ABSTRACT
Introduction
Over the last four decades, human immunodeficiency virus type 1 (HIV-1) infection has been a major public health concern. It is acknowledged that an effective vaccine remains the best hope for eliminating the HIV-1 pandemic. The prophylaxis of HIV-1 infection remains a central theme because of the absence of an available HIV-1 vaccine. The inability of conventional delivery strategies to induce potent immunity is a crucial task to overcome and ultimately lead to a major obstacle in HIV-1 vaccine research.
Areas covered
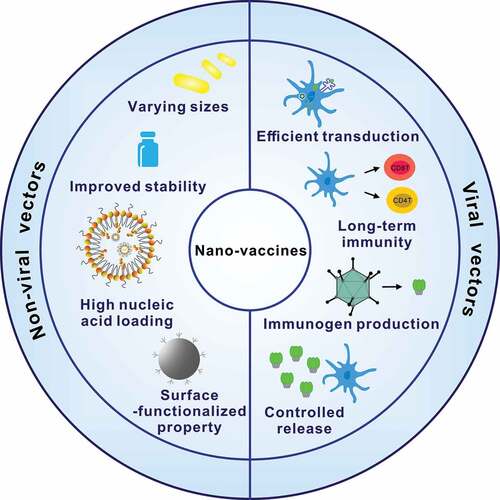
The literature search was conducted in the following databases: PubMed, Web of Science, and Embase. Nano-platforms-based vaccines have proven prophylaxis in various diseases for effectively activating the immune system. Nano-vaccines, including non-viral and viral vectored nano-vaccines, are in a position to improve the effectiveness of HIV-1 antigen delivery and enhance the innate and adaptive immune responses against HIV-1. Compared to traditional vaccination strategies, genetic immunization can elicit a long-term immune response to provide protective immunity for HIV-1 prevention.
Expert opinion
Research progress on nano-vaccines for gene delivery against HIV-1 was discussed. Vaccine strategies based on nano-platforms that are being applied to stimulate effective HIV-1-specific cellular and humoral immune responses were particularly emphasized.
1. Introduction
The human immunodeficiency virus type 1 (HIV-1) pandemic remains a devastating infectious pathogen [Citation1,Citation2], with UNAIDS reporting that a total of 38.4 million cases worldwide were infected with HIV until 2021 (https://www.unaids.org/en). Pre-exposure prophylaxis and antiretroviral therapy have revolutionized HIV-1 prevention and treatment, transforming HIV-1 from what used to be regarded as a loss of life sentence to a chronic disease [Citation3–5]. However, effective HIV-1 treatment and prevention demand strict dosing regimens and lifelong medication [Citation6]. In addition, viral rebound inevitably occurs in some HIV-1-infected individuals that are developing drug resistance [Citation7]. Therefore, many experts agree that obliteration of the HIV-1 pandemic still requires valid preventive vaccines [Citation8,Citation9]. Nevertheless, developing an efficient HIV-1 vaccine has been demonstrated to be inordinately hard [Citation10]. To date, a licensed vaccine against HIV-1 has yet to be created. The RV144 trial has been the only clinical trial to demonstrate a significant protection in humans [Citation11]. The vaccine regimen based on a canarypox vector-based vaccine prime and two HIV-1 gp120 boosts in the RV144 trial elicited protective non-neutralizing antibodies against the V1/V2 region of the HIV-1 envelope (Env), resulting in 31.2% efficacy for the prophylaxis of HIV-1 [Citation11].
An optimal HIV-1 vaccine will generate both humoral and cellular immune responses, providing protective immunity against HIV-1. Neutralizing antibodies are able to prevent mammalian cells from HIV-1 infection at first [Citation12]. Subsequently, CD8+ T cells can eliminate HIV-1-infected cells and prevent the formation of a latent reservoir of HIV-1 [Citation13]. Early studies have explored that the emergence of HIV-1-specific CD8+ T cells plays an essential role in controlling viral infection during the acute phase of infection [Citation14,Citation15]. To date, researchers have demonstrated that dendritic cells (DCs) and CD4+ T cells also depend on the induction of HIV-1-specific immune responses [Citation16,Citation17]. In the last years, nano-platforms have been increasingly applied to nanomedicine to effectively stimulate the immune system for prophylactic and therapeutic vaccination [Citation18]. Nano-vaccine is a class of nano-based system that is used for the prophylaxis of viral infection. Nano-vaccines, including non-viral and viral vectored nano-vaccines, have been extensively exploited as vectors for targeted delivery to antigen-presenting cells (APCs), vaccine production, and gene delivery [Citation19–21]. Furthermore, nano-vaccines can improve the effectiveness of HIV-1 antigen delivery and increase the induction of innate and adaptive immune responses that are crucial for the prophylaxis of HIV-1 infection [Citation22]. In addition, compared to traditional vaccination strategies, genetic immunization can elicit not only humoral immune response but also an enduring cellular immune response in vivo to protect animals from HIV-1 infection [Citation23,Citation24].
This review focuses on nano-vaccines for gene delivery against HIV-1 infection. The literature, published on peer-reviewed journals, were systematically searched from January 2000 to December 2022. The literature search was conducted in the following databases: PubMed, Web of Science, and Embase. The research progress was made in the nano-based gene delivery systems, which can be applied to generate HIV-1-specific immune responses to provide functional insights into the development of HIV-1 vaccines.
2. Non-viral vectored nano-vaccines
Non-viral vectored nano-vaccines for gene delivery can be categorized as organic nanoparticles and inorganic nanoparticles developed to enhance immunity [Citation24,Citation25]. These non-viral vectored HIV-1 nano-vaccines offer additional adjuvant properties to conventional vaccines with several unique features including improved stability, high nucleic acid loading, controlled tunability, and surface-functionalized property [Citation26].
2.1. Inorganic nano-vaccines
Inorganic nanoparticles, such as iron, silica, calcium, gold and silver, are frequently used as carriers for nano-vaccine [Citation27]. Inorganic nanoparticles are ideal for gene delivery as vaccines against viral infection [Citation27]. Most inorganic nanoparticles possess small hydrodynamic size, controlled fashion, high antigen loadings, improved stability, minimum immuno-toxicity and responsive release profile [Citation28–31]. These inorganic nano-vaccines can facilitate immunogen delivery to APCs to modulate an effective immune activation [Citation32]. Nano-vaccines based on various inorganic nanoparticles, such as gold nanorods (GNRs) and silica nanoparticles, are actively being pursued for the prophylaxis of HIV-1 infection since the last decade (, ).
Figure 1. Different types of nano-vaccines for gene delivery used in the development of HIV-1 vaccines. (a) Gold nanorods (GNRs); (b) Silica-coated calcium phosphate nanoparticles (SCPs); (c) Poly(lactic-co-glycolic acid) (PLGA); (d) Polymethylmethacrylate (PMMA); (e) Lipid nanoparticles (LNPs); (f) Adenovirus (Ad); (g) Adeno-associated virus (AAV); (h) Lentivirus (LV); (i) Poxvirus.

Table 1. Non-viral vectored nano-vaccines against HIV-1.
Surface-engineered metal nanoparticles, such as gold, silver, and platinum, have the potential as nucleic acid vaccine delivery systems for prophylaxis or treatment against HIV-1 [Citation33]. Because of their relatively tunable surface functionalization, varying sizes, and shapes, GNRs are ideal for vaccine delivery application. In brief, GNRs are rod-like gold nanoparticles with scales ranging from a few nanometers to hundreds of nanometers, possessing rich physical and chemical properties. Xu et al. investigated novel surface-engineered GNRs used as promising DNA vaccine nanocarriers delivery system against HIV-1 infection () [Citation34]. The GNRs-based vaccine was exploited through surface chemistry by placing three kinds of molecules. The surface of GNRs was modified with cetyltrimethylammonium bromide (CTAB), poly(diallydimethylammonium chloride) (PDDAC), and polyethyleneimine (PEI), which were termed PDDAC-Au NR-Env. The authors’ previous research suggested that PDDAC-Au NR-Env showed low toxicity and better internalization [Citation35]. Mice were immunized with PDDAC-Au NR-Env through intradermal injection. The ELISPOT assay demonstrated that the IFN-γ secretion level of PDDAC-Au NR-Env group was enhanced significantly compared with the naked Env pDNA group. Then, T cell proliferation assay showed that the PDDAC-Au NR-Env group exhibited significantly higher CD4+ and CD8+ T cell proliferation abilities compared with the naked Env pDNA group. In addition, the PDDAC-Au NR-Env group (nearly 8 times, titer-1:25,600) and PEI-Au NR-Env pDNA group (nearly 4 times, titer-1:12,800) elicited significantly higher Env-specific antibody titers compared to the naked Env pDNA group (titer-1:3200). The Th1 and Th2 cells elicit the generation of IgG2a and IgG1, respectively. Compared with the value of IgG1/IgG2a in the naked Env pDNA group, the value in the PDDAC-Au NR-Env group was significantly enhanced, indicating a Th2-biased immunity. As DCs were incubated with PDDAC-Au NR-Env complex, the proportion of mature DCs increased significantly compared with the uncultured group. The results clearly investigated that surface-engineered GNRs could significantly elicit ultimate immune responses through activating APCs in contrast to DNA vaccine encoding Env, demonstrating that the surface chemistry largely determined the self-adjuvant characteristics of GNRs [Citation34]. The promising results exhibited the appropriate strategy of inorganic nanoparticles as feasible nano-platforms for nucleic acid delivery [Citation36,Citation37].
Figure 2. Schematic illustrations of inorganic nano-vaccines for gene delivery against HIV-1. (a) The surface of GNRs was modified with CTAB, PDDAC, PEI, and pDNA. After the uptake of GNRs complexes, APCs, especially DCs, can phagocytose the GNRs complex and process the antigens. (b) The surface of calcium phosphate nanoparticles was modified with PEI, CpG, and pDNA. After the uptake of SCPs complexes, APCs, especially DCs, can be activated.

As a classic type of inorganic vaccine delivery systems, calcium phosphate nanoparticles are promising nano-platform candidates for gene delivery because of their good biodegradability and biocompatibility. Calcium phosphate nanoparticles have tunable size and good affinity to DNA and RNA and can also be surface-functionalized with different molecules. We have explored CpG-functionalized silica-coated calcium phosphate nanoparticles (SCPs) for efficiently delivering DNA-based HIV-1 trimeric Env vaccines for the prophylaxis of HIV-1, which were termed SCPs-CpG/pDNA [Citation38]. Calcium phosphate nanoparticles encapsulated with silica was a synthesized design to protect nucleic acid from biodegradation (). In addition, the pDNA encoding HIV-1 SOSIP.664 fused to bacteriophage T4 fibritin foldon motif or GCN4-based isoleucine zipper was chosen as native-like trimeric HIV-1 vaccines. Soluble BG505 SOSIP.664 gp140 is a kind of stable native spike that can induce neutralizing antibodies against HIV-1 [Citation39]. The SCPs-CpG/pDNA (s.c.) group (3.99 (±2.34) × 105) showed significantly higher antibody titers than the naked pDNA group. Both IL-4 SFCs and IFN-γ SFCs were significantly increased in the SCPs-CpG/pDNA (s.c.) vaccination groups compared to the PBS group, illustrating the elicitation of both Th1 and Th2 immune responses. The DCs in the SCP-CpG/pDNA groups exhibited significant upregulation of CD40, CD80, and CD86 compared to those in the PBS group, demonstrating the maturation-eliciting effect mediated by CpG-functionalized carriers [Citation38]. The results suggested that SCPs-mediated genetic immunization was able to significantly elicit potent cellular immune response and broad humoral immune response in contrast to pDNA immunization, demonstrating the feasibility of CpG-functionalized SCPs for delivering nucleic acid vaccines expressing a native-like HIV-1 Env [Citation38].
To sum up, inorganic nano-vaccines are systems that prevent premature antigen release and prolong antigen presentation for potent immunity against viral infectious diseases. Nevertheless, inorganic nano-vaccines have some limitations against viral infectious diseases, such as high cellular toxicity, low biocompatibility, and lack of biodegradability. The safety of inorganic nano-vaccines against HIV-1 needs to be improved and better optimized.
2.2. Organic nano-vaccines
A huge number of organic nanoparticles have been explored as nano-vaccine platform for gene delivery due to their biocompatibility, biodegradability, targeted delivery, low toxicity, and enhanced immune potentiation [Citation40–43]. Among different nanoparticle delivery systems, most organic nanoparticles (e.g. polymeric nanoparticles, liposomes, and virus-like particles) possess many advantages, including self-assembly in the presence of nucleic acids and adjuvants, APC activation and T-cell activation [Citation44].
Polymerized nanoparticles can be defined as nano-sized biodegradable polymers of natural, synthetic, or semi-synthetic origin. Polymeric nanoparticles are very promising candidate delivery systems and adjuvants for numerous antigens [Citation45]. Their favorability of polymeric nano-vaccines stems from their ease of biodegradability and biocompatibility, the fact that they are nontoxic and non-immunogenic [Citation46]. A variety of different polymeric nanoparticles exist, but the most frequently encountered types include poly(lactic-co-glycolic acid) (PLGA), polymethylmethacrylate (PMMA), and lipid nanoparticles (LNPs) against HIV-1 infection ().
Zhu et al. developed intestine-targeted pH-dependent Eudragit microparticles delivering HIV-1 vaccine carried by PLGA nanoparticles [Citation47]. The methacrylate-based polymer Eudragit, an anionic trimer, is pH-sensitive and soluble in intestinal fluids in the neutral pH environment, seen only in the terminal ileum to prevent the contents from being released too early [Citation48]. In brief, PLGA nanoparticles delivering PCLUS3-18IIIB and Toll-like receptors were encapsulated into Eudragit microparticles. The PLGA-coated vaccine elicited efficient clearance of HIV-1 after intra-colorectal challenge and intravaginal challenge, indicating delivery to the large intestine was effective in protecting against both genital and rectal challenges. In addition, IgA and IgG antibody responses were activated by such a vaccine regimen in both the large intestine and vaginal tracts. These results showed that Eudragit significantly elicited colorectal immune response after vaccination and showed protective effectiveness against vaginal and rectal HIV-1 challenges. Therefore, smart polymers are promising to elicit mucosal immune response and deliver HIV-1 vaccines to targeted organs.
Polymethylmethacrylate (PMMA)-based nano-platforms have been studied to deliver HIV-1 Tat and Gag DNA vaccines [Citation49]. These nanoparticles have a core-shell structure with an inner core based on PMMA and an outer shell made of poly(ethyleneglycol) chains. The nanoparticles are adsorbed on a large amount of nucleic acid through electrostatic interaction. This PMMA-based nano-platform has advantages of good biocompatibility, biodegradability, stability, and low toxicity. These PMMA-based nanoparticles delivering HIV-1 Tat DNA vaccine via intramuscular vaccination significantly induced increased Th1-type immunity and cytotoxic T lymphocyte response compared to naked Tat DNA vaccine. In addition, PMMA-based nanoparticles delivering HIV-1 Gag DNA vaccine via intranasal vaccination showed significantly induced HIV-1-specific IFN-γ production in contrast to naked DNA immunization. After a second Tat protein boost, a potent increase of anti-HIV-1 Tat IgG titer was observed in mice primed with nanoparticles (74,191 ± 85,967) and with naked tat DNA (247,314 ± 241,957), because nanoparticles induced a Th1-type immune response in vivo [Citation49]. The PMMA nanoparticles were able to increase the stability of the DNA vaccine and elicit potent antigen-specific immune response in mice.
Liposomal vesicles are candidate delivery systems in nano-vaccines, including unilamellar vesicles and multilamellar vesicles, with diameters ranging from 20 nm to 10 μm [Citation50,Citation51]. mRNA-based nano-vaccines have attracted a lot of attention as HIV-1 vaccines as formulated with LNPs encapsulating modified nucleoside [Citation52]. Researchers have developed LNPs for delivering nucleoside-modified mRNA encoding HIV-1 antigen in different animal models. The LNPs delivering mRNA encoding HIV-1 Env elicited significantly potent immune responses in mice [Citation53]. The LNPs delivering mRNA encoding HIV-1 gp120 induced a high magnitude of Env-specific antibody response in rhesus macaques and rabbits [Citation54]. HIV-1-specific ADCC responses were evaluated against both TV-1 and 1086C (two subtypes C HIV-1). The mean antibody titer was higher against 1086C (10,891 ± 11,520) compared to TV-1 (2774 ± 2379) [Citation54]. In addition, the currently licensed mRNA vaccines for COVID-19 are able to activate innate immune mechanisms to promote immune memory to SARS-CoV-2, demonstrating the feasibility of mRNA-based lipid nano-platforms [Citation55].
To sum up, organic nano-vaccines are systems that have great potential in the development and optimization of viral vaccines for prophylaxis. However, organic nano-vaccines have some limitations against viral infectious diseases, such as low reproducibility and drug entrapment issues. The protective efficacy of organic nano-vaccines against HIV-1 needs to be improved and better characterized.
3. Viral vectored nano-vaccines
A range of different viral vectors have been exploited as gene delivery systems against HIV-1 [Citation56]. The novel viral vector-based vaccines deliver a multiplex HIV-1 genome into the host either alone or in a prime-boost strategy [Citation57]. Numerous potential advantages of viral vector-based HIV-1 nano-vaccines have shown considerable efficacy, such as long-term immunity, efficient transduction, high vaccine stability, large-scale manufacturing, and immunogen production [Citation58]. Adenovirus (Ad), adeno-associated virus (AAV), lentivirus (LV), and poxvirus possess various advantages for the construction of HIV-1 nano-vaccines (, ). Viral vectored construct consists of a promoter, transgene, and regulatory elements that enable packaging into a vector. The recombinant viral vector is used to deliver transgene to the targeted cells ().
Figure 3. Transduction pathway of viral vectored nano-vaccines for gene delivery against HIV-1. The details of the trafficking pathway are not entirely clear. Viral vectors are thought to trigger internalization by endocytosis. The viral particles are transferred to the nucleus via the nuclear pore complex. In the nucleus, viral DNA is released by uncoating, followed by transcription and exporting messenger RNA for translation. The product of gene expression elicits HIV-1-specific immune responses after release.

Table 2. Viral vectored nano-vaccines against HIV-1.
3.1. Adenoviral vector-based nano-vaccines
Adenoviridae is a family of viruses with non-enveloped, icosahedral virions containing linear dsDNA genomes of 25–48 kb [Citation59]. Several Ads are currently being developed as potential HIV-1 vaccine candidates that rely on recombinant adenoviruses (rAds) to deliver HIV-1 immunogens [Citation60]. The Ads possess attractive properties as viral vectors for nano-vaccine development, including efficient infection of various types of cells, low pathogenicity, strong immunogenicity, excellent biosafety, transgene incorporation capacity, and ease of manufacture and administration [Citation61]. Of the current serotypes of Ad, human serotypes 2 and 5 have been the most prevalent gene delivery vectors. The Ad vectors tend to induce strong innate immune response by intravenous administration, and 90% of vector DNA is cleared in circulation within 24 h. The innate immune response is dose-dependent and independent of the activation state of the compartments. The Ad vectors interact with fragments of the complement component C3 or activates the complement of immunized individuals via antibodies [Citation62]. The rAds have been widely developed as vaccines delivering antigenic gene for the prophylaxis of HIV-1 [Citation63].
Several reports revealed that rAd5-based vaccines could induce effective immune response and protect non-human primates (NHPs) against SIVmac251 challenge [Citation64,Citation65]. Among SIVmac251-infected NHPs, 50% of the vaccinated monkeys were protected from SIVsmE660 infection. In contrast to rAd5, rAd26 induced lower levels of Ad-neutralizing antibodies [Citation66]. Detectable Ad-neutralizing antibodies occurred to 98% recipients at 14 days post vaccination. Researchers have exploited a prime-boost vaccination approach with a rAd26 encoding Env/Gag/Pol prime and a rAd26 encoding gp140 boost in phase I/II trials [Citation67]. It has induced strong Env-specific cytotoxic T cell (CTL) response, antibody-dependent cellular phagocytosis response, and humoral immune response in diverse populations of immunized hosts. In another phase I trial, regimens based on Ad26.ENVA.01 prime-Ad35/ENV boost elicited significant cellular and humoral immune responses in nearly all participants [Citation68]. Moreover, boosted vaccinations significantly elicited HIV-1-specific antibody titers (geometric mean titer, 4696 vs. 2274) in all regimens. Thus, for the elicitation of HIV-1-specific cellular immunity and humoral immunity, especially T-cell immune response, rAd-based nano-vaccines are promising candidates for the prophylaxis of HIV-1 infection.
The phase IIb clinical trials (HVTN502, HVYN503, and HVTN505) assessed the efficacy of rAd5-based HIV-1 preventive vaccine [Citation69–71]. In the HVTN502 trial, 3% vaccine recipients became HIV-1 infected versus 3% placebo recipients [Citation69]. The HVTN502 showed that MRKAd5 HIV-1 Gag/Pol/Nef vaccine promoted immune cells to attack HIV-1, but this cell-mediated immunity vaccine did not prevent HIV-1 infection or reduce the early viral level. In the HVTN503 trial, 16% vaccine recipients had HIV-1 infection compared with 9% placebo recipients at a median follow-up of 42 months [Citation70]. The risk of HIV-1 acquisition in Ad5 Gag/Pol/Nef vaccine recipients was increased, suggesting further research on the biological mechanism is necessary. Results of the HVTN505 trial based on rAd5 HIV-1 Env/Gag/Pol were similar to HVTN 502 and HVTN 503, with increased susceptibility to infection detected in HIV-1 high-risk populations [Citation71]. All three trials were discontinued due to the increased risk of infection. Although these results are not ideal, other novel vaccine strategies in the field are still being investigated.
3.2. Adeno-associated viral vector-based nano-vaccines
AAV is a type of small, nonenveloped, single-stranded DNA parvovirus containing a genome of ~4.7 kb [Citation72]. Eleven AAV serotypes, including the common serotypes 1, 2, 3, 4, 5, 7 and 8, have been isolated mainly from humans or NHPs so far [Citation73]. Recombinant adeno-associated virus (rAAV) vector has proven to be an efficient nano-platform for prophylaxis or treatment against HIV-1 in preclinical and clinical studies [Citation74]. It has been reported that AAV5-based vectors encompassing gp160 gene could efficiently transduce DCs and induce potent HIV-1-specific humoral immunity and cellular immunity in vivo [Citation75]. Up to 96.5% of DCs were transduced by the AAV5 vector as the dose of the vector increased.
Serotype 8 of rAAV (rAAV8) vectors possesses many advantages over other delivery platforms, including high affinity toward skeletal muscles, high virus titers, and efficient gene delivery [Citation76]. We have evaluated the feasibility of bispecific broadly neutralizing antibodies gene delivery mediated by rAAV8 for continuous expression [Citation77]. Our results demonstrated that rAAV8-based immunization could maintain a high level of neutralizing antibody titers for 24 weeks. Furthermore, rAAV platforms have been exploited as gene delivery vectors in several clinical trials against HIV-1, demonstrating the feasibility of rAAV-based platforms [Citation78]. Currently, two clinical trials on broadly neutralizing antibodies AAV gene delivery are available. The first one uses an rAAV1 vector encoding PG9 heavy and light chains under two isolated promoters (NCT01937455) [Citation79]. This clinical trial examined the safety and efficacy of PG9 delivery through an rAAV1 vector. Non-HIV infected men aged 18–45 were administered with rAAV1-PG9 via intramuscular administration. The clinical results exhibited that the AAV caused no adverse side effects on participants, and immunohistochemical assays indicated detectable IgG within muscle cells and extracellular tissues. The second clinical trial uses an rAAV8 vector encoding the VRC07 transgene (NCT03374202) [Citation80]. This clinical trial tested the safety and efficacy of VRC07 delivery using an rAAV8 vector to HIV-1-infected adults aged 18–60. The concentration of VRC07 antibody was up to 1 μg/mL and maintained well over a year by intramuscular injection. Neutralizing activity was detected in the trial volunteers, representing that antibodies produced by rAAV8-VRC07 retained their activity in humans. This trial firstly suggested a long-term systemic production of broadly neutralizing antibodies in humans, demonstrating strong evidence for the potential of vectored delivery systems. Both clinical trials showed that rAAV delivery of broadly neutralizing antibodies is safe and capable of long-term antibody expression following a single intramuscular administration.
3.3. Lentiviral vector-based nano-vaccines
Lentiviruses are RNA viruses that belong to the retroviridae family [Citation73]. In recent years, LV-based vector has been recognized as a robust vaccine platform for durative and efficient gene delivery in different animal models [Citation81]. The LVs can transduce into both dividing and nondividing cells, including DCs and macrophages [Citation82,Citation83]. The LV-based vaccine platforms have been extensively evaluated for gene delivery against HIV-1, prompting their application as clinical HIV-1 nano-vaccines [Citation84].
Several studies have evaluated that LVs encoding HIV-1 Gag/Rev/Env transduced DCs in vitro and in vivo for anti-HIV-1 prophylactic or therapeutic vaccination [Citation85]. The DCs infected with LV-based vector effectively induced CTL response and gp120-specific binding antibody response in all these model systems [Citation86–88]. These results demonstrated that efficient LV-based delivery system was responsible for the induction of potent CTL response and binding antibody response against HIV-1. HIV-1-specific IFN-γ-producing cells (1472.5 SFCs per 106 cells) showed a 17.8-fold increase over the control. HIV-1-specific lysis was observed at ratios of effector cells to target cells with 50:1, 25:1, and 12.5:1. In addition, RNA interference technology has been used in LV-based delivery system to develop therapeutic and prophylactic vaccines against HIV-1 [Citation89]. Several groups have evaluated that HIV-1 replication can be abrogated when HIV-1-specific siRNA duplexes are introduced using LV-based system [Citation90]. The LV expression system was able to induce macrophages to stably express shNef366 [Citation91]. Meanwhile, HIV-1 replication in cells was significantly inhibited for at least 3 weeks, demonstrating that LV-based gene delivery system can substantially reduce HIV-1 infection [Citation91].
THERAVECTYS was the first company to launch a clinical trial using an LV vector against HIV-1 (NCT02054286) [Citation92]. An LV vector encoding portions of HIV-1 Gag/Pol/Nef was intramuscularly injected twice in 38 HIV-1-infected volunteers. This trial demonstrated both safety and high immunogenicity of LV vectors in human with CD4+ and CD8+ T cell responses to multiple vaccine-associated epitopes. These CD4+ and CD8+ T cell responses were multifunctional as the production of multiple cytokines persisted for up to 24 weeks.
3.4. Poxviral vector-based nano-vaccines
Poxviridae are a family of double-stranded DNA (dsDNA) viruses with very large genomes [Citation73]. Poxvirus vectors possess attractive advantages as viral vector-based vaccine platforms, such as packing flexibility of genome, low cost, rapid production, and lack of genomic integration in the host [Citation93]. A range of poxvirus-based vectors have already been explored to deliver HIV-1 genes in clinical trials, such as the modified vaccinia virus Ankara (MVA) [Citation94], vaccinia virus TianTan [Citation95], the canarypox strain (ALVAC) [Citation96], and the New York vaccinia virus (NYVAC) [Citation97]. In contrast, ALVAC vaccine exhibited the highest protection in preventing HIV-1 infection.
Currently, a range of strategies have been taken to increase the immunogenicity of poxviral vector-based vaccines [Citation93]. The MVA-based vectors are usually applied in prime-boost strategies with heterologous viral vectors, including Ads [Citation98], vesicular stomatitis virus [Citation99], and other poxvirus-based vectors [Citation100]. Recently, a clinical test explored a NYVAC vector prime and Env protein boost strategy, resulting in a high magnitude of IgG response against the V1/V2 region with long-lasting immunity (HVTN 096) [Citation101]. IgG response reached the highest level against all antigens (74–100% overall) at 2 weeks after the month 3 vaccination. The results exhibited that the NYVAC prime and Env protein boost vaccine was more immunogenic than the NYVAC vector alone. Binding antibody responses were detected 6 months after the month 6 vaccination in all study groups: responses ranged from 58% to 81%. The vaccine regimens assessed in this trial were all immunogenic, with T-cell responses and antibody responses that were higher in the regimens containing the DNA vector.
4. Immunity and challenges to HIV-1
Nano-vaccines can improve HIV-1 antigen bioavailability and elicit innate and adaptive immune responses, such as the activation of DCs, the activation of B cell, the induction of neutralizing antibodies and the induction of cell-based immunity (). Immunological advantages of nano-vaccines have contributed to their success, including the ability to deliver HIV-1 antigenic genes to targeted immune cells, the ability to activate DCs, the up-regulation of CD4+ and CD8+ T cell levels, and the ability to activate B cells for eliciting humoral immune response.
Figure 4. The presentation mechanisms of nano-vaccines for induction of immune responses against HIV-1. Nano-vaccine is transfected into target cells, followed by gene transcription and synthesis of encoded proteins. HIV-1 antigens are presented by APCs via MHC I molecules either directly transfecting vaccines or presenting by other cells. HIV-1 antigens are also presented on MHC II molecules when transfected cells secrete encoded proteins. Subsequently, APCs activate T cells by presenting antigens using MHC I and T cell receptors to induce HIV-1-specific T-cell immune responses. Otherwise, antigens are presented to CD4+ T cells via the MHC II pathway, inducing HIV-1-specific B cell responses.

4.1. Activation of dendritic cells and cross-presentation
Pattern-recognition receptors, such as Toll-like receptors, are expressed in DCs and related to DC maturation and the generation of inflammatory cytokine [Citation102–104]. Pattern-recognition receptor agonists have been exploited as adjuvants in non-viral vectored nano-vaccines to upregulate related pathways and activate DCs [Citation105]. These platforms were able to increase the MHC class II pathway, leading to enhanced B cell activation [Citation34,Citation106]. In addition, some viral vectored nano-vaccines can efficiently transduce DCs without adjuvant to induce HIV-1-specific immune responses [Citation75,Citation82,Citation83]. In contrast, naked DNA vaccines are not targeted to DCs in most cases that most of the DCs and macrophages are not affected due to their poor uptake of these vaccines [Citation23].
4.2. Activation of B cell and humoral response
IgG titers are closely related to the efficacy of vaccines [Citation107]. The application of conventional naked vaccines for genetic immunization could be hard to consummate because of their inability to stimulate DCs. Nano-vaccines have been proven to elicit a high magnitude of IgG titers against HIV-1, probably because of their advantages of targeted delivery and immune cells activation [Citation108]. Nanoparticles of less than 200 nm can enter into the initial lymphatic vessels, migrate to lymph nodes, and activate follicular B cells, while nanoparticles at 200–500 nm are delivered to the follicular areas of lymph nodes with the help of DCs [Citation109]. Nano-vaccines have been designed for the elicitation of HIV-1-specific humoral immune response focus on the presentation of different antigens of HIV, such as Env, Gag, Pol, Nef or a combinatorial strategy of them [Citation110]. These viral structural proteins including polyproteins are proven to be crucial for eliciting humoral immune response [Citation110,Citation111].
4.3. Induction of cell-based immunity
An ideal vaccine strategy will likely induce complex immunities rather than simple antibody response, such as a combination of cellular immunity and humoral immunity. The presentations of endogenous and exogenous antigens on MHC class I molecules and MHC class II molecules by DCs, are essential for the induction of HIV-1-specific CD4+ and CD8+ T cell responses [Citation112]. As for naked DNA vaccines, DC stimulation to elicit CTL response is a key obstacle that affects the level of cellular immune response. Both non-viral and viral vectored nano-vaccines have been demonstrated to trigger HIV-1-specific cell-based immunity [Citation113]. Recently, LNPs delivering mRNA vaccines have been explored to induce robust CD4+ and CD8+ T cell responses in vivo [Citation52,Citation114]. Lipid nanoparticle-based mRNA encoding a tetravalent vaccine was able to induce robust Env-specific CD4+ and CD8+ T cell responses in vivo [Citation115]. As for viral vectored nano-platforms, comparative preclinical experiments have evaluated that viral vectors, such as Ad and LV vectors, are effective strategies for inducing cytotoxic T lymphocyte immune response against HIV-1 [Citation116,Citation117].
5. Conclusion and prospects
Despite years of work, a licensed vaccine against HIV-1 has yet to be created due to intricate structural features of HIV-1. Ideal HIV-1 vaccines will be able to elicit complex immunity to protect the host from HIV-1 infection. The major challenges to a successful HIV-1 vaccine for genetic immunization are antigen design and gene delivery. Nano-vaccines, including non-viral and viral vectored nano-vaccines, offer a potential strategy for HIV-1 gene delivery. These novel nano-platforms are now being explored to improve immunization strategies to elicit HIV-1-specific humoral immunity and cellular immunity in preclinical and clinical studies. There are still challenges to be solved for further increasing delivery efficiency of HIV-1 nano-vaccines in the future. We are optimistic that nano-vaccines for gene delivery play critical roles in the development of HIV-1 vaccines.
6. Expert opinion
Prophylaxis of HIV-1 infection remains a major challenge due to the absence of an available HIV-1 vaccine. The ideal HIV-1 vaccines should elicit complex immune responses to protect the host from HIV-1 infection. The incapability of conventional delivery strategies to elicit potent immune responses is a critical task to overcome and finally lead to a major obstacle in the research of HIV-1 prevention. Nano-platforms-based vaccines have used for effectively activating the immune system in prophylaxis of various diseases. Nano-vaccines are in a position to improve the effectiveness of HIV-1 antigen delivery and enhance the innate and adaptive immune responses against HIV-1. Genetic immunization can elicit a long-term immune response to provide protective immunity for HIV-1 prevention compared with traditional vaccination strategies. Nano-vaccines are able to offer potential strategies for HIV-1 gene delivery. Vaccine strategies based on nano-platforms for gene delivery that are being applied to elicit effective HIV-1-specific humoral and cellular immune responses were particularly valued. These novel nano-platforms are now being conducted to increase immune responses to elicit HIV-1-specific humoral immunity and cellular immunity in preclinical and clinical studies.
Over the years, there has been significant progress in the use of nano-vaccines. Both non-viral and viral vectored nano-vaccines offer unique advantageous properties as vaccine strategies. Inorganic nano-vaccines have smaller particle size, improved stability and controlled surface functionalization [Citation28–31]. However, the safety of inorganic nano-vaccines against HIV-1 needs to be better improved [Citation118]. Organic nano-vaccines are biocompatible, biodegradable, and nontoxic [Citation27]. Nevertheless, the protective efficacy of organic nano-vaccines against HIV-1 needs to be better characterized [Citation47]. Viral vectored nano-vaccines have numerous potential advantages, including long-term immunity, efficient transduction, high vaccine stability, large-scale manufacturing, and immunogen production [Citation58]. However, some viral vectors are not able to accommodate large heterologous inserts of vaccine antigens [Citation119]. The protection of viral vectored nano-vaccines against HIV-1 still needs to be better improved.
In the future, there are still challenges to be solved for further increasing delivery efficiency of HIV-1 nano-vaccines, such as antigen design and gene delivery. The challenge for HIV-1 antigen design is to elicit broadly neutralizing antibodies that can induce protection against heterologous neutralization-resistant viruses. Focusing on the response to these broadly neutralizing epitopes is one of the main challenges for developing an HIV-1 vaccine. Knowing the required neutralizing epitopes will help optimize the presentation of HIV-1 immunogen to protect against heterologous virus challenges. Moreover, immunomodulatory proteins can also be designed to induce transiently boost immune responses following vaccination. Nano-platforms possess advantages of targeting APCs and improving antigen uptake as well as immunostimulatory features of nanocarriers themselves. Nano-platforms are able to prevent premature antigen release and prolong antigen presentation for effective immunity against HIV-1. Nevertheless, more nano-platforms should be explored to increase their transfection and delivery efficiency for improving immunization strategies. Nanoparticles are needed to develop to stabilize HIV-1 immunogens for optimal immune triggering. Furthermore, a greater understanding of molecular mechanisms of immune activation needs to be further explored to improve the immunostimulation ability of nano-vaccines. In addition, we still do not know if nano-vaccines will cause some level of long-term toxicity. Some possible local or systemic damage should be further explored. A promising HIV-1 vaccine will likely employ nano-platforms for optimal immunogenicity, but additional study is vital to exploit them to their full potential. It is also essential to consider the manufacturability of nano-vaccines, as economic and easy scaling up in an industrial setting as well as reproducibility are key considerations in translating them into the clinic. The optimization of high-throughput and scale-up synthesis methods to produce uniform, repeatable nanoparticles in a cost-effective manner remains a challenge.
Overall, the field of nanotechnology will continue to address the challenges that remain in immunology and provide novel strategies for future HIV-1 vaccine design. Thus, we should expect significant advances against HIV-1 in the coming years.
Article highlights
Nano-vaccines can improve the effectiveness of HIV-1 antigen delivery and increase the induction of innate and adaptive immune responses that are crucial for the prophylaxis of HIV-1 infection.
Genetic immunization can elicit not only humoral immune response but also an enduring cellular immune response in vivo to protect animals from HIV-1 infection.
Nano-vaccines for HIV-1 gene delivery offer a potential strategy to improve HIV-1-specific humoral immunity and cellular immunity.
Declaration of interests
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
S Li conceived and drafted the manuscript; MY Zhang and J Yuan reviewed the manuscript; YX Zhang revised the manuscript. All authors have read and approved the submitted version.
Additional information
Funding
References
- Rodriguez-Izquierdo I, Sepulveda-Crespo D, Maria Lasso J, et al. Baseline and time-updated factors in preclinical development of anionic dendrimers as successful anti-HIV-1 vaginal microbicides. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2022 May;14(3).
- Ndhlovu ZM, Kamya P, Mewalal N, et al. Magnitude and kinetics of CD8(+) T cell activation during hyperacute HIV infection impact viral set point. Immunity. 2015 Sep 15;43(3):591–604.
- Kim PS, Read SW. Nanotechnology and HIV: potential applications for treatment and prevention. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2010 November-December 2(6):693–702.
- Schmitz JE, Kuroda MJ, Santra S, et al. Control of viremia in simian immunodeficiency virus infection by CD8(+) lymphocytes. Science. 1999 Feb 5;283(5403):857–860.
- Ding H, George S, Leng XI, et al. Silk fibers assisted long-term 3D culture of human primary urinary stem cells via inhibition of senescence-associated genes: potential use in the assessment of chronic mitochondrial toxicity. Mater Today Adv. 2022 Aug;15. DOI:10.1016/j.mtadv.2022.100261
- Goonetilleke N, Liu MKP, Salazar-Gonzalez JF, et al. The first T cell response to transmitted/founder virus contributes to the control of acute viremia in HIV-1 infection. J Exp Med. 2009 Jun 8;206(6):1253–1272.
- Gulick RM, Flexner C. Long-acting HIV drugs for treatment and prevention. In: Klotman ME, editor. Annual Review of Medicine. 2019;70:137–150.
- Janes HE, Cohen KW, Frahm N, et al. Higher T-cell responses induced by DNA/rAd5 HIV-1 preventive vaccine are associated with lower HIV-1 infection risk in an efficacy trial. J Infect Dis. 2017 May 1;215(9):1376–1385.
- Moore CB, John M, James IR, et al. Evidence of HIV-1 adaptation to HLA-restricted immune responses at a population level. Science. 2002 May 24;296(5572):1439–1443.
- Jones LD, Moody MA, Thompson AB. Innovations in HIV-1 vaccine design. Clin Ther. 2020 Mar;42(3):499–514.
- Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med. 2009 Dec 3;361(23):2209–2220.
- Burton DR, Hangartner L, Broadly neutralizing antibodies to HIV and their role in vaccine design. In: Littman DR, Yokoyama WM, editors. Annual Review of Immunology, Vol 34. Annual Review of Immunology. 2016;342016:635–659.
- Klatt NR, Shudo E, Ortiz AM, et al. CD8+ Lymphocytes control viral replication in SIVmac239-infected rhesus macaques without decreasing the lifespan of productively infected cells. PLoS Pathog. 2010 Jan;6(1):e1000747.
- Jin X, Bauer DE, Tuttleton SE, et al. Dramatic rise in plasma viremia after CD8(+) T cell depletion in simian immunodeficiency virus-infected macaques (vol 189, pg 991, 1999). J Exp Med. 1999 Jun 21;189(12):1999.
- Ogg GS, Jin X, Bonhoeffer S, et al. Quantitation of HIV-1-specific cytotoxic T lymphocytes and plasma load of viral RNA. Science (New York, NY). 1998 Mar 27;279(5359):2103–2106.
- Janssen EM, Lemmens EE, Wolfe T, et al. CD4(+) T cells are required for secondary expansion and memory in CD8(+) T lymphocytes. Nature. 2003 Feb 20;421(6925):852–856.
- Smith CM, Wilson NS, Waithman J, et al. Cognate CD4(+) T cell licensing of dendritic cells in CD8(+) T cell immunity. Nat Immunol. 2004 Nov;5(11):1143–1148.
- Sulczewski FB, Liszbinski RB, Romao PRT, et al. Nanoparticle vaccines against viral infections. Arch Virol. 2018 Sep;163(9):2313–2325.
- Petkar KC, Patil SM, Chavhan SS, et al. An overview of nanocarrier-based adjuvants for vaccine delivery. Pharmaceutics. 2021 Apr;13(4).
- Zhang J, Russell SJ. Vectors for cancer gene therapy. Cancer Metastasis Rev. 1996 Sep;15(3):385–401.
- Geng J, Xia X, Teng L, et al. Emerging landscape of cell-penetrating peptide-mediated nucleic acid delivery and their utility in imaging, gene-editing, and RNA-sequencing. J Control Release. 2022 Jan;341:166–183.
- Zaheer T, Pal K, Zaheer I. Topical review on nano-vaccinology: biochemical promises and key challenges. Process Biochem. 2021 Jan;100:237–244.
- Rezaei T, Khalili S, Baradaran B, et al. Recent advances on HIV DNA vaccines development: stepwise improvements to clinical trials. J Control Release. 2019 Dec;28(316):116–137.
- Brave A, Ljungberg K, Boberg A, et al. Multigene/multisubtype HIV-1 vaccine induces potent cellular and humoral immune responses by needle-free intradermal delivery. Mol Ther. 2005;Dec;12(6):1197–1205.
- Hajebi S, Yousefiasl S, Rahimmanesh I, et al. Genetically engineered viral vectors and organic-based non-viral nanocarriers for drug delivery applications. Adv Healthcare Mater. 2022;11(20):2201583.
- Zhao L, Seth A, Wibowo N, et al. Nanoparticle vaccines. Vaccine. 2014 Jan 9;32(3):327–337.
- Poon C, Patel AA. Organic and inorganic nanoparticle vaccines for prevention of infectious diseases. Nano Express. 2020 Jun 1;1(1):012001.
- Turner CT, McInnes SJP, Voelcker NH, et al. Therapeutic potential of inorganic nanoparticles for the delivery of monoclonal antibodies. J Nanomater. 2015;2015;2015(3):721–730.
- Dizaj SM, Jafari S, Khosroushahi AY. A sight on the current nanoparticle-based gene delivery vectors. Nanoscale Res Lett. 2014 May 21;9.
- Ren X, Geng P, Jiang Q, et al. Synthesis of degradable titanium disulfide nanoplates for photothermal ablation of tumors. Mater Today Adv. 2022 Jun;14
- Zhang L, Forgham H, Huang X, et al. All-in-one inorganic nanoagents for near-infrared-II photothermal- based cancer theranostics. Mater Today Adv. 2022 Jun;14
- Duan Y, Wang S, Zhang Q, et al. Nanoparticle approaches against SARS-CoV-2 infection. Current Opinion in Solid State & Mater Sci. 2021 Dec;25(6).
- Liu Y, Chen C. Role of nanotechnology in HIV/AIDS vaccine development. Adv Drug Deliv Rev. 2016 Aug;1(103):76–89.
- Xu L, Liu Y, Chen Z, et al. Surface-engineered gold nanorods: promising DNA vaccine adjuvant for HIV-1 treatment. Nano Lett. 2012 Apr;12(4):2003–2012.
- Qiu Y, Liu Y, Wang L, et al. Surface chemistry and aspect ratio mediated cellular uptake of Au nanorods [Article]. Biomaterials. 2010 Oct;31(30):7606–7619.
- Gupta U, Jain NK. Non-polymeric nano-carriers in HIV/AIDS drug delivery and targeting. Adv Drug Deliv Rev. 2010 Mar 18;62(4–5):478–490.
- Dykman L, Khlebtsov N. Gold nanoparticles in biomedical applications: recent advances and perspectives. Chem Soc Rev. 2012;41(6):2256–2282.
- Li S, Wang B, Jiang S, et al. Surface-functionalized silica-coated calcium phosphate nanoparticles efficiently deliver DNA-based HIV-1 trimeric envelope vaccines against HIV-1. ACS Appl Mater Interfaces. 2021 Nov 17;13(45):53630–53645.
- He L, de Val N, Morris CD, et al. Presenting native-like trimeric HIV-1 antigens with self-assembling nanoparticles [Article]. Nat Commun. 2016 Jun;7(1). DOI:10.1038/ncomms12041.
- Manatunga DC, Godakanda VU, de Silva RM, et al. Recent developments in the use of organic-inorganic nanohybrids for drug delivery. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2020 May;12(3).
- Singha S, Shao K, Ellestad KK, et al. Nanoparticles for immune stimulation against infection, cancer, and autoimmunity. ACS Nano. 2018 Nov;12(11):10621–10635.
- Bendre A, Bhat MP, Lee K-H, et al. Recent developments in microfluidic technology for synthesis and toxicity-efficiency studies of biomedical nanomaterials. Mater Today Adv. 2022 Mar;13
- Mahdi EM, Cuadrado-Collados C, Silvestre-Albero J, et al. Polymer nanocomposites functionalised with nanocrystals of zeolitic imidazolate frameworks as ethylene control agents. Mater Today Adv. 2019 Jun;2
- Poon C, Gallo J, Joo J, et al. Hybrid, metal oxide-peptide amphiphile micelles for molecular magnetic resonance imaging of atherosclerosis. J Nanobiotechnol. 2018 Nov 15;16.
- Karch CP, Matyas GR. The current and future role of nanovaccines in HIV-1 vaccine development. Expert Rev Vaccines. 2021 Aug 3;20(8):935–944.
- Date AA, Destache CJ. A review of nanotechnological approaches for the prophylaxis of HIV/AIDS. Biomaterials. 2013 Aug;34(26):6202–6228.
- Zhu Q, Talton J, Zhang G, et al. Large intestine-targeted, nanoparticle-releasing oral vaccine to control genitorectal viral infection. Nat Med. 2012 Aug;18(8):1291–+.
- Bott C, Rudolph MW, Schneider ARJ, et al. In vivo evaluation of a novel pH- and time-based multiunit colonic drug delivery system. Aliment Pharmacol Ther. 2004 Aug 1;20(3):347–353.
- Castaldello A, Brocca-Cofano E, Voltan R, et al. DNA prime and protein boost immunization with innovative polymeric cationic core-shell nanoparticles elicits broad immune responses and strongly enhance cellular responses of HIV-1 tat DNA vaccination. Vaccine. 2006 Jul 17;24(29–30):5655–5669.
- Brinkkemper M, Sliepen K. Nanoparticle vaccines for inducing HIV-1 neutralizing antibodies. Vaccines. 2019 Sep;7(3).
- Xu L, Liu Y, Chen Z, et al. Morphologically virus-like fullerenol nanoparticles act as the dual-functional nanoadjuvant for HIV-1 vaccine. Adv Mater. 2013 Nov;25(41):5928–5936.
- Mu Z, Haynes BF, Cain DW. HIV mRNA vaccines-progress and future paths. Vaccines. 2021 Feb;9(2).
- Pardi N, Hogan MJ, Porter FW, et al. mRNA vaccines - a new era in vaccinology. Nat Rev Drug Discovery. 2018 Apr;17(4):261–279.
- Pardi N, LaBranche CC, Ferrari G, et al. Characterization of HIV-1 nucleoside-modified mRNA vaccines in rabbits and rhesus macaques. Mol Ther Nucleic Acids. 2019 Apr 15;15:36–47.
- Teijaro JR, Farber DL. COVID-19 vaccines: modes of immune activation and future challenges. Nat Rev Immunol. 2021 Apr;21(4):195–197.
- Wilmschen S, Schmitz JE, Kimpel J. Viral vectors for the induction of broadly neutralizing antibodies against HIV. Vaccines. 2019 Sep;7(3).
- McCann N, O’Connor D, Lambe T, et al. Viral vector vaccines. Curr Opin Immunol. 2022 Aug;77
- Travieso T, Li J, Mahesh S, et al. The use of viral vectors in vaccine development. Npj Vaccines. 2022 Jul 4;7(1).
- Schnell MJ. Viral vectors as potential HIV-1 vaccines. FEMS Microbiol Lett. 2001 Jun 25;200(2):123–129.
- Parks CL, Picker LJ, King CR. Development of replication-competent viral vectors for HIV vaccine delivery. Curr Opin HIV AIDS. 2013 Sep;8(5):402–411.
- Kim J, Vasan S, Kim JH, et al. Current approaches to HIV vaccine development: a narrative review. J Int AIDS Soc. 2021 Nov;24(S7). DOI:10.1002/jia2.25793.
- Appledorn DM, McBride A, Seregin S, et al. Complex interactions with several arms of the complement system dictate innate and humoral immunity to adenoviral vectors [Article]. Gene Ther. 2008 Dec;15(24):1606–1617.
- Wen Z, Sun C. A zigzag but upward way to develop an HIV-1 vaccine. Vaccines. 2020 Sep;8(3).
- Letvin NL, Rao SS, Montefiori DC, et al. Immune and genetic correlates of vaccine protection against mucosal infection by SIV in monkeys. Sci Transl Med. 2011 May 4;3(81).
- Barouch DH, Liu J, Li H, et al. Vaccine protection against acquisition of neutralization-resistant SIV challenges in rhesus monkeys. Nature. 2012 Feb 2;482(7383):89–U115.
- Baden LR, Walsh SR, Seaman MS, et al. First-in-human evaluation of the safety and immunogenicity of a recombinant adenovirus serotype 26 HIV-1 Env vaccine (IPCAVD 001). J Infect Dis. 2013 Jan 15;207(2):240–247.
- Barouch DH, Tomaka FL, Wegmann F, et al. Evaluation of a mosaic HIV-1 vaccine in a multicentre, randomised, double-blind, placebo-controlled, phase 1/2a clinical trial (APPROACH) and in rhesus monkeys (NHP 13-19). Lancet. 2018 Jul 21;392(10143):232–243.
- Baden LR, Karita E, Mutua G, et al. Assessment of the safety and immunogenicity of 2 novel vaccine platforms for HIV-1 prevention. Ann Intern Med. 2016 Mar 1;164(5):313–+.
- Buchbinder SP, Mehrotra DV, Duerr A, et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet. 2008 November-December;372(9653):1881–1893.
- Gray GE, Moodie Z, Metch B, et al. Recombinant adenovirus type 5 HIV gag/pol/nef vaccine in South Africa: unblinded, long-term follow-up of the phase 2h HVTN 503/Phambili study. Lancet Infect Dis. 2014 May;14(5):388–396.
- Huang YD, Follmann D, Nason M, et al. Effect of rAd5-vector HIV-1 preventive vaccines on HIV-1 acquisition: a participant-level meta-analysis of randomized trials. PLoS One. 2015 Sep;10(9). DOI:10.1371/journal.pone.0127735.
- Sonntag F, Schmidt K, Kleinschmidt JA. A viral assembly factor promotes AAV2 capsid formation in the nucleolus. Proc Natl Acad Sci U S A. 2010 Jun 1;107(22):10220–10225.
- Krause A, Worgall S. Delivery of antigens by viral vectors for vaccination. Ther Deliv. 2011 Jan;2(1):51–70.
- Earley LF, Conatser LM, Lue VM, et al. Adeno-associated virus serotype-specific inverted terminal repeat sequence role in vector transgene expression. Hum Gene Ther. 2020 Feb 1;31(3–4):151–162.
- Xin K-Q, Mizukami H, Urabe M, et al. Induction of robust immune responses against human immunodeficiency virus is supported by the inherent tropism of adeno-associated virus type 5 for dendritic cells. J Virol. 2006 Dec;80(24):11899–11910.
- Penaud-Budloo M, Le Guiner C, Nowrouzi A, et al. Adeno-associated virus vector Genomes persist as episomal chromatin in primate muscle. J Virol. 2008 Aug;82(16):7875–7885.
- Li S, Qiao Y, Jiang S, et al. Broad and potent bispecific neutralizing antibody gene delivery using adeno-associated viral vectors for passive immunization against HIV-1. J Control Release. 2021 Oct 10;338:633–643.
- Lin A, Balazs AB. Adeno-associated virus gene delivery of broadly neutralizing antibodies as prevention and therapy against HIV-1. Retrovirology. 2018 Oct 1;15.
- Priddy FH, Lewis DJM, Gelderblom HC, et al. Adeno-associated virus vectored immunoprophylaxis to prevent HIV in healthy adults: a phase 1 randomised controlled trial [Article]. Lancet Hiv. 2019 Apr;6(4):E230–E239.
- Casazza JP, Cale EM, Narpala S, et al. Safety and tolerability of AAV8 delivery of a broadly neutralizing antibody in adults living with HIV: a phase 1, dose-escalation trial [Article]. Nat Med. 2022 May;28(5):1022–+.
- Pincha M, Sundarasetty BS, Stripecke R. Lentiviral vectors for immunization: an inflammatory field. Expert Rev Vaccines. 2010 Mar;9(3):309–321.
- Follenzi A, Santambrogio L, Annoni A. Immune responses to lentiviral vectors. Curr Gene Ther. 2007 Oct;7(5):306–315.
- Naldini L, Blomer U, Gallay P, et al. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science (New York, NY). 1996 Apr 12;272(5259):263–267.
- Gruber A, Kan-Mitchell J, Kuhen KL, et al. Dendritic cells transduced by multiple deleted HIV-1 vectors exhibit normal phenotypes and functions and elicit an HIV-specific cytotoxic T-lymphocyte response in vitro. Blood. 2000 Aug 15;96(4):1327–1333.
- Buffa V, Negri DRM, Leone P, et al. Evaluation of a self-inactivating lentiviral vector expressing simian immunodeficiency virus Gag for induction of specific immune responses in vitro and in vivo. Viral Immunol. 2006 Sep;19(4):690–701.
- Buffa V, Negri DRM, Leone P, et al. A single administration of lentiviral vectors expressing either full-length human immunodeficiency virus 1 (HIV-1)(HXB2) Rev/Env or codon-optimized HIV-1(JR-FL) gp120 generates durable immune responses in mice. J Gen Virol. 2006 Jun;87(6):1625–1634.
- Zarei S, Abraham S, Arrighi JF, et al. Lentiviral transduction of dendritic cells confers protective antiviral immunity in vivo. J Virol. 2004 Jul;78(14):7843–7845.
- Yamamoto T, Tsunetsugu-Yokota Y. Prospects for the therapeutic application of lentivirus-based gene therapy to HIV-1 infection. Curr Gene Ther. 2008 Feb;8(1):1–8.
- Morris KV, Rossi JJ. Lentivirus-mediated RNA interference therapy for human immunodeficiency virus type 1 infection. Hum Gene Ther. 2006 May;17(5):479–486.
- Scherer L, Rossi JJ, Weinberg MS. Progress and prospects: RNA-based therapies for treatment of HIV infection. Gene Ther. 2007 Jul;14(14):1057–1064.
- Yamamoto T, Miyoshi H, Yamamoto N, et al. Lentivirus vectors expressing short hairpin RNAs against the U3-overlapping region of HIV nef inhibit HIV replication and infectivity in primary macrophages. Blood. 2006 Nov 15;108(10):3305–3312.
- Toussaint H, Agaugue S, Sarry E, et al. A first-in-human phase I/II trial demonstrates the safety and the immunogenicity of a lentiviral-based therapeutic HIV vaccine eliciting potent polyfunctional multispecific CD8 and CD4 T-cell responses in HIV-infected individuals [Meeting Abstract]. Hum Gene Ther. 2015 Oct 1;26(10):A10–A10.
- Garcia-Arriaza J, Esteban M. Enhancing poxvirus vectors vaccine immunogenicity. Hum Vaccin Immunother. 2014;10(8):2235–2244.
- Baden LR, Walsh SR, Seaman MS, et al. First-in-human randomized, controlled trial of mosaic HIV-1 immunogens delivered via a modified vaccinia ankara vector. J Infect Dis. 2018 Aug 15;218(4):633–644.
- Liu C, Du S, Li C, et al. Immunogenicity analysis following human immunodeficiency virus recombinant DNA and recombinant vaccinia virus Tian Tan prime-boost immunization. Science China-Life Sciences. 2013 Jun 56(6):531–540.
- Teigler JE, Phogat S, Franchini G, et al. The canarypox virus vector ALVAC induces distinct cytokine responses compared to the vaccinia virus-based vectors MVA and NYVAC in rhesus monkeys. J Virol. 2014 Feb;88(3):1809–1814.
- Harari A, Bart P-A, Stoehr W, et al. An HIV-1 clade C DNA prime, NYVAC boost vaccine regimen induces reliable, polyfunctional, and long-lasting T cell responses. J Exp Med. 2008 Jan 21;205(1):63–77.
- Ratto-Kim S, Currier JR, Cox JH, et al. Heterologous prime-boost regimens using rAd35 and rMVA vectors elicit stronger cellular immune responses to HIV proteins than homologous regimens. PLoS One. 2012 Sep 26;7(9):e45840.
- Perdiguero B, Elena Gomez C, Garcia-Arriaza J, et al. Heterologous combination of VSV-GP and NYVAC vectors expressing HIV-1 trimeric gp145 Env as vaccination strategy to induce balanced B and T cell immune responses. Front Immunol. 2019 Dec 18;10
- Santra S, Sun Y, Parvani JG, et al. Heterologous Prime/Boost immunization of rhesus monkeys by using diverse poxvirus vectors. J Virol. 2007 Aug;81(16):8563–8570.
- Pantaleo G, Janes H, Karuna S. Safety and immunogenicity of a multivalent HIV vaccine comprising envelope protein with either DNA or NYVAC vectors (HVTN 096): a phase 1b, double-blind, placebo-controlled trial (vol 6, pg e737, 2019). Lancet Hiv. 2020 Dec;7(12):E803–E803.
- Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010 May;11(5):373–384.
- Suresh R, Mosser DM. Pattern recognition receptors in innate immunity, host defense, and immunopathology. Adv Physiol Educ. 2013 Dec;37(4):284–291.
- Zhang Y, Guo X, Yan W, et al. ANGPTL8 negatively regulates NF-kappa B activation by facilitating selective autophagic degradation of IKK gamma. Nat Commun. 2017 Dec 18;8
- Li AV, Moon JJ, Abraham W, et al. Generation of effector memory T cell-based mucosal and systemic immunity with pulmonary nanoparticle vaccination. Sci Transl Med. 2013 Sep 25;5(204).
- Du P, Liu R, Sun S, et al. Biomineralization improves the thermostability of foot-and-mouth disease virus-like particles and the protective immune response induced. Nanoscale. 2019 Dec 21;11(47):22748–22761.
- Li Y, Xiao Y, Chen Y, et al. Nano-based approaches in the development of antiviral agents and vaccines. Life Sci. 2021 Jan 15;265
- Veneziano R, Moyer TJ, Stone MB, et al. Role of nanoscale antigen organization on B-cell activation probed using DNA origami. Nat Nanotechnol. 2020 Aug;15(8):716–+.
- Bachmann MF, Jennings GT. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nat Rev Immunol. 2010 Nov;10(11):787–796.
- Agrawal L, Haq W, Hanson CV, et al. Generating neutralizing antibodies, Th1 response and MHC non restricted immunogenicity of HIV-I env and gag peptides in liposomes and ISCOMs with in-built adjuvanticity. J Immune Based Ther Vaccines. 2003 Nov;1(1):5.
- Ben Haij N, Mzoughi O, Planes R, et al. Cationic nanoglycolipidic particles as vector and adjuvant for the study of the immunogenicity of SIV Nef protein. Int J Pharm. 2012 Feb 14;423(1):116–123.
- Joffre OP, Segura E, Savina A, et al. Cross-presentation by dendritic cells. Nat Rev Immunol. 2012 Aug;12(8):557–569.
- Veldhoen S, Laufer SD, Restle T. Recent developments in peptide-based nucleic acid delivery. Int J Mol Sci. 2008 Jul;9(7):1276–1320.
- Moyo N, Vogel AB, Buus S, et al. Efficient induction of T cells against conserved HIV-1 regions by mosaic vaccines delivered as self-amplifying mRNA. Molecular Therapy-Methods Clin Devel. 2019 Mar 15;12:32–46.
- Moyo N, Wee EG, Korber B, et al. Tetravalent immunogen assembled from conserved regions of HIV-1 and delivered as mRNA demonstrates potent preclinical T-cell immunogenicity and breadth. Vaccines. 2020 Sep;8(3).
- Mealey RH, Leib SR, Littke MH, et al. Viral load and clinical disease enhancement associated with a lentivirus cytotoxic T lymphocyte vaccine regimen. Vaccine. 2009 Apr 21;27(18):2453–2468.
- Shiver JW, Emini EA. Recent advances in the development of HIV-1 vaccines using replication-incompetent adenovirus vectors. Annu Rev Med. 2004;55(1):355–372.
- Hofmann-Amtenbrink M, Grainger DW, Hofmann H. Nanoparticles in medicine: current challenges facing inorganic nanoparticle toxicity assessments and standardizations [Article]. Nanomed Nanotechnol Biol Med. 2015 Oct;11(7):1689–1694.
- Willemsen A, Zwart MP. On the stability of sequences inserted into viral genomes [Review]. Virus Evol. 2019 Jul;5(2). DOI:10.1093/ve/vez045.