Abstract
Objective
To identify the clinical characteristics of pregnancy associated group A streptococcus (GAS) infection and predictors for intensive care unit (ICU) admission.
Methods
A retrospective cohort study of culture-proven pregnancy-related GAS infections in tertiary hospital Electronic medical records were reviewed, for cases of cultures positive GAS that were identified between January 2008 and July 2021. A GAS infection was defined by the isolation of the pathogen from a sterile liquid or tissue site. Blood and urine cultures were obtained from all patients with peripartum hyperpyrexia (fever >38 °C). Medical Personnel screening included cultures of the throat, rectum, and skin lesions (if present). In cases of hemodynamic instability patients were transferred ad hoc to ICU, according to the obstetrician and intensivist judgment.
Results
Of the 143,750 who delivered during the study period, 66 (0.04%) were diagnosed as having a pregnancy associated GAS infection. Of these, 57 patients presented postpartum, and represented the study cohort. The most common presenting signs and symptoms among puerperal GAS, were postpartum pyrexia (72%), abdominal pain (33%), and tachycardia (>100 bpm, 22%). 12 women (21.0%) developed streptococcal toxic shock syndrome (STSS. Predictors for STSS and ICU admission were: antibiotic administration >24 h from presentation postpartum, tachycardia, and a C-reactive protein level >200 mg/L. Women that received antibiotic prophylaxis during labor had a significantly lower rate of STSS (0 vs 10, 22.7%; p = .04).
Conclusion
Deferral of medical intervention >24 h from the first registered abnormal sign had the most important impact on deterioration of women with invasive puerperal GAS. Antibiotic prophylaxis during labor in women with GAS may reduce associated complications.
Introduction
Gram-positive beta-haemolytic group A Streptococcus (GAS) bacteria, cause infections responsible for a wide range of diseases in humans [Citation1–3]. GAS-associated endometritis is a potentially life-threatening event during pregnancy and postpartum [Citation2,Citation4,Citation5]. GAS infections have reemerged since the 1980s [Citation6] after a period of continuous decline in infection rates associated with infection control measures and penicillin use. GAS infections account for more than 75,000 yearly deaths worldwide [Citation2]. The attack rate of invasive GAS infection is 20-fold higher for pregnant and postpartum women compared to non-pregnant women [Citation6]. Approximately 85–93% of infections occur postpartum among patients with pregnancy-related GAS infection [Citation7,Citation8]. Risk factors for intrapartum and postpartum GAS infection include upper respiratory tract infection prior to delivery, contact with carriers of GAS infection during pregnancy [Citation9], and risk factors attributed to the delivery itself, such as preterm premature rupture of membranes (PPROM) [Citation1], mucosal damage, and emergency cesarean deliveries [Citation10].
A rate of maternal morbidity and even mortality was reportedly as high as 60% when streptococcal toxic shock syndrome (STSS) develops [Citation11]. The severity of maternal infection in cases of pregnancy-associated GAS infection can be difficult to predict, and there is a lack of studies on predictions of pregnancy-associated GAS disease severity. It is plausible to assume that late recognition of pregnancy-associated GAS is related to substantial morbidities, such as Streptococcal toxic shock syndrome (STSS), intensive care (ICU) admissions, septic shock, surgical intervention, and emergency hysterectomy.
This study aimed to determine the risk factors associated with GAS disease severity in the postpartum period, such as maternal STSS and rates of admission to the ICU. The objective was to assess the impact of a delay in recognition of the infection or pathogen subtype and the provision of appropriate treatment on maternal instability and clinical deterioration.
Material and methods
This was a retrospective cohort study performed in a single university-affiliated tertiary medical center with an annual birth rate of approximately 12,000 deliveries. Comprehensive electronic medical records were reviewed, and all cases of cultures positive for GAS that had been taken from various body sites and fluids between January 2008 and July 2021 were identified.
A GAS infection was defined by the isolation of the pathogen from a sterile liquid or tissue site. A postpartum GAS infection was defined as the isolation of GAS growth in association with a clinical infection during the postpartum period. Blood and urine cultures were obtained from all patients with peripartum hyperpyrexia (fever >38 °C). Additional cultures such as vaginal and cervical were obtained in some cases of a suspected maternal infection.
Each case of a positive culture was considered as being infectious since GAS is considered a specific pathogen and not a contaminant/coloniser.
The bacterial identification tests from the clinical specimens were performed at the local microbiology laboratory using the VitekMS and Vitek2 systems (bioMerieux, St. Louis, MO) according to the Clinical and Laboratory Standards Institute criteria. The characteristics of the GAS infections were retrieved from medical files, including time to symptom onset, initial symptoms or signs of illness, maximal body temperature, laboratory workup, and time from first presentation of symptoms to antibiotic treatment. The complications, including adult respiratory distress syndrome, renal and hepatic failure, disseminated intravascular coagulation, transfer to the ICU, and mechanical ventilation, were also documented. Lastly, the data on the medical and surgical treatments (antibiotics, intravenous immunoglobulin administration, laparoscopy, and hysterectomy) were collected and reviewed.
In accordance with the medical policy, an epidemiologic investigation was carried out after every case of postpartum GAS infection, and it included screening for group A streptococci carriage from all healthcare workers who treated the patients from the time of admission. Personnel screening included cultures of the throat, rectum, and skin lesions (if present). It should be noted that vaginal cultures were nor preformed. An institutional investigation was carried out by The Infection Control Unit in cases of GAS infection-related isolation, and the samples taken from the healthcare workers who had been screened during the investigation were sent to the national streptococci reference laboratory for subtyping analysis in cases of hospital-acquired infection.
The departmental antibiotic protocol included: antimicrobial prophylaxis (2 g cefazolin intravenously 30 min before skin incision) in cases of cesarean deliveries. If PPROM occurred prior to 34 weeks and there were no signs of chorioamnionitis or fetal distress, the pregnancies were managed expectantly until 35 weeks at which time they were routinely induced. Expectant management included a five-day antibiotic course in accordance with The Mercer protocol for PPROM. Penicillin-based antibiotics and intravenous clindamycin (900 tid) were administered after the diagnosis of a GAS-related illness had been established.
Descriptive statistics are expressed as median, mean, standard deviation, minimum and maximum values, and interquartile ranges (IQR). Student’s t-test was used for parametric variables that were normally distributed, and a Welch’s t-test or a Mann–Whitney U test was used for non-parametric variables that were non-normally distributed. Fisher’s exact test was applied for small samples of categorical variables. All tests were two-sided, and p-values of <.05 were considered significant. Bootstrap resampling with random computer-generated iterations was applied in cases of n = 0.
Results
During the study period, there were 143,750 deliveries, 66 (0.04%) were diagnosed as having a pregnancy associated GAS infection. Of these, 57 patients presented postpartum, and represented the study cohort.
57 women identified with puerperal GAS-, of these 42 (73.1%) delivered vaginally, 5 (8.7%) by vacuum extraction, and 10 (26.3%) by cesarean delivery. During the study period, there was an incidence of one puerperal GAS infection per 2521 deliveries (0.04%) in 12.5-year study period. () Fifteen GAS-infected women were treated with antibiotics by routine protocols during labor: specifically, nine women during a cesarean delivery, three because of a GBS-positive test result, and three others due to a fever during labor. None of the patients were treated with antibiotics due to PPROM.
Table 1. Characteristics of group A Streptococcus infection in pregnancy and postpartum (n = 57).
No deaths occurred among this cohort.
The most common presenting signs and symptoms of infection among puerperal GAS infection were postpartum fever (48 patients, 84.2%), abdominal pain (22, 38.5%), and/or tachycardia (15, 26.8%). Cultures positive for GAS infection were obtained from various body sites and sterile liquids, mostly from the female genital tract (uterus, cervix, vagina, lochia, and placenta, 66%), followed by blood (36%), urine (13%), cesarean delivery and episiotomy wounds (6%). There were 28 puerperal women (49.1%) with GAS-positive cultures originating from more than one sites.
Complications and treatment of puerperal associated GAS infections are presented in . Twelve women (21.0%) developed STSS, of whom 10 delivered vaginally and two by cesarean delivery. The infectious prodrome occurred soon after birth, and the STSS was diagnosed within 48 h of delivery in eight of the 12 women (66.6%), between 2 and 7 days in three, and more than 1 week postpartum in the remaining two. Positive genital tract cultures for GAS infection (from the uterus, cervix, vagina, lochia, or placenta) were obtained from 11 women (84.6%). Blood cultures were positive in six women. Organ complications included disseminated intravascular coagulation (n = 4), acute respiratory distress syndrome (n = 8), acute liver failure (n = 4), acute renal injury (n = 2), necrotizing fasciitis (n = 1) and respiratory failure necessitating intubation (n = 4).
Table 2. Complications and treatment for group A Streptococcus infections in women with streptococcal toxic shock syndrome admitted to an intensive care unit (n = 12).
The characteristics of the women with a puerperal GAS, transferred to the ICU compared to women hospitalized in the maternity department are presented in . The groups were similar with regard to age, body mass index, and mode of delivery. The rate of women who presented with tachycardia (>100 bpm) was higher among the ICU group (50% vs 17.7%, p = .02). The rate of women who showed abnormal signs/symptoms less than 48 h after delivery was higher among women admitted to the ICU (61% vs 28%, p = .02). The rate of women who were first started on antibiotic treatment more than 24 h from presentation (first clinical sign) was also higher among those in the ICU group (98% vs 38.4% p < .001) the calculated RR for ICU admission in cases of antibiotic deferral was 10.85, 95%,Cl for RR (9.408, 12.29). Six of the women who had been transferred to the ICU also received intravenous immunoglobulin. Exploratory laparoscopy or laparotomy was performed in six cases in which the patient had failed to recover following antibiotics and supportive treatment in the ICU.
Table 3. Characteristics of women admitted to an intensive care unit (n = 12).
The dominant emm strains that were isolated were: emm 14.3 (n = 3), emm 22 (n = 3), emm 75 (n = 4), and emm 11 (n = 3) and all of the affected patients were admitted to the ICU (). represents the multi-year analysis of infections in the medical center. Five infections were deemed to be acquired from the hospital staff, and three of them that occurred in March 2008 were identified as having the same source of infection. Therefore, the overall rate of a proven hospital personal associated GAS infection was 8.7%.
Figure 1. A multi-year description of pregnancy associated GAS infection and the results of the epidemiologic investigation. Eis: epidemiologic investigation status, Ca: community acquired, Ha: hospital-staff acquired, LpHa: low probability of hospital staff acquired.
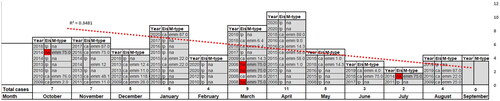
Table 4. Characteristics of women who received antibiotics during labor.
describes the characteristics of the women who either received or not antibiotics during labor and subsequently developed puerperal GAS infection. Those who received antibiotic prophylaxis during labor for various reasons (primarily due to a positive GBS screen or a cesarean delivery) had significantly lower rates of a subsequent STSS [0 vs 10 (22.7%), p = .04], although the time from delivery to septic presentation was significantly longer (8 ± 4.8 vs 4.8 ± 4.2), p = .008).
Most of the identified cases of infection occurred between October–April (n = 45, 78.7%) compared to the period between May and September (n = 12, 21.2%, p = .0001) ().
Discussion
This study sought to report the clinical consequences of women diagnosed with pregnancy-associated GAS. Its main findings were:
Women who received antibiotic prophylaxis during labor for various reasons had less severe infectious characteristics, such as STSS. This observation was supported by a longer interval between delivery to the first infectious presentation in those who received antibiotics.
ICU admission was predicted by a delayed empirical antibiotic administration of more than 24 hours after postpartum presentation and tachycardia.
In contrast to other reports on a 30% mortality rate, there were no incidences of maternal death among the women who had sustained SSTS in the current study.
Hospital staff transmission was relatively uncommon throughout the study period. There was a seasonal distribution of GAS infection in a multi-year analysis, with most cases having been identified between October and April.
In spite of the advances in medical care, pregnancy-associated GAS infection contributes significantly to maternal morbidity and mortality worldwide. Since the recognition of healthcare personnel-related puerperal sepsis by Semmelweis [Citation12], extensive and costly efforts have been undertaken to investigate outbreaks of GAS infection from a common nosocomial source. Contrarily, the current study findings, taken together with previous reports [Citation8,Citation13], reveal that healthcare personnel test negative in most cases, and that infections are considered as being community acquired for the most part. The overall incidence of puerperal GAS infection in the current cohort was like that of a previous study from the same institution [Citation13].
This study has several limitations that bear mention. First, its retrospective nature raises questions about the applicability and generalization of the results to account for local strains and subtypes. Second, several variables were underpowered, such as the rates of hysterectomies and laparotomies, since the prophylactic antibiotic analysis used only relatively small numbers. Furthermore, it was not possible to identify specific risk factors (e.g. throat colonization and carriers among family members), which might serve as predictors for a possible future screening system for GBS prophylaxis. Lastly, it is very challenging to study the associations between emm types and clinical manifestations due to the vast number of circulating emm types.
An additional limitation is that expected in cases of mild GAS associated symptoms, in these cases infection and specifically GAS could potentially overlooked, this could affect both the identification of the crude prevalence of GAS cases and identification of milder emm groups, however, to a much lesser extent we believe is prone to miss the iGAS cases.
Interpretation
The present study emphasizes the importance of vital signs and the early recognition of infection for preventing a rapid infectious sequala. The regression analysis of the characteristics and clinical course of the 12 women whose pregnancy had been complicated with STSS and who were admitted to the ICU revealed that tachycardia as the first presenting sign and delay in providing antibiotic treatment were independent risk factors for severe infection that led to STSS and hospitalization in the ICU. It is noteworthy that a high level of suspicion of STSS is always warranted because no single risk factor, specific clinical sign, or laboratory point to this serious complication. Since vital signs have been demonstrated as being of the utmost clinical importance with regard to infection prediction in cases of delay, the implementation of simple wearable technologies with the capacity for continuous monitoring of vitals should be considered.
Although GAS is a highly virulent pathogen, it has almost no resistance toward chemo-prophylactic agents commonly administered in labor. It was interesting to trace the natural history of patients diagnosed with GAS who received antimicrobial prophylaxis regardless of whether the source of infection was or was not known. The impact of antimicrobial prophylaxis has been described extensively by many authors as prolonging the disease-free state/latency period [Citation14]. The eventual reduction in disease morbidity would be logical in this case, but it has yet to be proven. A large number of these individuals in the current work had received antimicrobial prophylaxis prior to undergoing a cesarean delivery, which could be a potential confounder. However, as stated in the results, the rates of cesarean delivery-related GAS infection were similar to its relative proportion in vaginal deliveries over the entire study period at the authors’ institution. Assuming that antimicrobial prophylaxis at labor may indeed reduce the risk of severe infection, and specifically STSS, the calculated number needed to treat one case of STSS by antimicrobial prophylaxis is 14,375 women.
The seasonality of the incidence of GAS has been reported before [Citation15] in a large epidemiologic survey from 1975 to 2012. Those authors reported a significant seasonal variation in the incidence of GAS infections. They noticed a mid- to late-winter increase from January to April in both incidence and severity of infection (the diagnoses of sepsis, STSS, and death) among children and adults (38% vs 16%, respectively, p < .01). Puerperal sepsis was diagnosed in only eight of their study women, precluding the drawing of any specific inferences for that subgroup. The current study had similar results, with most of the identified cases of GAS infection having occurred between October and April, although there was no significant correlation between specific emm-type and infection severity or seasonality.
It is important to note that there was no patient mortality in this study. This finding may be attributable to the fact that it is a tertiary care hospital with a large and skilled staff, that intensive antibiotic treatment was identified and started promptly, and that all patients received antibiotics. Additionally, it’s possible that these strains are less aggressive than those in other cohorts
This study documented the incidence, clinical course, and outcomes of pregnancy-related GAS infection and sought to elucidate the factors associated with infection severity. Deferral of medical intervention of more than 24 h from the first signs of infection had the most important impact upon maternal deterioration. Antibiotic prophylaxis during labor may reduce GAS complications, warranting further study to detect specific risk factors and to reassess GAS screening, antibiotic prophylaxis and prevention policies.
Ethical approval
This study was approved by the institutional ethics review board, approval number 0284-08-TLV: July 2015.
Disclosure statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Funding
References
- Anteby EY, Yagel S, Hanoch J, et al. Puerperal and intrapartum group a streptococcal infection. Infect Dis Obstet Gynecol. 1999;7(6):276–282.
- O'Loughlin RE, Roberson A, Cieslak PR, et al. The epidemiology of invasive group a streptococcal infection and potential vaccine implications: United States, 2000–2004. Clin Infect Dis. 2007;45(7):853–862.
- Tanaka H, Katsuragi S, Hasegawa J, et al. The most common causative bacteria in maternal sepsis-related deaths in Japan were group a Streptococcus: a nationwide survey. J Infect Chemother. 2019;25(1):41–44.
- Schuitemaker N, van Roosmalen J, Dekker G, et al. Increased maternal mortality in The Netherlands from group a streptococcal infections. Eur J Obstet Gynecol Reprod Biol. 1998;76(1):61–64.
- Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–1074.
- Gustafson LW, Blaakær J, Helmig RB. Group a streptococci infection. A systematic clinical review exemplified by cases from an obstetric department. Eur J Obstet Gynecol Reprod Biol. 2017;215:33–40.
- Hamilton SM, Stevens DL, Bryant AE. Pregnancy-related group a streptococcal infections: temporal relationships between bacterial acquisition, infection onset, clinical findings, and outcome. Clin Infect Dis. 2013;57(6):870–876.
- Rottenstreich A, Benenson S, Levin G, et al. Risk factors, clinical course and outcomes of pregnancy-related group a streptococcal infections: retrospective 13-year cohort study. Clin Microbiol Infect. 2019;25(2):251.e1–e4.
- Leonard A, Wright A, Saavedra-Campos M, et al. Severe group a streptococcal infections in mothers and their newborns in London and the South East, 2010–2016: assessment of risk and audit of public health management. BJOG. 2019;126(1):44–53.
- Tuuli MG, Liu L, Longman RE, et al. Infectious morbidity is higher after second-stage compared with first-stage cesareans. Am J Obstet Gynecol. 2014;211(4):410.e1–6.
- Rimawi BH, Soper DE, Eschenbach DA. Group a streptococcal infections in obstetrics and gynecology. Clin Obstet Gynecol. 2012;55(4):864–874.
- Atalić B. Uz 200. obljetnicu rođenja Ignaza Philippa Semmelweisa [200th birth anniversary of Ignatius Philipp Semmelweis]. Acta Med Hist Adriat. 2018;16(1):9–18. Jun;16(1):9-18. Croatian. PMID: 30198270.
- Shinar S, Fouks Y, Amit S, et al. Clinical characteristics of and preventative strategies for peripartum group a streptococcal infections. Obstet Gynecol. 2016;127(2):227–232. PMID: 26942347.
- Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997;278(12):989–995.
- Olafsdottir LB, Erlendsdóttir H, Melo-Cristino J, et al. Invasive infections due to Streptococcus pyogenes: seasonal variation of severity and clinical characteristics, Iceland, 1975 to 2012. Euro Surveill. 2014;19(17):5–14. Erratum in: Euro Surveill. 2016;21(10). PMID: 24821122.

