg Med Chem. 2008;16(19):8976–8987.
- de Oliveira JF, Lima TS, Vendramini-Costa DB, de Lacerda Pedrosa SCB, Lafayette EA, da Silva RMF, de Almeida SMV, de Moura RO, Ruiz ALTG, de Carvalho JE, et al. Thiosemicarbazones and 4-thiazolidinones indole-based derivatives: Synthesis, evaluation of antiproliferative activity, cell death mechanisms and topoisomerase inhibition assay. Eur J Med Chem. 2017;136:305–314.
- Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: a review. J Pharm Anal. 2016;6(2):71–79.
- Stengel DB, Connan S, editors. Natural products from marine algae: Methods and protocols. New York (NY): Springer; 2015. (Methods in Molecular Biology; MIMB, vol 1308).
- Heatley NG. A method for the assay of penicillin. Biochem J. 1944;38(1):61–65.
- Boly R, Lamkami T, Lompo M, et al. DPPH free radical scavenging activity of two extracts from Agelanthus dodoneifolius (Loranthaceae) leaves. Int J Tox Pharmacol Res. 2016; 8 (1):29–34.
- Kenneth S, T. Belete M. A simple, inexpensive method for preparing cell lysates suitable for downstream reverse transcription quantitative PCR. Sci Rep. 2014;4(1):4659–4666.
- Yamamoto S. Mammalian lipoxygenases: molecular structures and functions. Biochim Biophys Acta. 1992;1128(2–3):117–131.
- Gaffney BJ. Lipoxygenases: structural principles and spectroscopy. Annu Rev Biophys Biomol Struct. 1996;25:431–459.
- Zhang ZH, Chung TDY, Oldenburg KR. A simple statistical parameter for use in evaluation and validation of high throughput screening assays. J Biomol Screen. 1999;4(2):67–73.
- Adedapo AA, Sofidiya MO, Maphosa V, et al. Antiinflammatory and analgesic activities of the aqueous extract of Cussonia Paniculatastem bark. Rec Nat Prod. 2008;2:46–53.
- Cho CH, Ogle CW. Cholinergic-mediated gastric mast cell degranulation with subsequent histamine H1-and H2 receptor activation in stress ulceration in rats. Eur J Pharmacol. 1979;55(1):23–33.
- Bancroft JD, Gamble M. Theory and practice of histological techniques. 6th Edition, China: Churchill Livingstone Elsevier, Elsevier Health Sciences.
- Docherty JC, Gerrard JM. An enzyme-linked immunosorbent assay for 6-Keto PGF alfa. Prostaglandins. 1986;31(3):375–383.
- Rao PS, Lukes JJ, Ayres SM, Mueller H. New manual and automated method for determining activity of creatine kinase isoenzyme MB, by use of dithiothreitol: clinical applications. Clin Chem. 1975;21(11):1612–1618.
- Martinek RG. A rapid ultraviolet spectrophotometric lactic dehydrogenase assay. Clin Chim Acta. 1972;40(1):91–99.
- Hassanein EHM, Abd El-Ghafar OAM, Ahmed MA, Sayed AM, Gad-Elrab WM, Ajarem JS, Allam AA, Mahmoud AM. Edaravone and acetovanillone upregulate Nrf2 and PI3K/Akt/mTOR signaling and prevent cyclophosphamide cardiotoxicity in rats. Drug Des Devel Ther. 2020;14:5275–5288.
- [cited 2022 Feb 20]. Available from: https://www.molinspiration.com/.
- [cited 2022 Feb 20]. Available from: https://preadmet.qsarhub.com/.
- [cited 2022 Feb 21]. Available from: http://www.swissadme.ch/.
- Lamie PF, Philoppes JN. Design, synthesis, stereochemical determination, molecular docking study, in silico pre-ADMET prediction and anti-proliferative activities of indole-pyrimidine derivatives as Mcl-1 inhibitors. Bioorg Chem. 2021;116:105335–105351.
- Ahmad S, Panda BP, Fahim M, Dhyani N, Dubey K. Ameliorative effect of beraprost sodium on celecoxib induced cardiotoxicity in rats. Iran J Pharm Res. 2018;17(1):155–163.