Abstract
Objective
Parity is a prognostic variable when considering trial of labor after cesarean section (TOLAC). This study aimed to determine whether grandmultiparous patients are at increased risk of poor TOLAC outcomes such as uterine rupture.
Study design
A retrospective cohort was conducted at a single university-affiliated medical center with approximately 10,000 deliveries per year. The study group included women post one cesarean section who attempted TOLAC carrying a singleton fetus in vertex presentation. We divided the cohort into three groups: group 1 – women who had a parity of 1; group 2 – parity of 2–4; group 3 – parity of 5 and above. The primary outcome was successful VBAC. Secondary outcomes included mode of delivery, uterine rupture, and combined maternal and neonatal adverse outcomes. Data were analyzed using Fisher’s exact test, Chi-square test, ANOVA, and paired t-test.
Results
Five thousand four hundred and forty-seven women comprised the study group: group 1 – 879 patients, group 2 – 2374 patients, and group 3 − 2194 patients. No significant between-group differences were found in gestational age at delivery. Rates of a successful VBAC were 80.6%, 95.4%, and 95.5%, respectively. Group 1 were more likely to have a failed TOLAC compared to group 2 (OR 5.02, 95% CI 3.9–6.5, p<.001) and group 3 (OR 5.17, 95% CI 4.0–6.7, p<.001). There was no increased risk of failed TOLAC when comparing groups 2 and 3 (OR 1.03; 95% CI 0.8–1.4, p=.89). Operative delivery rate differed significantly between all three groups; 25.1%, 6.2%, and 3.6%, for groups 1, 2, and 3, respectively (p<.001). The rate of uterine rupture was significantly higher in group 1 compared to group 2 (1.02% vs. 0.29% p=.02) and group 3 (1.02% vs. 0.2%, p=.01, respectively). There were no differences between group 2 and group 3 (0.29% vs. 0.2% p=.78).
Conclusions
Grandmultiparity is not associated with an increased risk of uterine rupture during TOLAC.
Introduction
A trial of labor after cesarean section (TOLAC) has been widely encouraged to combat the rising rate of cesarean deliveries worldwide and reduce the maternal and neonatal impacts of multiple repeat cesarean deliveries. However, while a successful VBAC is associated with good maternal and neonatal outcomes, a failed TOLAC can cause severe maternal and neonatal morbidity, such as blood transfusion and infectious complications, particularly in cases of uterine rupture [Citation1].
As a result, ideal candidates for TOLAC are women thought to have a high chance of succeeding and a low risk of complications. Women with a previous vaginal delivery [Citation2], previous vaginal birth after cesarean (VBAC) [Citation2], and spontaneous onset of labor [Citation3] have the best TOLAC outcomes, while women with advanced maternal age [Citation2], fetal macrosomia [Citation4], or no previous vaginal deliveries [Citation2] have less favorable results.
In the paper "the dangerous multipara", Solomons highlighted the risks associated with grandmultiparity [Citation5]. Indeed, studies have demonstrated that these patients are at increased risk of maternal and neonatal complications, including hypertensive disorders of pregnancy [Citation6], diabetes [Citation7], placental abruption [Citation6], postpartum hemorrhage [Citation6], and increased perinatal mortality [Citation8]. Of particular concern regarding TOLAC is the risk of uterine rupture, which has been reported in grand multiparas with spontaneous [Citation9] and induced labors [Citation10] and with [Citation11] and without [Citation9] a scarred uterus. However, these studies were small cohort studies conducted in low-resource settings. Results from larger studies conducted in high-resource settings, have not shown grandmultiparas to be at increased risk of uterine rupture when undergoing TOLAC [Citation12].
The purpose of this study was to ascertain whether grand multiparous patients who are keen to undergo a trial of labor after cesarean delivery have an increased risk of adverse maternal or neonatal outcomes. These data can help counsel grand multiparous women regarding the safety and feasibility of a TOLAC attempt and potentially avoid the complications of multiple repeat cesarean deliveries.
Methods
A retrospective cohort study was conducted at a single university-affiliated medical center over seven years. The delivery ward has around 10,000 deliveries per year and a cesarean delivery rate of 10%. The patient population is characterized by a large proportion of grandmultiparas who are highly motivated for vaginal delivery and TOLAC. Contraindications to TOLAC include a prior uterine incision other than a lower segment transverse incision and a clinical or sonographic estimated fetal weight of >4000 g. Before a TOLAC attempt, patients are counseled regarding their chances of success, risk of uterine rupture, and other maternal and neonatal adverse outcomes.
The study group consisted of women who underwent a trial of labor after one previous cesarean delivery with a single neonate. The rate of induction of labor in this cohort was 18%. Induction of labor in patients undergoing TOLAC at our center is carried out using one or more of the following methods, dependent on the patient’s preference and Bishop score, the insertion of an extra-amniotic balloon, a membrane sweep, artificial rupture of membranes and IV Oxytocin. The study group was divided into three groups according to parity. Group 1 – parity of 1 (no previous vaginal deliveries), group 2 – parity of 2–4, and group 3 – parity of 5 or greater.
The primary outcome was TOLAC success. Secondary outcomes included the mode of vaginal delivery, uterine rupture – defined as the disruption of all uterine layers before or during labor, postpartum hemorrhage – defined as >500 ml and >1000 ml blood loss after vaginal and cesarean delivery, respectively, neonatal APGAR score <7 at 5 min, umbilical artery pH <7.1 that were analyzed as individual parameters and as combined adverse maternal and neonatal outcome.
Data were collected from the computerized patient database. Demographic data and maternal and neonatal outcomes for each group were compared.
A statistical power analysis was performed. With an alpha=.05 and power = 0.80, the projected sample size needed to detect a 6% difference in TOLAC success rate is approximately 1668 in the control group and 268 in the study group. Thus with our proposed sample size of 879 in the control group and 2379 in the study group, our study is powered to detect significant differences in the primary outcome of TOLAC success.
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 25.0, IBM Corp. (Armonk, NY). Data were analyzed using Fisher’s exact test, Chi‐square tests, ANOVA, and Student’s t-test.
The local ethical review board approved the study.
Results
During the study period, there were 81,000 deliveries at our center. Five thousand four hundred and forty-seven women comprised the study group of women who underwent a trial of labor after one previous cesarean delivery. Group 1 consisted of 879 women, group 2 had 2734 women, and group 3 had 2194 women. The clinical and demographic characteristics of the study group are presented in . As expected, maternal age and the number of previous VBACs were significantly different. No significant between-group differences were found in the mean gestational age at delivery ().
Table 1. Demographic characteristics across the groups.
Rates of a successful VBAC were 80.6%, 95.4%, and 95.5% for groups 1, 2, and 3, respectively. Group 1 was more likely to have a failed TOLAC compared to group 2 (OR 5.02, 95% CI 3.9–6.5, p<.001) and group 3 (OR 5.17, 95% CI 4.0–6.7, p<.001); however, there was no difference in the rates of failed TOLAC between groups 2 and 3 (OR 1.03; 95% CI 0.8–1.4, p=.89). The rates of uterine rupture were 1.0%, 0.29%, and 0.23% in groups 1, 2, and 3, respectively. Patients in group 1 were more likely to experience uterine rupture compared to group 2 (OR 3.45, 95% CI 1.3, 9.3, p<.02) and group 3 (OR 4.3, 95% CI 1.5–14.5, p=.007); however, there was no difference in the rates of uterine rupture between group 2 and group 3 (OR 1.3, 95% CI 0.4, 4.0, p=.78).
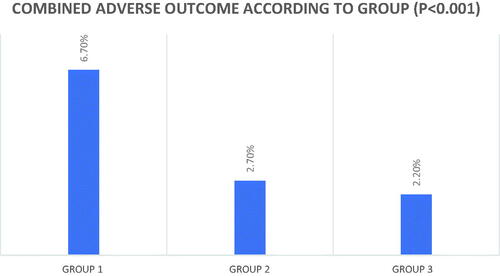
The rates of operative vaginal delivery, PPH, umbilical artery pH <7.1 and combined adverse outcomes were significantly greater in group 1 compared to groups 2 and 3, respectively, but there were no differences in the rates of these complications in group 2 compared to group 3 ( and ). There were no between-group differences in Apgar scores of <7 at 5 min.
Table 2. Maternal and neonatal outcomes among the groups.
Discussion
The results of our study demonstrate that grandmultiparous patients (parity of 5+) undergoing a trial of labor after one previous cesarean delivery have similarly high chances of achieving VBAC and are not at increased risk of adverse maternal and neonatal outcomes compared to multiparous patients (parity 2–4).
We also show that, compared to both multiparous and grandmultiparous women, patients with no previous vaginal deliveries undergoing TOLAC are at the highest risk of adverse TOLAC outcomes, including failed TOLAC, operative vaginal delivery, PPH, uterine rupture, and low umbilical artery pH.
A particular concern when considering a TOLAC is the risk of uterine rupture. When considering whether grandmultiparity affects this risk, on the one hand, a history of previous vaginal deliveries has been shown to protect against uterine rupture [Citation13]. On the other hand, the possible synergistic effect of age, grandmultiparity and a scarred uterus may worsen these patients’ prognosis [Citation2,Citation9–11]. The incidence of uterine rupture in our study was 1%, 0.29%, and 0.23% in groups 1, 2, and 3, respectively. The rate of uterine rupture in the group of patients with no history of previous vaginal delivery is similar to that reported in the literature [Citation13]. We also report that this group had the highest rate of uterine rupture compared to groups 2 and 3, which is consistent with studies demonstrating the protective effect of a previous vaginal delivery on uterine rupture [Citation9,Citation12–14].
Our results support the multiple studies in the literature demonstrating that the strongest predictor of a successful VBAC is a history of previous vaginal delivery [Citation2]. One study reported that patients with a history of previous vaginal delivery have TOLAC success rates of 87% vs. 61% in patients with no history of vaginal delivery [Citation14]. We report higher TOLAC success rates in patients with and without a previous vaginal delivery (95% and 80.5%, respectively) compared to those reported in the literature (60–80%) [Citation15]. This discrepancy can be attributed to the characteristics of our study group. Stemming from a cultural desire for large families, our patient population is highly motivated for TOLAC. We hypothesize that our patients’ strong desire for achieving TOLAC success was translated into an increased threshold for terminating the trial of labor which may have facilitated more patients achieving VBAC.
This study aimed to investigate the effect of grandmultiparity on TOLAC outcomes. The results of this study support the previously well-described protective effect of parity on TOLAC outcomes, and our study demonstrates that grandmultiparity is no different from multiparity and is not a risk factor in grand multiparous women desiring TOLAC.
The data regarding TOLAC outcomes in the grandmultiparous population are limited. However, the most extensive study to date in 1922 grandmultiparous attempting TOLAC at three medical centers in Jerusalem reports a uterine rupture risk of 0.3% and a TOLAC success rate of 87% [Citation16]. This result is similar to the present and other studies [Citation17–19] that have been conducted in high resource settings and indicate that TOLAC in grandmultiparous patients is safe with a high chance of success.
While older studies report increased risks of uterine rupture in grandmultiparous patients without a scarred uterus [Citation9,Citation10], it is possible that this has not been demonstrated in grandmultiparous patients in the setting of TOLAC owing to stricter selection criteria, a higher threshold for labor induction and augmentation as well as increased intrapartum surveillance due to concern about the risk for uterine rupture.
The increased incidence of operative delivery among group 1 was expected since it has been widely reported that nulliparous patients have a higher risk of undergoing operative vaginal delivery than multiparous patients [Citation20]. We also report overall high rates of operative vaginal delivery across all the study groups. The current rate of operative vaginal delivery in the United Kingdom is 10–15% [Citation21], and in our cohort, it was 25% in primiparous patients, 6.2% in multiparous patients and 3.5% in grandmultiparous patients. It is possible that our patient’s strong desire for vaginal delivery rather than a repeat cesarean delivery resulted in a higher rate of operative vaginal deliveries being performed and fewer second stage cesarean deliveries. This reciprocal relationship between cesarean and operative vaginal delivery rates is well known; since there is a parallel recent global trend in increasing rates of cesarean deliveries [Citation22], there has also been a dramatic decline in operative vaginal delivery rates [Citation21]. In our study, the converse is true, cesarean section rates were lower than average while there was a high overall rate of operative vaginal delivery.
The prevalence of PPH reported in the literature is around 1% [Citation22], a rate similar to that reported in our study. The risk of PPH in our study was highest in group 1, with no difference in risk between groups 2 and 3. Multiparity as well as grandmultiparity is thought to be a risk factor for postpartum hemorrhage [Citation6]. The lower rates of PPH in groups 2 and 3 may be due to more active management of the third stage of labor in multiparous patients at our center, including removal of the placenta, uterotonics, breastfeeding in the delivery room.
The implications from our study are that the group of patients at highest risk for adverse outcomes are patients undergoing TOLAC with no history of vaginal delivery. As a result, these may be the patients who should be considered high risk when considering their delivery management. Perhaps stricter selection criteria for TOLAC should be applied to this subgroup of patients and possibly more restricted induction of labor protocols and increased surveillance during labor. More research is required to determine which other modifiable factors increase the risk of adverse outcomes in this specific patient population. In addition, this study’s results can reassure patients and their clinicians when considering the outcomes of TOLAC attempts in a parous population, including the grandmultiparous population.
We report good outcomes from a grand multiparous population in high resource settings. Further research is required to ascertain whether grandmultiparity still has a protective effect in women undergoing a TOLAC attempt in a low-resource settings, where grandmultiparity is more common.
The strengths of this study are the large study population. We report results from one of the largest cohorts in the literature of over 2000 grand multiparous patients undergoing TOLAC. We also report results from a single center over a relatively short period, and therefore, the guidelines for TOLAC labor-management were uniform throughout the study.
The limitations of this study are its retrospective nature and the lack of data regarding the effect of other confounding variables.
Conclusions
A trial of labor after cesarean delivery on grand multiparous patients is safe and feasible for both mother and neonate. These data can be used to counsel grandmultiparas considering the mode of delivery to assist patients wanting to avoid multiple repeat cesarean deliveries.
Author contributions
Lopian M – project development, data collection, and first draft manuscript writing. Kashani-Ligumski L – project development, Data collection, and review of the final version of the manuscript; Cohen R – data collection and review of the final version of the manuscript; Herzlich J – data collection and review of the final version of the manuscript; Vinnikov Y – data collection and review of the final version of the manuscript; Perlman S – project development, supervision, and first draft manuscript writing.
Acknowledgements
Presentation: Presented at the SMFM 40th Annual Pregnancy Meeting, Texas.
Disclosure statement
There are no conflicts of interest or competing interests.
Additional information
Funding
References
- Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351(25):2581–2589.
- Grobman WA, Lai Y, Landon MB, et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstet Gynecol. 2007;109(4):806–812.
- Shanks AL, Cahill AG. Delivery after prior cesarean: success rate and factors. Clin Perinatol. 2011;38(2):233–245.
- Jastrow N, Roberge S, Gauthier RJ, et al. Effect of birth weight on adverse obstetric outcomes in vaginal birth after cesarean delivery. Obstet Gynecol. 2010;115(2 Pt 1):338–343.
- Solomons B. The dangerous multipara. Lancet. 1934;2:8.
- Babinszki A, Kerenyi T, Torok O, et al. Perinatal outcome in grand and great-grand multiparity: effects of parity on obstetric risk factors. Am J Obstet Gynecol. 1999;181(3):669–674.
- Samueloff A, Mor-Yosef S, Seidman DS, et al. Grand multiparity – a nationwide survey. Isr J Med Sci. 1989;25(11):625–629.
- Roman H, Robillard PY, Verspyck E, et al. Obstetric and neonatal outcomes in grand multiparity. Obstet Gynecol. 2004;103(6):1294–1299.
- Agrawal S, Agarwal A, Das V. Impact of grandmultiparity on obstetric outcome in low resource setting. J Obstet Gynaecol Res. 2011;37(8):1015–1019.
- Rahman J, Al-Sibai MH, Rahman MS. Rupture of the uterus in labor. A review of 96 cases. Acta Obstet Gynecol Scand. 1985;64(4):311–315.
- Ali AM, Abu-Heija AT. Obstetric and perinatal outcome of women para > or = 5 including one lower segment cesarean section. J Obstet Gynaecol Res. 2002;28(3):163–165.
- Hochler H, Wainstock T, Lipschuetz M, et al. Grandmultiparity, maternal age, and the risk for uterine rupture – a multicenter cohort study. Acta Obstet Gynecol Scand. 2020;99(2):267–273.
- Zelop CM, Shipp TD, Repke JT, et al. Uterine rupture during induced or augmented labor in gravid women with one prior cesarean delivery. Am J Obstet Gynecol. 1999;181(4):882–886.
- Landon MB, Leindecker S, Spong CY, et al. The MFMU cesarean registry: factors affecting the success of trial of labor after previous cesarean delivery. Am J Obstet Gynecol. 2005;193(3 Pt 2):1016–1023.
- Macones GA, Peipert J, Nelson DB, et al. Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol. 2005;193(5):1656–1662.
- Hochler H, Yaffe H, Schwed P, et al. Safety of trial of labor after cesarean delivery in grandmultiparous women. Obstet Gynecol. 2014;123(2 Pt 1):304–308.
- Kugler E, Shoham-Vardi I, Burstien E, et al. The safety of a trial of labor after cesarean section in a grandmultiparous population. Arch Gynecol Obstet. 2008;277(4):339–344.
- Schuit E, Kwee A, Westerhuis ME, et al. A clinical prediction model to assess the risk of operative delivery. BJOG. 2012;119(8):915–923. Erratum in: BJOG. 2017;124(8):1290.
- Murphy DJ, Strachan BK, Bahl R, et al. Assisted vaginal birth: green-top guideline no. 26. BJOG. 2020;127(9):e70–e112.
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2019. Natl Vital Stat Rep. 2021;70(2):1–51.
- Merriam AA, Ananth CV, Wright JD, et al. Trends in operative vaginal delivery, 2005–2013: a population-based study. BJOG. 2017;124(9):1365–1372.
- Sheldon WR, Blum J, Vogel JP, et al. Postpartum haemorrhage management, risks, and maternal outcomes: findings from the World Health Organization multicountry survey on maternal and newborn health. BJOG. 2014;121(Suppl. 1):5–13.