Abstract
Purpose
Even though the risks and advantages of repeat Cesarean sections (CSs) and vaginal births after cesarean section (VBACs) are well studied, there is a scarcity of information on the effects of previous CS on maternal and fetal outcomes during subsequent deliveries. The aim of this study is to evaluate delivery mode and fetal outcomes in a trial of labor after cesarean section (TOLAC).
Methods
In this nationwide retrospective cohort study, data from the National Medical Birth Register (MBR) were used to evaluate the outcomes of TOLACs. TOLACs were compared to the outcomes of the trial of labor after previous successful vaginal delivery. A multivariable logistic regression model was used to assess the primary outcomes (delivery mode, neonatal intensive care unit, and perinatal/neonatal mortality). Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were used for comparison.
Results
A total of 29 352 (77.0%) women attempted vaginal delivery in the TOLAC group. In the control group, 169 377 (97.2%) women attempted vaginal delivery. The adjusted odds for urgent CS (aOR 13.05, CI 12.59–13.65) and emergency CS (aOR 3.65, CI 3.26–4.08) were notably higher in the TOLAC group when compared to the control group. The odds for neonatal intensive care unit treatment (aOR 2.05, CI 1.98–2.14), perinatal mortality (aOR 2.15, CI 1.79–2.57), and neonatal mortality (aOR 1.75, CI 1.20–2.49) were higher in the TOLAC group.
Conclusions
The odds for emergency CS were higher among women who underwent TOLAC. The odds for neonatal intensive care and perinatal mortality were also higher, and further research is needed to identify those expecting women who are better suited for TOLAC to minimize the risk for a neonate. The results of this study should be acknowledged by the mother and the clinician when considering the possibility of vaginal births after cesarean section.
Introduction
Vaginal births after cesarean section (VBACs) are a suggested alternative to repeated cesarean sections (CSs). The trend of increasing CS rates had evoked worldwide attention for both healthcare workers and the general population. Many studies have assessed the worldwide incidence of CS and it has been found to be increasing rapidly [Citation1,Citation2]. Despite the rapidly increasing incidence worldwide, the rates of CS have remained low (19% in 2020) in Finland [Citation3]. High-income European countries have an uneven distribution of CS rates, with Southern European countries, such as Italy and Cyprus having higher rates [Citation4,Citation5]. Although the World Health Organization (WHO) recommends a CS rate not higher than 15%, it has been recently suggested 19% would be more reasonable yet still effective in reducing maternal and neonatal morbidity and mortality [Citation6].
The main factor contributing to these discrepancies is the prevalence of repeat cesarean sections within and across countries, with Italy having the highest CS rate in Europe at almost 40% [Citation4,Citation5]. Multiple repeat CS are known to be risk factors for adverse events, such as uterine rupture and intraoperative complications [Citation7]. Multiple repeat cesarean deliveries are associated with more difficult surgery and increased blood loss compared with a second planned cesarean delivery, and the risk of major complications increases with a cesarean delivery number [Citation8]. In comparison to repeated cesarean, VBACs have been associated with lower maternal mortality, but higher perinatal mortality [Citation9]. Furthermore, the risk of uterine rupture has increased [Citation9].
According to a 10-year survey in the United States, the rates of successful VBAC in the United States vary between 38.5% and 69.8% [Citation10]. A study in Taiwan reported that the rate of VBAC among those mothers who attempted vaginal delivery was 85% [Citation11]. According to a large multicenter study in the United States in 2012, the total VBAC was 71.8%, and the rate rose with an increasing number of prior VBACs [Citation12].
The literature on maternal delivery and fetal outcomes in Finland is lacking. A recent study by Toijonen et al. found that higher rates of elective CS and emergency CS were found among women with pregnancies after previous preterm cesarean breech birth [Citation13]. Also, the need for neonatal intensive care unit treatment was higher in this group [Citation13]. Another study in 2017 found out that the rate of vaginal delivery was 72.9%, and the rate of repeat CS for failed induction or labor dystocia was 17.7% among TOLAC pregnancies [Citation14].
Even though the risks and advances of multiple repeat CSs and VBACs are well studied, epidemiological studies assessing the clinical importance of the effects of previous CS on maternal and fetal outcomes in subsequent deliveries are lacking. As the incidence of CS is currently rapidly increasing [Citation1,Citation2], studies assessing the effects of previous CS on maternal and fetal outcomes in subsequent pregnancies are warranted. The authors hypothesize that women with a trial of labor after cesarean section (TOLAC) have poorer maternal and fetal outcomes in subsequent pregnancies. The aim of this study is to evaluate the mode of delivery and fetal outcomes of the trial of labor after cesarean sections (TOLACs) using nationwide high-quality registers.
Materials and methods
In this nationwide retrospective register-based cohort study, data from the National Medical Birth Register (MBR), which is maintained by the Finnish Institute for Health and Welfare were used to evaluate the outcome of TOLACs, when compared to the outcome of a trial of labor in pregnancies following first successful vaginal delivery. All labors after CS, where vaginal delivery is attempted are defined as TOLACs (including urgent and emergency CS), whereas the term VBAC includes only those with successful vaginal delivery after CS. The MBR has high coverage and quality (the current coverage is nearly 100%) [Citation15,Citation16]. The study period was from 1st of January 2004 to December 31st, 2018.
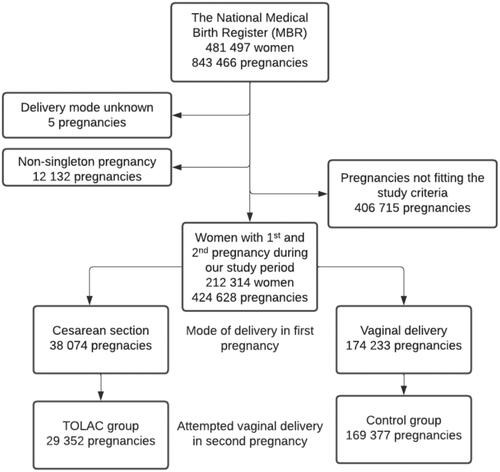
The MBR contains data on pregnancies, delivery statistics, and the perinatal outcomes of all births with a birthweight of ≥ 500 g or a gestational age of ≥ 22+0 weeks. All nulliparous women, who had their first and second singleton pregnancy during our study period, and with the mode of delivery identified in both of these pregnancies were included in this study. Pregnancies with unknown modes of delivery and non-singleton pregnancies were excluded from the analysis. Mothers who had only one pregnancy during our study period were excluded from the analysis. In addition, the 3rd or later pregnancies from the mothers included were also excluded from the analysis. Women with TOLAC were compared to the control group, consisting of women with successful vaginal delivery in their first pregnancy and trial of labor in 2nd pregnancy. In both trials of labor groups, women giving birth with elective CS were excluded. Successful vaginal delivery includes also breech, vacuum, and forceps deliveries. The process used to form the study groups is shown as a flowchart in .
Figure 1. Flowchart depicting the process used to divide the study population into groups. Trial of labors after cesarean section (TOLACs) were compared to the control group. Exclusion criteria for the pregnancies in this study were the following: Only the first and second pregnancies of the mother were included. However, pregnancies of mothers who had only one pregnancy during our study period were excluded from the analysis. In addition, women with a missing delivery mode in either of included pregnancies were excluded from the analysis.
Statistical analysis
Continuous variables were interpreted as means with standard deviations (SDs) or as a median with an interquartile range (IQR) based on the distribution of the data. The categorical variables are presented as absolute numbers and percentages. Student’s t-test, Mann–Whitney U-test, and Chi-Squared tests were used for group comparisons. A p-value under .05 was considered statistically significant. The multivariable logistic regression model was used to assess the primary outcome in attempted vaginal deliveries. Women with TOLAC were compared to the control group.
The exposure variable was the type of previous pregnancy (successful vaginal delivery/CS). The maternal outcome was the mode of delivery (successful vaginal delivery/urgent CS/emergency CS) in the second delivery of the mother. Unplanned CS includes urgent and emergency CS. Urgent CS is defined as a CS made on duty, but it is not an emergency situation, whereas emergency CS is performed when there is an immediate threat to the life of a fetus and/or mother. The model was adjusted by the smoking status of the mother, maternal length and pre-pregnancy body mass index (BMI, kg/m2), need for induction of labor, gestational weeks, birthweight, and age of the mother, shoulder dystocia, and 5-min Apgar points, as these are known to have an effect on the risk for urgent/emergency CS [Citation17–22]. The fetal outcome was the need for an intensive care unit and perinatal/neonatal mortality. The model for neonatal intensive care and perinatal/neonatal mortality was adjusted by maternal smoking status and gestational diabetes, as these are known to be risk factors for adverse health effects for the neonate [Citation23,Citation24]. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were used for comparisons. The aORs were calculated separately for urgent and emergency CS, neonatal intensive care unit treatment, and perinatal/neonatal mortality. Perinatal mortality included stillbirths, those who died during labor, and neonatal mortality up to 7 d of age. The results of this study are reported according to STROBE guidelines [Citation25]. The statistical analyses were conducted on R version 4.0.3 for Windows, developed by the R Foundation for Statistical Computing in Vienna, Austria.
Ethics
All methods were carried out in accordance with Finnish regulations. The ethical committee of Tampere university hospital has waived the ethical committee evaluation of all retrospective studies utilizing routinely collected healthcare data and this decision is based on the law of medical research 488/1999 and the law of patient rights 785/1992. In accordance with Finnish regulations (the Law on the secondary use of routinely collected healthcare data 552/2019), no ethical informed written consent was required because of the retrospective register-based study design, and the patients were not contacted. The authors did not have access to the pseudonymization key, as it is maintained by Findata. Permission for the use of the data was granted by Findata after the evaluation of the study protocol. (Permission number: THL/1756/14.02.00/2020)
Results
A total of 29 352 (77.0%) women attempted vaginal delivery in the TOLAC group. In the control group, 169 377 (97.2%) women attempted vaginal delivery after their first pregnancy. Women in the TOLAC group were older at the time of 2nd pregnancy than women in the control group (31.0 years vs. 29.6 years). A higher rate of women were confirmed smokers at the time of pregnancy in the TOLAC group (13.6% vs. 11.2%), compared to the control group. Women in the TOLAC group had a notably lower rate of successful vaginal deliveries (69.3% vs. 96.8%), a higher rate of urgent CS (28.3% vs. 2.7%), and a higher rate of emergency CS (2.4% vs. 0.5%) than women having a successful vaginal delivery as their first pregnancy. Also, the rate for vacuum deliveries was higher in the TOLAC group (16.0% vs. 3.0%). () Women in the TOLAC group had a higher rate of preterm deliveries when compared to the control group (5.5% vs. 3.6%). Lower rate of fetal asphyxia (umbilical arterial Ph < 7.00) was observed in the TOLAC group (6.5% vs. 11.6%). Of these, a higher rate of neonates required respiratory treatment in the TOLAC group (1.1% vs. 0.5%). ()
Table 1. Information on the study groups (at the time of the second pregnancy).
Table 2. Information on neonates and neonatal outcomes (at the time of second pregnancy).
In the logistic regression analyses, the adjusted odds for unplanned CS (28.3% vs. 2.7%; aOR 13.05, CI 12.59−13.65) and emergency CS (2.4% vs. 0.5%; aOR 3.65, CI 3.26−4.08) were notably higher in TOLAC group, when compared to the control group. In the models for fetal outcomes, the adjusted odds for neonatal intensive care unit treatment (13.2% vs. 6.8%; aOR 2.05, CI 1.98−2.14), perinatal mortality (0.5% vs. 0.3%; aOR 2.15, CI 1.79−2.57) and neonatal mortality (0.1% vs. 0.1%; aOR 1.75, CI 1.20−2.49) were all increased in TOLAC group, when compared to the control group. ()
Table 3. Adjusted odds ratios (aORs) with 95% confidence intervals (Cis) for delivery mode and fetal outcomes.
Discussion
The main finding of this study is that the odds for emergency CS were markedly higher among women with previous CS. Also, the odds for unplanned CS showed a markable increase, but as the indications for unplanned CS have such a large scale, precise conclusions based only on current register data should not be made. Furthermore, the need for neonatal intensive care unit treatment was higher in the TOLAC group, as were the rates of perinatal and neonatal mortality also.
The odds for emergency CS are interestingly high. Similar findings were observed in a recent study investigating the TOLAC outcomes after previous preterm cesarean breech birth [Citation13]. According to a study in 2013, the main risk factors for emergency CS in TOLACs were no prior vaginal delivery, index emergency cesarean during labor, maternal age ≥35 years, pre-pregnancy body mass index ≥30, and birthweight 4000–4499 g [Citation26]. However, due to the crude nature of our data, the reasons behind the notably higher rate of emergency CS among women with previous CS remains unknown. The register does not contain the indication for emergency CS and therefore we were unable to identify whether the increased need for emergency CS would be due to maternal or fetal emergencies. Our data doesn’t identify the event, where elective CS was converted into urgent CS due to the onset of labor before the scheduled elective CS and these are classified as urgent in the Finnish MBR. Therefore, the notably higher rate of emergency CS is a valid and important finding, as emergency CS is made based on strict criteria, and clear signs of danger either for the mother or for the fetus are required.
The rates of vacuum deliveries were also markedly higher in the TOLAC group. One possible explanation for this finding might be, that in the TOLAC group, there might be higher rates of labor dystocia and prolonged pregnancy, as these are known to be possible indications for urgent CS or vacuum-assisted delivery [Citation27,Citation28]. However, this topic has not been previously studied among TOLACs, as the previous studies are focused on the outcome of different delivery methods instead of the indications.
Based on our results, the total success rate for VBAC was 69.3%, which is similar to some of the findings in previous literature. In the United States, the success rate was found to be between 38.5% and 69.8% [Citation10]. In Taiwan, the success rate of VBAC among those mothers who ended up attempting vaginal delivery was 85% [Citation11]. According to a large multicenter study in 2012, the total success rate of VBAC was 71.8% [Citation12]. However, in the present study, only the first VBACs were included, which is most likely to decrease the success rate, as later VBACs after a successful VBAC are known to have a higher success rate [Citation12]. In previous literature it has been suggested that the most important goal to improve the VBAC rate is in the first VBAC after one CS [Citation29]. However, it has been also found that the risk of uterine rupture in TOLAC was not increased after two previous CS [Citation29]. The probability of VBAC is important to evaluate when considering TOLAC, as a failed VBAC increases the risk of maternal complications more than a repeat elective CS [Citation30,Citation31].
The adverse fetal outcomes were clearly higher in the TOLAC group. As the odds for neonatal intensive care were increased, it is important to acknowledge, that a notably higher rate of CS in the TOLAC group contributed to the increased odds of neonatal intensive care. Also, the higher rate of preterm deliveries in the TOLAC group partly explains the higher need for a neonatal intensive care unit. A recent study by Toijonen et al. also found higher odds for neonatal intensive care [Citation13], but the predicting model in this study was an unadjusted model, which most likely overestimates the observed results. Another recent population-based study found slightly higher odds for the need for neonatal intensive care, but the increase in this study was not as high (OR 1.12, 95% CI 1.09–1.16) as in our current study [Citation32]. Thus, the increased need for neonatal intensive care unit treatment should be noted when deciding the delivery method in the next pregnancy after a previous CS. Importantly, the odds for perinatal and neonatal mortality were clearly increased in the TOLAC group, which should be acknowledged in clinical decision-making. Although our current study can’t provide clear reasons for the increased mortality, raises it its reasons to concern. Future studies should focus on the optimal recognition of mothers, who may have TOLAC and those whose elective CS is recommended due to the increased risks in the neonatal period.
The strengths of our study are the large nationwide register data used and the long study period, which allowed us to analyze the VBACs using a large study population [Citation15,Citation16]. Register data used in our study are routinely collected in structured forms using national instructions, which ensures good coverage (over 99%) and reduces possible reporting and selection biases. The main limitation of this study is that the indications behind CS delivery are not registered in the MBR, which means that indications for these delivery methods remain unknown. Thus, it is unknown whether the patient had planned elective CS or attempted vaginal delivery before undergoing unplanned CS. Also, typical contraindications against TOLAC, such as uterine scar remain unknown in our data [Citation33]. Also, despite the many confounding factors available in our data, there are some confounding factors that are not available in our data, such as presentation, obstructed labor, fetal distress, duration of the labor, and maternal facility center which might have an influence on our results. According to previous literature, practice pattern is in fact a major driver of the variability of delivery modes across facilities [Citation4,Citation5,Citation34].
Conclusion
The odds for emergency CS were higher among women with TOLACs. The odds for neonatal intensive care and perinatal mortality were higher. Further research is needed to recognize expecting women better for TOLAC to minimize the risk for the neonate. The results of this study should be acknowledged by the mother and the clinician when considering the possibility of VBAC.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Betrán AP, Ye J, Moller AB, et al. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLOS One. 2016;11(2):e0148343.
- Niino Y. The increasing cesarean rate globally and what we can do about it. Biosci Trends. 2011;5(4):139–150.
- THL. Perinatal statistics – parturients, delivers and newborns – THL. 2018. Available from: https://thl.fi/en/web/thlfi-en/statistics-and-data/data-and-services/register-descriptions/newborns
- Cegolon L, Mastrangelo G, Heymann WC, et al. A systematic evaluation of hospital performance of childbirth delivery modes and associated factors in the friuli venezia giulia region (North-Eastern Italy), 2005–2015. Sci Rep. 2019;9(1):19442.
- Cegolon L, Mastrangelo G, Maso G, et al. Understanding factors leading to primary cesarean section and vaginal birth after cesarean delivery in the Friuli-Venezia Giulia region (North-Eastern Italy), 2005–2015. Sci Rep. 2020;10(1):380.
- Optimal C-section rate may be as high as 19 percent to save lives of mothers and infants. News Center. 2015. [cited 2023 March 14]. Available from: http://med.stanford.edu/news/all-news/2015/12/optimal-c-section-rate-may-be-as-high-as-19-percent-to-save-lives.html
- Gasim T, Jama A, Rahman FE, et al. J. Multiple repeat cesarean sections: operative difficulties, maternal complications and outcome. J Reprod Med. 2013;58(7–8):312–318.
- Nisenblat V, Barak S, Griness OB, et al. Maternal complications associated with multiple cesarean deliveries. Obstet Gynecol. 2006;108(1):21–26.
- Guise JM, Denman MA, Emeis C, et al. Vaginal birth after cesarean: new insights on maternal and neonatal outcomes. Obstet Gynecol. 2010;115(6):1267–1278.
- Uddin SFG, Simon AE. Rates and success rates of trial of labor after cesarean delivery in the United States, 1990–2009. Matern Child Health J. 2013;17(7):1309–1314.
- Tsai HT, Wu CH. Vaginal birth after cesarean section—The world trend and local experience in Taiwan. Taiwan J Obstet Gynecol. 2017;56(1):41–45.
- Stamilio DM, Shanks A. Vaginal birth after cesarean (VBAC) outcomes associated with increasing number of prior VBACs. Womens Health. 2008;4(3):233–236.
- Toijonen A, Hinnenberg P, Gissler M, et al. Maternal and neonatal outcomes in the following delivery after previous preterm caesarean breech birth: a national cohort study. J Obstet Gynaecol. 2022;42(1):49–54.
- Place K, Kruit H, Tekay A, et al. Success of trial of labor in women with a history of previous cesarean section for failed labor induction or labor dystocia: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):176.
- Gissler M, Shelley J. Quality of data on subsequent events in a routine medical birth register. Med Inform Internet Med. 2002;27(1):33–38.
- Gissler M, Teperi J, Hemminki E, et al. Data quality after restructuring a national medical registry. Scand J Soc Med. 1995;23(1):75–80.
- Lurie S, Ribenzaft S, Boaz M, et al. The effect of cigarette smoking during pregnancy on mode of delivery in uncomplicated term singleton pregnancies. J Matern Fetal Neonatal Med. 2014;27(8):812–815.
- Bergholt T, Skjeldestad FE, Pyykönen A, et al. Maternal age and risk of cesarean section in women with induced labor at term—A nordic register-based study. Acta Obstet Gynecol Scand. 2020;99(2):283–289.
- Mogren I, Lindqvist M, Petersson K, et al. Maternal height and risk of caesarean section in singleton births in Sweden—A population-based study using data from the Swedish pregnancy register 2011–2016. PLOS One. 2018;13(5):e0198124.
- Mishanina E, Rogozinska E, Thatthi T, et al. Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. CMAJ. 2014;186(9):665–673.
- Bjorklund J, Wiberg-Itzel E, Wallstrom T. Is there an increased risk of cesarean section in obese women after induction of labor? A retrospective cohort study. PLOS One. 2022;17(2):e0263685.
- Roos N, Sahlin L, Ekman-Ordeberg G, et al. Maternal risk factors for postterm pregnancy and cesarean delivery following labor induction. Acta Obstet Gynecol Scand. 2010;89(8):1003–1010.
- Mitanchez D, Yzydorczyk C, Simeoni U. What neonatal complications should the pediatrician be aware of in case of maternal gestational diabetes? World J Diabetes. 2015;6(5):734–743.
- Knopik VS. Maternal smoking during pregnancy and child outcomes: real or spurious effect? Dev Neuropsychol. 2009;34(1):1–36.
- von EE, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349.
- Studsgaard A, Skorstengaard M, Glavind J, et al. Trial of labor compared to repeat cesarean section in women with no other risk factors than a prior cesarean delivery. Acta Obstet Gynecol Scand. 2013;92(11):1256–1263.
- Levin G, Tsur A, Rottenstreich A, et al. The association of vacuum-assisted delivery and shoulder dystocia among macrosomic newborns: a retrospective study. Arch Gynecol Obstet. 2021;304(1):117–123.
- Nolens B, van den Akker T, Lule J, et al. Women’s recommendations: vacuum extraction or caesarean section for prolonged second stage of labour, a prospective cohort study in Uganda. Trop Med Int Health. 2019;24(5):553–562.
- Barber EL, Lundsberg LS, Belanger K, et al. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38.
- McMahon MJ, Luther ER, Bowes WA, et al. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med. 1996;335(10):689–695.
- Wu Y, Kataria Y, Wang Z, et al. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19:360.
- Litwin CE, Czuzoj-Shulman N, Zakhari A, et al. Neonatal outcomes following a trial of labor after caesarean delivery: a population-based study. J Matern Fetal Neonatal Med. 2018;31(16):2148–2154.
- Landon MB, Spong CY, Thom E, et al. Risk of uterine rupture with a trial of labor in women with multiple and single prior cesarean delivery. Obstet Gynecol. 2006;108(1):12–20.
- Schemann K, Patterson JA, Nippita TA, et al. Variation in hospital caesarean section rates for women with at least one previous caesarean section: a population based cohort study. BMC Pregnancy Childbirth. 2015;15:179.

