Abstract
Objectives
To assess factors associated with spontaneous rotation in the occiput anterior position for fetuses in persistent occiput posterior (OP) during the second stage of labor. To evaluate maternal and fetal outcomes after spontaneous rotation of persistent OP.
Methods
This is a prospective cohort of 495 women with fetuses in persistent OP position, confirmed with ultrasonography during the second stage of labor. We performed simple logistic regressions, followed by multiple logistic regressions.
Results
Among 495 women with fetuses in persistent OP position, 78 fetuses (16%) underwent a spontaneous rotation during the second stage of labor. The multivariate analysis found that a short duration of the first stage of labor (<7 h) was associated with a spontaneous rotation of the fetal head in the second stage of labor (OR 0.43 [0.23; 0.76. There were fewer episiotomies (25.6% vs 52.3%, p < .01), cesarean sections (0% v. 5.4%, p = .03), and instrumental deliveries (8.9% vs. 50%, p < .01) in the "spontaneous rotation” group, and the two groups were similar regarding post-partum hemorrhage.
The newborns in the “spontaneous rotation” group had a higher Apgar score at 1 min (10 v. 9, p = .02). The two groups did not differ for other neonatal parameters, such as arterial pH value, Apgar score at 5 min, birth trauma, or transfer into the pediatric unit.
Conclusion
A shorter duration of the first stage of labor (< 7 h) is a predictive factor of spontaneous rotation in the occiput anterior position for fetuses in persistent OP position. A spontaneous rotation in case of an OP position is associated with better maternal and fetal outcomes.
Introduction
The occiput posterior (OP) position is common in early labor (around 20% of fetuses), but the majority of fetuses initially in OP position rotate spontaneously during labor, and some of these spontaneous rotations occur during the second stage of labor [Citation1–5].
The OP position is known as persistent when this presentation persists in the second stage of labor. These persistent OP positions are associated with more prolonged labor, more frequent use of uterotonics, higher risks of operative deliveries, more frequent and severe vaginal and perineal tears, increased risk of postpartum hemorrhage and postpartum infections [Citation3,Citation4,Citation6–15]. These newborns have lower Apgar scores at birth, are more often admitted to the neonatal care unit and stay longer in the hospital [Citation3,Citation4,Citation7,Citation9,Citation15,Citation16]
Despite the frequency of these situations, there is currently no recommendation for the management of persistent OP positions. During the second stage of labor, different options are available to correct persistent OP position: expectative management with a potential spontaneous rotation, manual rotation or instrumental rotation [Citation2,Citation17–23]. Use of ultrasonography is helpful in the case of manual or instrumental rotation [Citation17,Citation18,Citation24,Citation25].
Currently, some centers suggest the possibility of a “prophylactic” manual rotation at full dilation in order to reduce perinatal risks [Citation26–30]. However, this manual rotation is not without risks, and some of these fetuses could have performed a spontaneous rotation. There are few data on factors associated with spontaneous rotation of the fetal head.
The purpose of this study is therefore to assess predictive factors of spontaneous rotation in the occiput anterior position of persistent OP positions during the second stage of labor, and to describe the maternal and fetal outcomes after these deliveries.
Methods
This is a prospective cohort study, conducted at Toulouse University Hospital, in the tertiary maternity ward, from September 2015 to October 2016 [Citation21].
We included all women with a singleton pregnancy, with the fetus in persistent OP position at full dilation. The type of presentation was systematically checked by ultrasound at the beginning of the second stage of labor.
Exclusion criteria were: stillbirth; medical terminations of pregnancy; non-cephalic presentations. Cesarean deliveries due to non-reassuring fetal condition in the first hour of the second stage were excluded as the rapid execution of the cesarean could not allow the fetus to spontaneously rotate. The indication of a cesarean section for non-progression, with a fetus in OP position, was not an exclusion criterion.
In our maternity ward, any clinical suspicion of a persistent OP position is confirmed by ultrasound. If this type of presentation is confirmed, a one-hour delay is allowed at full dilation. If the fetal head has progressed, a manual rotation is not performed. If after one or two hours the spontaneous rotation has not occurred, in the absence of progression of the fetal head, a correction of uterine contractility with oxytocin if necessary is performed, or a manual rotation if the uterine contractility is sufficient. An attempt at manual rotation is systematically performed in case of instrumental delivery. The variety of presentation is then attested by ultrasound.
We compared the patients whose fetuses underwent a spontaneous rotation in the occiput anterior position in the second stage of labor with the rest of the fetuses in the persistent OP position.
The two groups were compared on the following factors: weight, height, BMI (body mass index), gestational age, parity, scarred uterus, gestational diabetes, epidural analgesia modality, fetal sex, fetal biometrics, duration of the first stage of labor, delay between full dilation and the beginning of expulsive efforts, duration of the second stage of labor.
For maternal and fetal outcomes, the groups were compared on the following factors: perineal tear, episiotomy, mode of delivery (spontaneous vaginal delivery, instrumental delivery, cesarean section), post-partum hemorrhage; Apgar scores at 5 min, arterial pH at birth, shoulder dystocia, head trauma, transfer to the neonatal care unit.
Quantitative variables were described in terms of means (± standard deviation). Normality was validated graphically and using a Shapiro-Wilk test. Categorical variables were described in terms of numbers and proportions. Data were analyzed for quantitative variables with Student”s or Mann-Whitney”s tests according to the normality and homogeneity of variances between the two compared groups. For qualitative variables, the Chi2 test (or Fisher”s test in the event of theoretical numbers of less than 5) was used. A significance level of 5% was chosen.
Multivariate analysis was performed to identify factors associated with spontaneous rotation within the first hour of the second stage of labor.
First, simple logistic regressions were implemented for each predictive explanatory variable. This allowed us to check the log-linearity of continuous variables and transform them into quartiles if this condition was not met. Finally, a multiple logistic regression was implemented with all the predictive variables, with a descending stepwise selection to obtain the final model. Statistical analyses were performed using R version 4 and the R Studio software.
This study was approved by the Comité d”Ethique de la Recherche en Gynécologie Obstétrique under the IRB number (CEROG OBS 2013-11-02) and informed consent was obtained.
Results
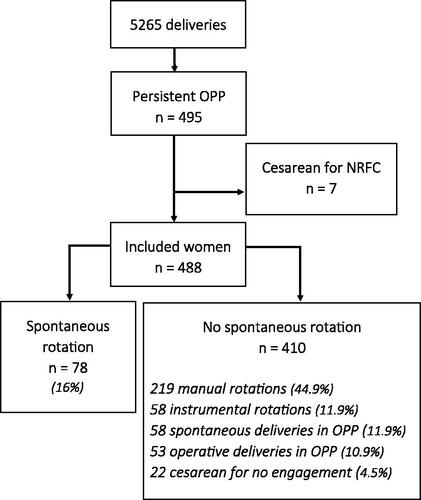
Between September 2015 and October 2016, among 5265 births, 495 women (9.4%) presented with a fetus in persistent OP position confirmed by ultrasound (). Seven patients were excluded because of an emergency cesarean section for a non-reassuring fetal condition during the first hour of the second stage. The characteristics of these patients were not different from the rest of the included population.
We observed 78 spontaneous rotations before delivery (16% of included patients) and 410 patients (84%) whose fetuses did not perform spontaneous rotations before delivery (delivery in OP position, manual or instrumental rotation, a cesarean section in posterior variety, or instrumental delivery in OP position). 76% (59/78) of the spontaneous rotations occurred during the first hour of the second stage of labor.
Among the variables studied, there was a significant difference between the two groups for maternal height and parity. The height difference between the two groups was not clinically relevant (about 2 centimeters). The maternal characteristics are shown in .
Table 1. Demographic and obstetrical outcomes.
The duration of each stage of labor (first and second stage) were significantly shorter in the “spontaneous rotation” group. These durations are shown in . Regarding maternal outcomes, there were fewer episiotomies (25.6% vs. 52.3%, p < .01) and fewer instrumental deliveries in the “spontaneous rotation” group (8.9% vs. 50.0%, p < .01).
Table 2. Duration of the different stages of labor (means, in hours and in minutes).
In the “non-spontaneous rotation” group, 194 patients (50%) had an instrumental delivery, for the arrest of progression, or non-reassuring fetal status, in comparison with 8.9% (7 out of 78 patients) in the “spontaneous rotation” group (p < .01). In the “non-spontaneous rotation” group, the proportion of cesarean sections for non-engagement was 5.4%, compared to 0% in the “spontaneous rotation” group (p = .03). Thus there were significantly fewer operative deliveries in the spontaneous rotation group compared to the “non-spontaneous rotation” group (8.9% vs 52.7%, p < .001). We did not find any difference between the two groups for post-partum hemorrhage or neonatal outcomes (Apgar score at 5 min, arterial pH, shoulder dystocia, head trauma, neonatal transfers). In addition, birth weight, birth size, and head circumference were similar between the two groups.
Maternal and neonatal outcomes are shown in .
Table 3. Maternal and fetal outcomes.
In bivariate analyses, we observed a significant difference between the two groups for the following variables: parity, maternal height and duration of the first stage of labor. After multiple logistic regressions, the multivariate analysis found only one variable involved in the prediction of spontaneous rotation: the duration of the first stage.
A duration of the first stage of labor greater than 7 h reduces the probability of spontaneous rotation (OR 0.39 [0.19; 0.77]), compared to women who had labor during less than 3 h (reference group). For other groups (duration between 3 and 5 h; and duration between 5 and 7 h), there was no difference with the reference group. A survival analysis showing probability of spontaneous rotation depending on the duration of first stage of labor is available as supplementary material.
Then, patients were separated into two groups depending on the duration of the first stage of labor: shorter than 7 h; or longer than 7 h. We found a similar result: a first stage of labor longer than 7 h reduces the probability of spontaneous rotation (OR 0.43 [0.23; 0.76]), compared to women who had labor during less than 7 h. These results are detailed in and .
Figure 2. Probability of spontaneous rotation at full dilation, depending on the duration of the first stage of labor.
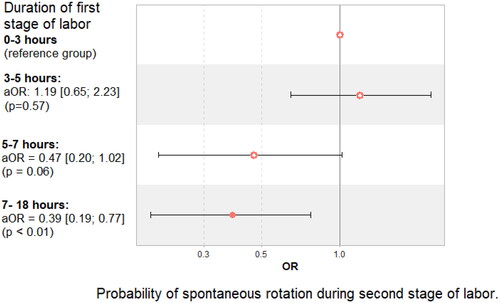
Table 4. Univariable analysis by simple logistic regressions for the probability of spontaneous rotation; then multivariable analysis by multiple logistic regression (step-by-step descending selection).
In addition, we compared the maternal and fetal outcomes between the women who had a spontaneous rotation and those in whom manual rotation was performed. There were more instrumental deliveries and episiotomies (p < .01) for the group “manual rotation”; there were no difference for the other outcomes.
This posthoc analysis is shown in .
Table 5. Posthoc analysis: comparison of maternal and neonatal outcomes, between “spontaneous rotation” and “manual rotation.”
Discussion
In our study, 16 % of fetuses in persistent OP position spontaneously rotated in occiput anterior position during the second stage of labor. Most of the spontaneous rotations occurred during the first hour of the second stage. This result is consistent with previous studies [Citation2–5].
The main significant data in the bivariate analysis found in this study are the duration of the first stage of labor, and parity, with a higher probability of observing spontaneous rotation for multiparous women. These characteristics are also found in other studies [Citation4,Citation5,Citation7,Citation10]. However, in the multivariate model, parity is no longer a significant variable. In the multivariate model from our study, the duration of the first stage of labor of more than 7 h reduces the probability of spontaneous rotation in the second stage of labor by almost 50%.
Regarding the duration of each stage of labor, women in the “spontaneous rotation” group had significantly shorter stages of labor. However, we cannot retain the durations of the second stage of labor (“time between full dilation and expulsive efforts,” “duration of active second stage,” and “total duration of the second stage of labor”) as being predictive factors of spontaneous rotation at one hour of full dilation. Indeed, the duration of these phases can be shortened by the fact that a fetus in the anterior position (after spontaneous rotation) is associated with faster labor [Citation1,Citation2,Citation5,Citation6].
Regarding demographic and obstetrical data, our study also shows that women whose fetuses spontaneously rotated were significantly taller. This variable is not significant in the final multivariate model.
Epidural analgesia may decrease the chances of spontaneous rotation. Some authors suggest that epidural analgesia decreases the mobility of the parturient and the possibilities of maternal postures, which would be associated with a lower probability of rotation, although this causal relationship is disputed [Citation5,Citation31]. However, these data are not statistically significant in our study.
Regarding maternal outcomes, our study shows a decreased rate of episiotomies and operative deliveries in the “spontaneous rotation” group. This reduction is classically explained by better cephalic flexion, which facilitates obstetrical mechanics [Citation1,Citation2], but this decrease is also found when we compared them with women who only had a manual rotation. Spontaneous rotation is less associated with instrumental deliveries even compared with manual rotation. This result may be partly due to the fact that in our service protocol, a manual rotation is offered in the setting of the absence of progression of the fetal head, and before operative deliveries in case of OP position.
For newborns in the “spontaneous rotation” group, their Apgar scores at 1 min are significantly higher; but this difference is clinically negligible as the 5 min Apgar scores are not different. The occurrence of other neonatal complications was not significantly different between the two groups. This lack of significance can, however, be explained by the low number of neonatal complications collected in our study.
The management of persistent OP position is currently debated.
The persistent OP position is the source of obstetrical complications, as the rates of cesarean section, instrumental deliveries and severe perineal tears are greatly increased [Citation6–8,Citation12]. Some interventions were used in order to have a rotation of the fetal head. Maternal postures are safe but their effectiveness has not been proven [Citation32]. Moreover, instrumental rotation can be a substantial help but is more invasive [Citation19–20].
Manual rotation seems to be an effective and safe way to get an occiput anterior position from a fetus initially in an OP position, and with fewer complications than instrumental rotation [Citation33]. Recent works tend to show the superiority of manual rotation over other managements of the persistent OP position, but there is no definitive optimal management for the persistent OP position yet [Citation26–30]. In particulary, interrogations remain about the optimal timing for performing a manual rotation, between “prophylactic” rotation in the beginning of the second stage of labor and “therapeutic” rotation (i.e. in case of non-progression of the fetal head or before operative delivery).
In our study, we showed that the chances of spontaneous rotation during the second stage of labor are non-negligible, especially during the first hour. The opportunity to provide a one-hour expectative delay for women whose fetuses are in persistent OP position with correction of uterine dynamics is an alternative option, allowing some of these fetuses to undergo spontaneous rotation.
The strengths of our study are its prospective design and a large number of women included, and the homogeneity of practices in the delivery room at the Toulouse University Hospital. The type of presentation was also systematically confirmed by ultrasound in the delivery room. The limitations to this study are the unicentric nature of the analysis, and the frequent performance of manual rotations in the absence of progression, mechanically lowering the rate of spontaneous rotation.
Conclusion
In our prospective study, 1 out of 6 fetuses in persistent OP position spontaneously rotated in the occiput anterior position during the second stage of labor. Most of the spontaneous rotations occurred during the first hour of the second stage. The only factor associated with spontaneous rotation at full dilation was the duration of the first stage of labor. A short duration of the first stage of labor (<7 h) was predictive of spontaneous rotation in the second stage of labor.
Maternal and fetal outcomes were better when spontaneous rotation occurred than in the other situations in our cohort. These data suggest that we should consider waiting for spontaneous rotation before manual rotation, especially for patients with a short first stage of labor. This study may help to refine the management of these frequent situations, and possibly avoid a rotation maneuver in patients with a higher probability of spontaneous rotation.
Supplemental Material
Download MS Word (66.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Schaal JP, Benoit S, Eyraud JL, et al. [Normal delivery with vertex presentation]. Rev Prat. 15 févr. 1997;47(4):435–449.
- Castel P, Bretelle F, D’Ercole C, et al. [Pathophysiology, diagnosis and management of occiput posterior presentation during labor]. Gynecol Obstet Fertil Senol. 2019;47(4):370–377.
- Simkin P. The fetal occiput posterior position: state of the science and a new perspective. Birth. 2010;37(1):61–71.
- Othenin-Girard V, Boulvain M, Guittier M-J. Accouchement en variété occipito-postérieure : issues materno-fœtales et facteurs prédictifs de la rotation. Gynecol Obstet Fertil Senol. 2018;46(2):93–98.
- Blanc-Petitjean P, Le Ray C, Lepleux F, et al. Factors affecting rotation of occiput posterior position during the first stage of labor. J Gynecol Obstet Hum Reprod. 2018;47(3)119–125.
- Barth WH. Persistent occiput posterior. Obstet Gynecol. 2015;125(3):695–709.
- Cheng YW, Shaffer BL, Caughey AB. Associated factors and outcomes of persistent occiput posterior position: a retrospective cohort study from 1976 to 2001. J Matern-Fetal Neonatal Med off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2006;19(9):563–568.
- Fitzpatrick M, McQuillan K, OHerlihy C. Influence of persistent occiput posterior position on delivery outcome. Obstet Gynecol. 2001;98(6):1027–1031.
- Riethmuller D, Teffaud O, Eyraud JL[, et al. Maternal and fetal prognosis of occipito-posterior presentation. J Gynecol Obstet Biol Reprod févr. 1999;28(1):41–47.
- Sizer AR, Nirmal DM. Occipitoposterior position: associated factors and obstetric outcome in nulliparas. Obstet Gynecol. 2000;96(5 Pt 1):749–752.
- Ducarme G, Pizzoferrato AC, de Tayrac R, et al. Perineal prevention and protection in obstetrics: CNGOF clinical practice guidelines. J Gynecol Obstet Hum Reprod. 2019;48(7):455–460.
- Ponkey SE, Cohen AP, Heffner LJ, et al. Persistent fetal occiput posterior position: obstetric outcomes. Obstet Gynecol. 2003;101(5, Part 1):915–920.
- Fitzgerald MP, Weber AM, Howden N, et al. Pelvic floor disorders network. Risk factors for anal sphincter tear during vaginal delivery. Obstet Gynecol. 2007;109(1):29–34.
- Pergialiotis V, Bellos I, Fanaki M, et al. Risk factors for severe perineal trauma during childbirth: an updated meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;247:94–100.
- Pearl ML, Roberts JM, Laros RK, et al. Vaginal delivery from the persistent occiput posterior position. Influence on maternal and neonatal morbidity. J Reprod Med. 1993;38(12):955–961.
- Cheng YW, Shaffer BL, Caughey AB. The association between persistent occiput posterior position and neonatal outcomes. Obstet Gynecol. avr. 2006;107(4):837–844.
- Vayssière C, Beucher G, Dupuis O, et al. Instrumental delivery: clinical practice guidelines from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2011;159(1):43–48.
- Masturzo B, Farina A, Attamante L, et al. Sonographic evaluation of the fetal spine position and success rate of manual rotation of the fetus in occiput posterior position: a randomized controlled trial. J Clin Ultrasound. 2017;45(8):472–476.
- Vidal F, Simon C, Cristini C, et al. Instrumental rotation for persistent fetal occiput posterior position: a way to decrease maternal and neonatal injury? PLOS One. 2013;8(10):e78124.
- Guerby P, Allouche M, Simon-Toulza C, et al. Management of persistent occiput posterior position: a substantial role of instrumental rotation in the setting of failed manual rotation. J Matern Fetal Neonatal Med. 2 Janv. 2018;31(1):80–86.
- Guerby P, Parant O, Chantalat E, et al. Operative vaginal delivery in case of persistent occiput posterior position after manual rotation failure: a 6-month follow-up on pelvic floor function. Arch Gynecol Obstet. 2018;298(1):111–120.
- Marguier Blanchard I, Metz J-P, Eckman Lacroix A, et al. [Manual rotation in occiput posterior position: a systematic review in 2019]. Gynecol Obstet Fertil Senol. 2019;47(9):672–679.
- Le Ray C, Goffinet F. [Manual rotation of occiput posterior presentation]. Gynecol Obstet Fertil. 2011;39(10):575–578.
- Gaudineau A, Vayssière C. Place de l’échographie en salle de naissance. Gynécologie Obstétrique Fertil. mars. 2008;36(3):261–271.
- Tao H, Wang R, Liu W, et al. The value of intrapartum ultrasound in the prediction of persistent occiput posterior position: systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. juill. 2019;238:25–32.
- Blanc J, Castel P, Mauviel F, et al. Prophylactic manual rotation of occiput posterior and transverse positions to decrease operative delivery: the PROPOP randomized clinical trial. Am J Obstet Gynecol. 2021;225(4):444.e1–444.e8.
- Verhaeghe C, Corroenne R, Spiers A, et al. Delivery mode after manual rotation of occiput posterior fetal positions: a randomized controlled trial. Obstet Gynecol. 2021;137(6):999–1006.
- Phipps H, Hyett JA, Kuah S, et al. Persistent occiput posterior position outcomes following manual rotation: a randomized controlled trial. Am J Obstet Gynecol MFM. 2021;3(2):100306.
- De Vries B, Phipps H, Kuah S, et al. Transverse position. Using rotation to aid normal birth-OUTcomes following manual rotation (the TURN-OUT trial): a randomized controlled trial. Am J Obstet Gynecol MFM. 2022;Sep 174(1):100488.
- Bertholdt C, Piffer A, Pol H, et al. Management of persistent occiput posterior position: the added value of manual rotation. Int J Gynaecol Obstet. 2022;157(3):613–617.
- Anim‐Somuah M, Smyth RM, Cyna AM, et al. Epidural versus non‐epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev [Internet]. 2018;5(5):CD000331.
- Hunter S, Hofmeyr GJ, Kulier R, Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). Cochrane Database Syst Rev [Internet]. 2007;2007(4):CD001063.
- Bertholdt C, Morel O, Zuily S, et al. Manual rotation of occiput posterior or transverse positions: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2022;226(6):781–793.