ABSTRACT
Radiofrequency microneedle (RFM) is relatively safe to use for all skin types but there is still possibility of adverse events. Tram-track scarring or uniform papular eruptions is a rarely reported adverse event, but it is challenging to manage. We report a case of successful treatment of tram track scarring post RFM using a combination of light emitting diodes 640 nm and a salicylic acid peel and home treatment with a combination of azelaic acid and retinoic acid. There is still no standard therapy to treat this case. The results of clinical observations showed the lesions completely recovered in 6 months.
Background
Radiofrequency microneedle (RFM) is the treatment for various indications like skin rejuvenation, skin tightening, acne scars, acne vulgaris, axillary hyperhidrosis, cellulite, striae, alopecia, post-inflammation erythema, and rosacea. RFM technology delivers energy by needles and penetrates the skin with adjustable depth. RFM technology can cause dermis structure to heat up until 65°C until 70°C with minimal heat on the epidermis when using insulated needles. The advantage of this technology is that it has minimal downtime and does not depend on chromophore, so it is relatively safe to use for all skin types. Although for darker skin types, it is still possibility to have adverse events, such as pain, transient erythema, edema, bleeding, and post inflammatory hyperpigmentation (Citation1). In addition, there are also other effects, rarely happen but require special attention, such as tram-track scarring, remote compensatory hyperhidrosis, dysesthesia, xerosis, squamation, crusting, acne exacerbation, pustulation, and also allergic contact dermatitis (Citation2,Citation3). Tram-track scarring or uniform papular eruption is an adverse event that is rarely reported, but it is challenging to manage, and also some even mention it is irreversible (Citation3,Citation4). We report a case of the successful treatment of rare adverse events after RFM on a Fitzpatrick IV skin type patient.
Case report
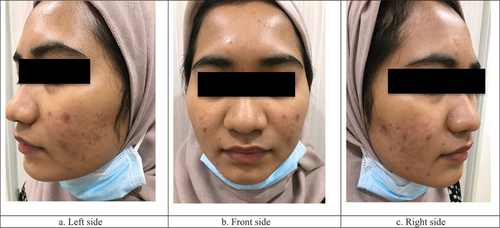
A 27-year-old woman with a history of acne vulgaris for the past 3 years. The patient has been undergoing treatment for acne vulgaris for the past 2 years. She complained about some acne scars and she also want firmer and glowing face skin. In addition, acne often recurs, especially before menstruation, but menstruation happens regularly. She works as a medical doctor and not married yet. The patient has no personal or family history of hypertrophic scars or keloids. The patient lives in Sumbawa island, eastern island from Lombok. From dermatologic examination, there were multiple erythema and hyperpigmentation macules and atrophic scars with more boxcar and rolling type than icepick scars (). The patient’s skin type is Fitzpatrick IV. The chosen treatment for atrophic acne scars was 3 session treatment with a 1-month interval using insulated bipolar radiofrequency microneedle (ENSEMBLE, BISON Medical, Seoul, South Korea). She had been undergoing treatment for acne vulgaris by using a topical regimen such as azelaic acid 20% gel and sunscreen SPF 30 every morning and adapalene 0.1% cream every night. One week before treatment, the patient stopped using the other topical regimen beside sunscreen. After signing the informed consent for a medical procedure and taking photos of the patient’s face in 3 positions, the procedure area was cleaned with 10% povidone iodine, 70% alcohol and normal saline solution. Topical anesthesia was applied for 60 minutes. Then, the patient underwent RFM with right and left cheek parameters using a needle tips with a depth of 1.5 mm with 40 watts; time 100 ms, forehead using a needle tips with a depth of 0.5 mm with 15 watts; time 120 ms and chin area using a needle tips with a depth of 0.5 mm with 30 watts; time 60 ms. All of this treatment was done on 1 pass. After treatment, the patient was given compress with normal saline solution in sterile gauzes about 15 minutes followed by the application of gentamycin cream 0.1% on the treated area after RFM. The patient was instructed to continue the application of gentamycin cream 0.1% for the next 3 days, avoid excessive sun exposure, use sunscreen SPF 30, and control 1 week after treatment by using teledermatology with WhatsApp messenger.
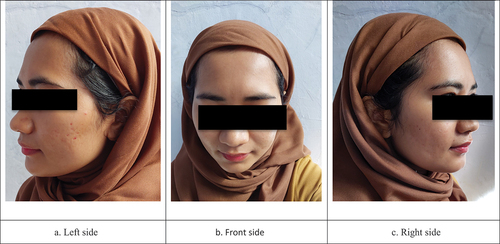
The temporary adverse events reported in this case were erythema, transient edema that happens 48 hours, post-inflammatory hyperpigmentation, and exacerbation of acne. Then, the patient was instructed to continue the previous acne treatment regimen. One month after the first session of treatment, there were multiple uniforms skin-colored papules with a needle tips pattern in the forehead area and hyperpigmented macules with a tram-track pattern that similar to the needle tips pattern on the right zygomaticus arch. The patient was assessed as uniform papular eruption (). The patient refused histopathological biopsy examination of her face. This rare adverse event was then treated using 640 nm red light therapy using light emitting diodes (LED) followed by chemical peels with 30% salicylic acid in same session, this combination were done in 2 sessions with 1 month interval. The 30 minutes LED therapy was done to cover entire face but the chemical peel only done on the tram track lesion. Both RFM sessions were continued on the others area except the forehead and the right zygomatic arch. Meanwhile, for home treatment, the patients still use a topical regimens such as retinoic acid 0,025% cream and azelaic acid 20% cream sequentially every night, and also sunscreen SPF 30 every morning. Three months after last treatment, uniform papular eruption were minimally diminished and the atrophic scar lesions showed improvement ().
Figure 2. Photo of the face 1 month after RFM treatment. Uniform papular eruptions appeared in the forehead area and hyperpigmented macules appeared with tram track pattern in the zygomatic arch area on the right side.
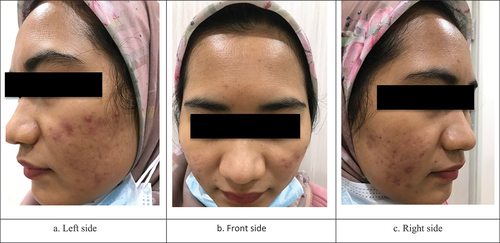
Figure 3. Photo of the face 3 month after RFM treatment, chemical peel and LED therapy completed. There was an improvement in the texture and color on patient’s skin. The lesions on the forehead were overcome.
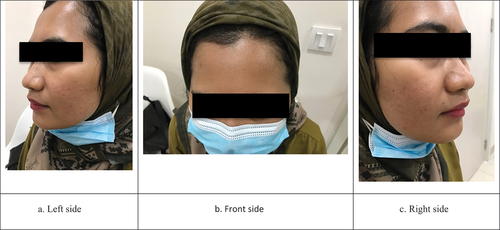
Six months after last treatment, by teledermatology, patient sent us her facial photos. At this time, the patient continued to use home treatment for maintenance and reported that the lesions on the forehead and right zygomatic arch completely recovered, improvement of atrophic scars, smoother skin texture, smaller pores and brighter looking skin ().
Discussion
Radiofrequency microneedle in this case report was using bipolar RFM with insulated needle. Bipolar RFM with insulated needles has well-known more safety than adverse events because theoretically, the RF energy in insulated needles is directly delivered to the dermis while protecting the epidermis from most of the heat from RF energy. However, there is still a small amount of energy from RF that can be delivered along with the insulation, which may be caused by a more aggressive treatment setting or breakdown of the insulation (Citation1). For after procedure care, we use normal saline solution immediately after the procedure because normal saline can be used for comforting the patient and reduce the pain (Citation5). We apply gentamicin 0.1% cream in order to reduce the risk of infection especially bacterial infection where there is a possibility of holes caused by the entry of microneedles into the skin to become the site of infection, this is also in accordance with some consensus on the use of fractional radiofrequency microneedle which considers the application of topical antibiotics for 2 to 3 days after the procedure (Citation6–9). In addition, gentamicin cream is thought to be more comfortable for her face and some references mention that gentamicin also plays a role in wound healing (Citation10–12).
Adverse events tram track scarring have been reported by previous studies as the worst side effect although they rarely happen (Citation3,Citation4). The incidence of tram track scarring has been reported at 5.6% with manual microneedling (5.6%) while RFM was 6.5% (Citation2). The clinical manifestation of tram track scarring is uniform papular eruptions or similar skin color and shape pattern from the probe device which usually happen and persists after 1 month or even until 18 months (Citation13,Citation14). The predilection sites of this occurrence are in areas with bony prominences such as the forehead, temporal, zygomatic arch, malar, and presterna (Citation13–16). There are several factors are suspected of causing this events, including the treatment area, the application of probe devices that are longer, energy density and longer exposure time, stronger pressure of the probe during the procedure, or allergies to the needle material (Citation13,Citation14,Citation16,Citation17). However, the pathogenesis is not fully understood, but tram track scarring included in the category of aberrant scarring (Citation3). The previous histopathological examination showed that the epidermis has focal necrosis with infiltration of inflammatory cells such as neutrophils, lymphocytes, and histiocytes. There was also slightly perifollicular fibrosis (Citation14).
Adverse events in RFM actually include mild and can be treated. Transient erythema, edema, pain associated with therapy usually last 2 days, post-inflammatory hyperpigmentation can last up to 10 days and can be treated with topical bleaching agents (Citation2). According to the authors’ knowledge, there is currently still no standard treatment of adverse events in RFM. There are several reports about treating the uniform papular eruption, such as using silicon gel for 6 months, 0.025% tretinoin gel for 3 months, and using 585-nm pulsed dye laser and 511/578 nm laser. All of them showed good results (Citation13,Citation14,Citation16). Also, in the future, there is more concerns to several precautions to prevent this adverse events by reducing RF energy, needle length depth and time exposure, especially in the area of the skin with bone protrusions and explaining to patients related adverse events that may occur and how to treat it. RFM treatment can still be carried out but not in areas that are still experiencing this adverse events (Citation3,Citation13,Citation18).
In this case, we chose a combination treatment of two sessions of 640 nm LED therapy followed by chemical peels with 30% salicylic acid with 1-month intervals, and for home treatments of acne vulgaris such as 0.025% retinoic acid cream and 20% azelaic acid and sunscreen SPF 30. The RFM treatment was still continued in areas other than the forehead and right zygomatic arch. Improvements were seen 3 months after the last session. Considering the use of red light 640 nm LED treatment based on research can help wound healing and suppress inflammation. This is presumably because LED therapy can reduce IL-6 mRNA levels, which has the potential to prevent aberrant healing (Citation19). Salicylic acid peel was chosen because it has antihyperplastic, anti-inflammatory, keratolytic and desmolytic effects (Citation20). The chemical peel and the red light therapy was done at the same session, but the red light therapy was done about 30 minutes prior to the chemical peel because this therapy does not cause exfoliation and/or inflammation as well as thermal injury to the skin, hence it’s able to be combined with various aesthetic procedures. LED therapy application should be done before any other procedure on a clean and dry skin so that the subsequent procedure can be done safely. In addition, several references stated that combining superficial chemical peel, in this case 30% salicylic acid, with other procedure is able to accelerate the recovery process through epidermal turnover (Citation21–23).
We consider using the combination between 0.025% retinoic acid and 20% azelaic acid because combination therapy can target several pathological processes in acne vulgaris simultaneously to get great results with synergistic effects (Citation20). The retinoids work by stimulating the proliferation of epidermal cells and the elimination of sebum in the pilosebaceous ducts, reducing inflammation in the sebaceous glands, loosening the connections between cells in the stratum corneum, thereby inhibiting keratosis (Citation24). In addition, the combination of 0.025% tretinoin cream and azelaic acid cream was reported to increase efficacy and patient’s satisfaction (Citation25).
Handling this case is a challenge for us because the patient lives on a different island and there is the policy of community activities restrictions in our area due to COVID-19 pandemic situation. Therefore, we chose combination therapy with multiple modalities and longer intervals and follow-up using teledermatology with WhatsApp messenger to treat this conditions. Teledermatology is a solution and reliable tool for remote consultations in dermatology fields, especially in this pandemic situation and WhatsApp is currently one of the most popular applications worldwide that allows its users to communicate via text, voices, photos and videos (Citation26).
Conclusion
Radiofrequency microneedle is one of the skin rejuvenation treatments for atrophic acne scars, which is currently very popular and relatively safe. The more often treatment is taken, the risk of rare adverse events will rise. Therefore, the occurrence of uniform papular eruptions or tram track scarring is rare. Still, physicians who use this technology need to recognize and know how to prevent and overcome them. Further research about the management of RFM adverse events especially in Fitzpatrick skin type IV is also needed.
Acknowledgments
The authors has no conflict of interest in this case report. There was no sponsorship in this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Weiner S. Radiofrequency microneedling: overview of technology, advantages, differences in devices, studies, and indications. Facial & Plastic Surg Clin North Amer. 2019 August;27(3):291–303. doi:10.1016/j.fsc.2019.03.002.
- Gowda A, Healey B, Ezaldein H, Merati M. A systematic review examining the potential adverse effects of microneedling. J Clin Aesthet Dermatol. 2021 January;14(1):45–54.
- Juhasz M, Cohen J. Microneedling for the treatment of scars: an update for clinicians. Clin & Cos Invest Derm. 2020 December;13:997–1003. doi:10.2147/CCID.S267192.
- Cho J. Practical use of microneedle RF for common scar and pigment. International Aesthetic Dermatology Symposium of the Association of Korea Dermatologist on KOREADERMA; 2020 Dec 17–20; Seoul, Korea.
- Singh A, Yadav SM. Microneedling: advances and widening horizons. Indian Dermatol Online J. 2016;7(4):244–254. doi:10.4103/2229-5178.185468.
- Lee S, Yeo U, Wee S, Shim J, Roh K, Lim E. Consensus recommendations on the use of a fractional radiofrequency microneedle and its applications in dermatologic laser surgery. Med Lasers. 2014 June;3(1):5–10. doi:10.25289/ML.2014.3.1.5.
- Devgan L, Singh P, Durairaj K. Minimally Invasive Facial Cosmetic Procedures. Otolaryngology Clini North Amer. 2019;52(3):443–59. doi:10.1016/j.otc.2019.02.013.
- Waghule T, Singhvi G, Dubey S. Microneedles: a smart approach and increasing potential for transdermal drug delivery system. Biomed Pharma. 2019;109:1249–58. doi:10.1016/j.biopha.2018.10.078.
- Kleidona I, Karypidis D, Lowe N, Myers S, Ghanem A. Fractional radiofrequency in the treatment of skin aging: an evidence-based treatment protocol. J Cosmet Laser Ther. 2020;22(1):9–25. doi:10.1080/14764172.2019.1674448.
- Yetim I, Ozkan O, Dervisoglu A, Erzurumlu K, Cambolant E. Effect of local gentamicin application on healing and wound infection in patients with modified radical mastectomy: a prospective randomized study. J Int Med Res. 2010;38(4):1442–47. doi:10.1177/147323001003800426.
- Varga M, Sixta M, Bem R, Matia J, Jirkovska A, Adamec M. Application of gentamicin collagen sponge shortened wound healing time after minor amputations in diabetic patients - a prospective, randomised trial. Arch Med Sci. 2014;10(2):283–87. doi:10.5114/aoms.2014.42580.
- Kwong A, Cogan J, Hou Y, Antaya R, Hao M, Kim G, Lincoln V, Chen Q, Woodley DT, Chen M. Gentamicin induces laminin 332 and improves wound healing in junctional Epidermolysis Bullosa patients with nonsense mutations. Mol Ther. 2020;28(5):1327–1338. doi:10.1016/j.ymthe.2020.03.006.
- Pahwa M, Pahwa P, Zaheer A. “Tram track effect” after treatment of acne scars using a microneedling device. Dermato Surg. 2012 July;38(7 Pt 1):1107–08. doi:10.1111/j.1524-4725.2012.02441.x.
- Suh D, Lee M, Lee S, Song K, Byun J. Prolonged inflammatory reaction after fractional radiofrequency microneedle treatment. Dermato Surg. 2018 September;44(9):1234–36. doi:10.1097/DSS.0000000000001407.
- Chandrashekar B, Sriram R, Mysore R, Bhaskar S, Shetty A. Evaluation of microneedling fractional radiofrequency device for treatment of acne scars. J Cutaneous Aesthetic Surg. 2014 April;7(2):93–97. doi:10.4103/0974-2077.138328.
- Dogra S, Yadav S, Sarangal R. Microneedling for acne scars in Asian skin type: an effective low cost treatment modality. J Cosmet Dermatol. 2014 September;13(3):180–187. doi:10.1111/jocd.12095.
- Yadav S, Dogra S. A cutaneous reaction to microneedling for post acne scarring caused by nickel hypersensitivity. Aesthetic Sur J. 2016 April;36(4):168–70. doi:10.1093/asj/sjv229.
- Ablon G. Phototherapy with light emitting diodes: treating a broad range of medical and aesthetic conditions in dermatology. J Clin Aesthet Dermatol. 2018 February;11(2):21–27.
- Arif T. Salicylic acid as a peeling agent: a comprehensive review. Clin & Cosmet Inves Dermatol. 2015August:455–61. doi:10.2147/CCID.S84765.
- Sacchidanand S, Lahiri K, Godse K, Patwardhan N, Ganjoo A, Kharkar R, Narayanan V, Borade D, Dsouza L. Synchronizing pharmacotherapy in acne with review of clinical care. Indian J Dermatol. 2017 Jul-Aug;62(4):341–57. doi:10.4103/ijd.IJD_41_17.
- Trelles M, Mordon S, Calderhead R. Facial rejuvenation and light: our personal experience. Lasers Med Sci. 2007;22(2):93–99. doi:10.1007/s10103-006-0418-6.
- Linder J. Chemical peels and combination therapies. Plastic Surgery Nursery. 2013;33(2):88–93. doi:10.1097/PSN.0b013e318294cf71.
- Simao J C L, Wambier C G. Combining Superficial Chemical Peels. In: Issa M C A, Tamura B, editors. Chemical and Physical Procedures. Springer International Publishing AG; 2018. p. 41–50.
- Zasada M, Budzisz E. Retinoids: active molecules influencing skin structure formation in cosmetic and dermatological treatments. Postepy Dermatol Alergo. 2019 August;36(4):392–97. doi:10.5114/ada.2019.87443.
- Searle T, Ali F R, Al-Niaimi F. The versatility of azelaic acid in dermatology. J Dermatolog Treat. 2020 August;33(2):722–732.
- Jakhar D, Kaul S, Kaur I. WhatsApp messenger as a teledermatology tool during coronavirus disease (COVID-19): from bedside to phone-side. Clin Exp Dermatol. 2020 August;45(6):739–40. doi:10.1111/ced.14227.