Abstract
Introduction
The European Society of Cardiology (ESC) guidelines (GL) provide indications on the mode of delivery in women with heart disease. However available data suggests that the rate of Cesarean Delivery (CD) is high and widely variable among such patients. In this study, we aimed to investigate the degree of adherence to the ESC recommendations among women delivering in four tertiary maternity services in Italy and how this affects the maternal and neonatal outcomes.
Material and methods
Retrospective multicenter cohort study including pregnant women with heart disease who gave birth between January 2014 and July 2020. Composite adverse maternal outcome (CAM) was defined by the occurrence of one or more of the following: major postpartum hemorrhage, thrombo-embolic or ischemic event, de novo arrhythmia, heart failure, endocarditis, aortic dissection, need for re-surgery, sepsis, maternal death. Composite Adverse Neonatal outcome (CAN) was defined as cord arterial pH <7.00, APGAR <7 at 5 min, admission to the intensive care unit, and neonatal death. We compared the incidence of CAM and CAN between the cases with planned delivery in accordance (group “ESC consistent”) or in disagreement (group “ESC not consistent”) with the ESC GL.
Results
Overall, 175 women and 181 liveborn were included. A higher frequency of CAN was found when delivery was not planned accordingly to the ESC guidelines [(“ESC consistent” 9/124 (7.2%) vs “ESC not consistent” 13/57 (22.8%) p = 0.002 OR 3.74 (CI 95% 1.49–9.74) , while the occurrence of CAM was comparable between the two groups. At logistic regression analysis, the gestational age at delivery was the only parameter independently associated with the occurrence of CAN (p = 0.006).
Conclusion
Among pregnant women with heart disease, deviating from the ESC guidelines scheduling cesarean delivery does not seem to improve maternal outcomes and it is associated with worse perinatal outcomes, mainly due to lower gestational age at birth.
Introduction
In the last decades an increased incidence of pregnancies in women with heart disease has been registered, contributing to the rise of cardiovascular adverse events recorded during pregnancy. Cardiovascular events are nowadays the leading cause of maternal morbidity and mortality [Citation1].
The management of maternal heart disease in pregnancy requires a multidisciplinary approach including different specialist, and in such context timing and mode of delivery is of paramount importance to improve the maternal and neonatal outcome. Recent data support the safety and the feasibility of vaginal birth in such patients [Citation2–6]. The guidelines of the European Society of Cardiology (ESC) endorse vaginal delivery in women with heart disease as this seems associated with improved maternal and neonatal outcomes, while the recommendation to planned Cesarean Delivery (CD) should be limited to obstetric indications and specific conditions such as labor onset under oral anticoagulant treatment, patients with aggressive aortic pathology, acute intractable heart failure and in the context of severe pulmonary hypertension [Citation7–8]. Nonetheless, available data suggest that the rate of CD in this cohort of women is extremely variable across the countries and, most importantly, the adherence to the ESC recommendations remains low [Citation9]. The aim of this study was to investigate the degree of adherence to the ESC recommendations among women delivering in four tertiary maternity services in Italy and how adherence to guidelines affects the maternal and neonatal outcomes.
Materials and methods
This was a multicentric retrospective cohort study involving four Italian academic tertiary maternity units (Parma University Hospital, Pisa University-Hospital, Sant’Orsola-Malpighi Hospital of Bologna, Agostino-Gemelli Foundation University Hospital of Rome). The participating units all record over 2000 deliveries per year and represent referral centers for outpatient multidisciplinary services for the management of high-risk pregnancies which include the availability of a 24-h onsite anesthesiology and neonatology service.
All women with congenital and/or acquired heart disease diagnosed before or during the pregnancy who gave birth at one of participating units between 1 January 2014 and 30 June 2020 were considered eligible for the study. From each Center women were identified through the ICD codes reported on the patient's notes. Delivery prior to 22 weeks of gestation and missing data represented exclusion criteria for the study, while cases of stillbirth were excluded from the analysis of neonatal outcomes.
Data were collected through medical records and patient case notes and included information concerning the cardiac maternal disease as classified according to the mWHO system (modified World Health Organization classification of maternal cardiovascular risk) [Citation8], the NYHA (New York Heart Association Classification) score at booking, the baseline and obstetrical characteristics, pregnancy complications including worsening of the maternal cardiovascular function (defined as the need for hospital admission, intensive care, surgery, deep venous thrombosis, ischemic events, myocardial infarction, arrhythmia, heart failure), planned mode of delivery, the actual mode of delivery and maternal and neonatal short-term outcomes. In each study center, the decision regarding the mode of delivery is taken by the multidisciplinary team mentioned above, through a comprehensive examination of both the cardiovascular and obstetric features of the woman and her pregnancy. For each case, two members of the research team (L.A. and S.F.) evaluated whether the planned mode of delivery was consistent or not with the ESC guidelines. As the ESC recommends performing a CD on cardiovascular indication only in case of labor onset under oral anticoagulant treatment, aggressive aortic pathology, acute intractable heart failure and/or in the context of severe pulmonary hypertension [Citation7–8], any other cardiological indications to delivery by CD with no obstetrical reason were considered not consistent with the overmentioned guidelines. Patients were so divided into the following two groups:
Group “ESC consistent”: including all cases in which the mode of delivery was appropriate according to the ESC guidelines.
Group “ESC not consistent”: including all cases in which the mode of delivery was not consistent with the recommendations by the ESC guidelines.
In the case of planned CD due to obstetrical reasons (such as breech delivery, placenta previa, etc), patients have been included in the “ESC consistent” group. For cases included in “ESC not consistent,” each participating unit was requested to specify which of the following was the leading indication to planned cesarean delivery: unavailability of intensive clinical and/or instrumental monitoring during labor, cardiological indication to cesarean delivery not endorsed in the ESC guidelines.
Composite adverse maternal (CAM) outcome was defined based on the occurrence in the six weeks after the delivery of at least one among major postpartum hemorrhage (>1000cc), thrombotic, ischemic or embolic event, de novo arrhythmia, heart failure, significant clinical worsening requiring urgent treatment, endocarditis, aortic dissection, cardiac arrest, need for cardiac re-surgery, sepsis, maternal death. Composite adverse neonatal (CAN) was defined in the event of at least one among cord arterial pH <7.00, APGAR <7 at 5 min, admission to the neonatal intensive care unit (NICU), and neonatal death.
A multivariable analysis has been performed and, to improve the strength of the association, only the variables significantly associated with CAN outcome were included.
Statistical analysis
The collected data were analyzed using MedCalc and SPSS software. The continuous variables were compared using Student’s t test after evaluating their distribution; categorical variables were analyzed by chi-Square or Fisher exact test where necessary. Only the variables found to be significant in the univariable analysis between the subgroups (p ≤ 0.05) were included in the multivariable logistic regression.
Results
Overall, 175 women and 181 liveborns were included in the study; summarizes the baseline and obstetrical features, maternal and neonatal outcomes of the study population. CAM outcome occurred in 11/175 (6.3%) cases and included 5 cases of major PPH, 2 cases of de novo arrhythmia, 3 cases of worsening of the underlying disease and 1 case of sepsis. There was no case of maternal death. Two cases of stillbirth have been recorded. CAN outcome occurred in 22/181 (12.1%) cases and was accounted by 3 cases of neonatal death, 10 NICU admissions and 9 cases of APGAR <7.
Table 1. Baseline and obstetrical characteristics, maternal and neonatal outcomes of the study population.
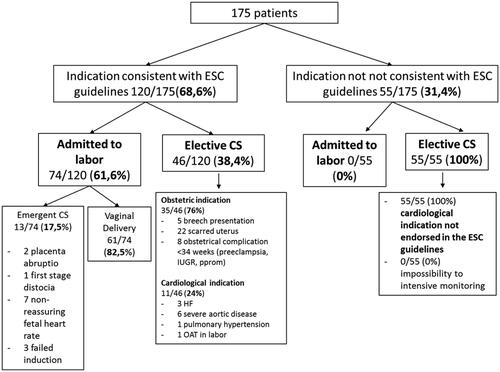
The study population in relation to the adherence to the ESC recommendations in terms of planned mode of delivery is shown in . 120/175 (68.6%) women and 124/181 (68.5%) neonates were eventually assigned to the group “ESC consistent” (planned mode of delivery consistent with ESC guidelines). In this group, 74/120 women (61.6%) were scheduled for planned vaginal delivery; among the remaining 46/120 (38.3%) women scheduled for planned cesarean delivery, 35/46 (76%) had a non-cardiologic and 11/46 a cardiologic indication (24%), which was in accordance with the ESC guidelines as herein described: acute heart failure refractory to medical therapy (3 cases), severe aortic pathology (6 cases), 1 case of labor during oral anticoagulation therapy in a patient with a mechanical valve prosthesis and 1 case of critical pulmonary hypertension. All the 55 women included in the group “ESC not consistent” were submitted to cesarean delivery, which was performed purely due to the maternal cardiac disease but not in accordance with the ESC guidelines. No cases of unavailability of intensive clinical and/or instrumental monitoring during labor have been declared. The baseline characteristics of the two groups are presented on . Among the pregnancies who were managed in accordance with ESC smaller body mass index (BMI) (25.4 ± 5.7 vs 23.4 ± 3.9, p = 0.016) and nulliparity [68/120, 56.7% vs 48/55, 87.3%, p < 0.001)] and a higher prevalence of less severe cardiac disease according to mWHO classes were noted (class I 31.7% vs 9.1%, class II 19.2% vs 14.5%, class II–III 25.8% vs 34.5%, class III 19.2% vs 34.5%, class IV 4.2% vs 10.9%, p < 0.0001). The gestational age at delivery and the birthweight were lower in “ESC not consistent” (36.5 wk ± 3.4 vs 38.24 ± 2.2, p < 0.0001 and 2580 ± 768 vs 2975 ± 607 grams, p = 0.032, respectively), however, no difference was recorded in the incidence of SGA neonates [13/120 (10.8%) vs 9/55 (16.3%), p = 0.441]. No difference in the incidence of CAM was noticed [8/120 (6.7%) vs 3/55 (5.4%) p = 0.796 OR 1.22 CI 0.34–4.43)]. The incidence CAN outcome was higher in the group “ESC not consistent” [9/124 (7.2%) vs 13/57 (22.8%) p = 0.002 OR 3.74 95% CI 1.49–9.74] ().
Table 2. Primary analysis: univariable comparison between “ESC consistent” and “ESC not consistent.”
At logistic regression analysis, the gestational age at delivery proved to be the only parameter independently associated with the occurrence of CAN outcome (OR 0.743, 95%CI 0.602–0.918, p = 0.006) ().
Table 3. Multivariatble analysis for neonatal composite adverse outcome (CAN).
Discussion
Principal findings
Our study has shown that within a population of pregnancies at risk due to maternal heart disease the delivery plan based on the underlying maternal disease is not in agreement with the ESC GL in over 30% of cases. The implementation of ESC GL regarding the mode of delivery in clinical settings does not seem to affect the maternal cardiovascular status. Within our cohort of women with heart disease indeed, the decision to proceed with a scheduled CD in absence of ESC or an obstetric indication is associated with a higher incidence of adverse perinatal events without maternal benefits. At logistic regression analysis the gestational age at birth proved to be the only parameter independently associated with worse neonatal outcome, being earlier gestational age at delivery more commonly in women submitted to planned CD whom indication was not consistent with ESC recommendations.
Comparison with previous literature
The CD rate in our study group was double compared with the value reported in Italy among unselected pregnant women (65.7% vs 33.2%) [Citation10]. This data is consistent with previous studies from other countries [Citation11–12]. The largest cohort of mothers with heart diseases has been analyzed by Ruys et al. from the ROPAC register, which included 1062 patients from more than 20 countries. In this study, the CD rate appears to be 160% higher than that of the general population [Citation2]. It is important to underline that the ESC guidelines are based on experts’ opinions [Citation5,Citation13] and on the background assumption that CD should be pursued when clinically indicated for sake of the mother or the infant since abdominal delivery per se increases the risk of infection, thrombosis, and post-partum hemorrhages [Citation14]. Some authors advocate that in pregnant women with severe cardiac illness, cesarean delivery may exert a protective role on the mother [Citation21–23]. However, there is a paucity of data on the obstetric management of women with CHD. Previous studies have focused mostly on the pregnancy outcome but not on the mode of delivery [Citation15–18], while others have investigated this latter aspect only for a specific type of cardiac disease [Citation19,Citation20]. More recently a Canadian study by Robertson et al. [Citation3] including over 550 patients with heart disease supported the feasibility and safety of vaginal delivery. In this series, the rates of CD were similar to a matched group of over 1000 patients with no cardiovascular problems. Moreover, adverse maternal cardiac events at delivery were rare (2% of pregnancies) and were not associated with the mode of delivery. Similarly, Petrus et al. [Citation6] reported an 89% rate of admission to labor in a cohort of 128 pregnant women with heart disease and an overall rate of vaginal birth of 75% with no maternal or perinatal deaths. Consistently Easter et al. [Citation4] showed a low CD rate (23.9%) and no case of elective CD based on the cardiological indication on a cohort of 270 pregnant women with heart disease: in this study, adverse cardiac outcomes were similar between planned vaginal birth and cesarean delivery groups, with no differences in adverse obstetric or neonatal outcomes in the cohort overall or in the subset of women with high-risk cardiovascular disease or a high burden of obstetric comorbidity.
The results from the ROPAC register [Citation2] also showed comparable outcomes between women admitted to a trial of vaginal delivery and the ones submitted to planned CD, with no difference in maternal mortality, and postpartum heart failure between those delivered by elective CD and those delivered by emergency CD. Some authors advocate the option of elective CD in women with severe illness since the avoidance of labor is supposed to play a protective role in women with more advanced cardiac disease [Citation21–23]. This is in contrast with the study by Easter et al. [Citation4], which reported favorable outcomes after vaginal birth even among high-risk mWHO classes. In our series, 11 patients with mWHO class ≥ III disease and 2 women with an NYHA score of 2 at the beginning of the pregnancy were admitted to labor and no cardiovascular complication was recorded during and after vaginal delivery.
A crucial point emphasized by all authors is the need for a multidisciplinary approach and detailed birth plan, which must take into account the specific risk of each pregnant woman [Citation24]. Previous studies have focused on defining predictive risk factors of adverse maternal outcomes [Citation25,Citation26], but that was not the aim of our study.
Interpretation of data
Although among pregnant women with cardiac disease clinicians are mostly prone to plan a cesarean delivery due to a presumed protective role toward the mother's health [Citation2,Citation8,Citation9], this strategy does not seem to confer any clinical benefit to the woman and may hence increase the risk of adverse perinatal outcome. Notably, in none of the women who in accordance with the ESC guidelines were allowed to reach the full term of the pregnancy and to attempt vaginal delivery a worsening of cardiovascular condition has been recorded. With respect to the mode of delivery, the ESC [7,Citation8], and the American Heart Association [Citation27] recommend that laboring mothers falling into the high-risk mWHO classes should be submitted to early instrumental vaginal delivery, as Valsalva maneuver is forbidden is such patients. In Italy where the rate of operative deliveries is low, and the use of forceps has been almost abandoned, this recommendation might lead to a higher incidence of planned Cesarean deliveries in pregnant women with CHD. Interestingly, in the aforementioned study by Easter et al. [Citation4] all women admitted to labor were allowed active pushing efforts while deterioration of maternal hemodynamic parameters related to Valsalva maneuvers was not noted. A more selective policy of operative delivery based on the standard obstetric indications and not on the presence of severe heart disease per se [Citation28], may enlarge the eligibility of such women for vaginal birth.
In our series, the gestational age at birth proved to be the only factor independently related to the composite neonatal outcome and appeared significantly lower in the group of women who were submitted to planned CD out of the ESC guidelines. An earlier gestational age at delivery in women submitted to elective CD had been reported in a previous study [Citation2], however, in this cohort, no difference in the occurrence of perinatal morbidity was recorded. Early-term compared with the full-term delivery is acknowledged to be associated with an increased risk not only of perinatal complications, but also of long-term adverse conditions in terms of autoimmune metabolic and respiratory diseases in the offspring [Citation29–33].
Clinical implications
Our data suggest that the clinical implementation of ESC guidelines regarding the mode of delivery among pregnant women with cardiac disease is desirable, as this does not seem to impact negatively on the short-term cardiovascular status of the mother and might yield better neonatal outcomes. As pregnant women with heart disease represent a relatively new cohort of patients for obstetricians, efforts need to be done to widespread the best knowledge and practice about the correct management of these patients. We believe that the implementation of the appropriate obstetric management would require the joint work of different specialists in the context of a multidisciplinary team, therefore pregnant women with heart disease should be referred to dedicated Maternity units with special interest and expertise in this field. Furthermore, clinicians should be aware of the adverse impact on the perinatal outcomes of both early timing of birth and planned abdominal delivery when these are not clinically indicated.
Strengths and limitations
The main strength of the study is that this is to our knowledge the first study investigating the adherence to the ESC guidelines regarding the mode of delivery in a large clinical setting and analyzing their impact on short-term maternal and neonatal outcomes.
The main limitations of our study are represented by its retrospective design and by the relatively small number of included cases and adverse events. Moreover, the small number of women included has not allowed us to evaluate if obstetric management in accordance with the ESC guidelines would impact on the incidence of adverse maternal events which are known to be much more rare than neonatal adverse outcomes. Finally, the limited size of the study population has not permitted to compare the outcome of treatment groups (ESC vs non-ESC based) according to mWHO classes and to NYHA score of the cardiac disease.
Conclusion
Our study has shown that in the Italian territory, the clinical implementation of the ESC guidelines regarding the obstetric management of pregnancies with maternal cardiac disease is still suboptimal. In these women, the high rate of CD based on inappropriate cardiological indications and scheduled at earlier gestational ages carries a negative impact on perinatal outcomes with no clear maternal benefit. The centralization of these pregnancies to highly specialized centers must be pursued to minimize the occurrence of adverse events. Further studies are needed to confirm the potential benefits of adopting the ESC guidelines in the obstetric management of this cohort of patients.
Ethical approval
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- WHO. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Accessed February 26, 2023. https://www.who.int/publications/i/item/9789240068759.
- Ruys TPE, Roos-Hesselink JW, Pijuan-Domènech A, et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart. 2015;101(7):530–536.
- Robertson JE, Silversides CK, Ling Mah M, et al. A contemporary approach to the obstetric management of women with heart disease. J Obstet Gynaecol Can. 2012;34(9):812–819.
- Easter SR, Rouse CE, Duarte V, et al. Planned vaginal delivery and cardiovascular morbidity in pregnant women with heart disease. Am J Obstet Gynecol. 2020;222(1):77.e1–77.e11.
- Warnes CA. Pregnancy and delivery in women with congenital heart disease. Circ J. 2015;79(7):1416–1421.
- Petrus AHJ, Jongert BL, Kiès P, et al. Evaluation of mode of birth in pregnant women with heart disease. Eur J Obstet Gynecol Reprod Biol. 2020;248:150–155.
- Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC guidelines on the management of cardiovascular diseases during pregnancy. Eur Heart J. 2011;32(24):3147–3197.
- Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the Management of Cardiovascular Diseases during Pregnancy.; Brussels, Belgium: European Society of Cardiology; 2018.
- Registry Of Pregnancy And Cardiac disease (ROPAC). Accessed October 29, 2020. https://www.escardio.org/Research/Registries-&-surveys/Observational-research-programme/Registry-Of-Pregnancy-And-Cardiac-disease-ROPAC.
- OECD iLibrary | Health at a Glance 2019: OECD Indicators. Accessed May 3, 2021. https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2019_4dd50c09-en.
- Stangl V, Schad J, Gossing G, et al. Maternal heart disease and pregnancy outcome: a single-centre experience. Eur J Heart Fail. 2008;10(9):855–860.
- Siu SC, Colman JM, Sorensen S, et al. Adverse neonatal and cardiac outcomes are more common in pregnant women with cardiac disease. Circulation. 2002;105(18):2179–2184.
- Ruys TPE, Cornette J, Roos-Hesselink JW. Pregnancy and delivery in cardiac disease. J Cardiol. 2013;61(2):107–112.
- Caughey AB, Cahill AG, Guise JM, et al. Safe prevention of the primary cesarean delivery this document was developed jointly by the with the assistance of. Am J Obstet Gynecol. 2014;210(3):179–193.
- Pfaller B, Sathananthan G, Grewal J, et al. Preventing complications in pregnant women with cardiac disease. J Am Coll Cardiol. 2020;75(12):1443–1452.
- Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104(5):515–521.
- Drenthen W, Boersma E, Balci A, et al. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010;31(17):2124–2132.
- Khairy P, Ouyang DW, Fernandes SM, et al. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006;113(4):517–524.
- Hayward RM, Foster E, Tseng ZH. Maternal and fetal outcomes of admission for delivery in women with congenital heart disease. JAMA Cardiol. 2017;2(6):664–671.
- Ouyang DW, Khairy P, Fernandes SM, et al. Obstetric outcomes in pregnant women with congenital heart disease. Int J Cardiol. 2010;144(2):195–199.
- Hidano G, Uezono S, Terui K. A retrospective survey of adverse maternal and neonatal outcomes for parturients with congenital heart disease. Int J Obstet Anesth. 2011;20(3):229–235.
- Hrycyk J, Kaemmerer H, Nagdyman N, et al. Mode of delivery and pregnancy outcome in women with congenital heart disease. PLOS One. 2016;11(12):e0167820–12.
- Tutarel O. Mode of delivery for pregnant women with heart disease. Heart. 2015;101(7):504–505.
- Easter SR, Valente AM, Economy KE. Creating a multidisciplinary pregnancy heart team. Curr Treat Options Cardio Med. 2020;22(1):1–14.
- Goya M, Casellas M, Merced C, et al. Predictors of obstetric complications in women with heart disease. J Matern Neonatal Med. 2016;29(14):2306–2311.
- Silversides CK, Grewal J, Mason J, et al. Pregnancy outcomes in women With heart disease: the CARPREG II study. J Am Coll Cardiol. 2018;71(21):2419–2430.
- Canobbio MM, Warnes CA, Aboulhosn J, et al. Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the american heart association.Circulation.2017;135(8): e50–e87.
- D'Souza R, Sermer M, Silversides C. The management of the cardiac patient in labour: primum non nocere. BJOG. 2017;124(9):1310.
- Parikh LI, Reddy UM, Männistö T, et al. Neonatal outcomes in early term birth. Am J Obstet Gynecol. 2014;211(3):265.e1–265.e11.
- Delnord M, Zeitlin J. Epidemiology of late preterm and early term births – An international perspective. Semin Fetal Neonatal Med. 2019;24(1):3–10.
- Chan E, Leong P, Malouf R, et al. Long-term cognitive and school outcomes of late-preterm and early-term births: a systematic review. Child Care Health Dev. 2016;42(3):297–312.
- Crump C, Sundquist K, Winkleby MA, et al. Early-term birth (37–38 weeks) and mortality in young adulthood. Epidemiology. 2013;24(2):270–276.
- Kotecha SJ, Gallacher DJ, Kotecha S. The respiratory consequences of early-term birth and delivery by caesarean sections. Paediatr Respir Rev. 201;19:49–55.