Abstract
Objective
Term prelabour rupture of membrane (PROM) occurs in 8% of term deliveries, but it is unclear when to initiate induction. Our objective was to assess the optimal timing of oxytocin induction in the management of term PROM in terms of maternal and neonatal outcomes.
Methods
A retrospective cohort study was performed at a single tertiary care center from 2010 to 2020. All singleton pregnancies with PROM beyond 37 weeks gestation, without regular uterine contractions, were included. Eligible women were divided into three groups according to the timing of oxytocin induction (≤12; 12–24; ≥24 h) following PROM.
Results
Of 9,443 women presented with the term PROM, 1676 were included. They were classified according to the timing of oxytocin induction initiation following PROM: 1,127 within 12 h; 285 within 12–24 h; 264 after 24 h. There were no significant differences in baseline demographic characteristics between groups. Women who presented at our emergency department were induced earlier delivered significantly sooner than those who received oxytocin later (45 vs. 28.2 vs. 23.2 h, respectively, p < .001. Maternal infection rate was similar and unrelated to oxytocin starting time. Induction at <12 h from PROM was associated with reduced rate of antibiotic administration compared with other timings (26.8% vs. 38.6% vs. 33.33%, respectively; p < .001), and the same was found for neonatal composite adverse outcomes (RR = 1.27, p = .0307).
Conclusion
In term PROM, early induction (within 12 h of PROM) may be recommended to reduce the time-do-delivery interval and increase the delivery rate within 24 h. It may be of economic significance and improve women satisfaction. Furthermore, early induction may also improve neonatal outcomes, without worsening maternal outcomes.
Introduction
Prelabor rupture of the membranes (PROM) refers to the rupture of the fetal membranes prior to the onset of regular uterine contractions [Citation1]. Term PROM is referred to ruptured membranes beyond 37 + 0/7 weeks of gestation. The frequency of the term PROM in the Unites States is estimated as 8% of pregnancies [Citation2,Citation3]. Previous prospective studies have shown that 60% of these primiparous women with term PROM will give birth within 24 h, and over 95% will begin delivery within 72 h [Citation4–6]. These results are also consistent for women with an unfavorable cervix [Citation4].
PROM at term can be managed actively by induction of labor or expectantly by waiting for the onset of spontaneous contractions. Several studies have shown an association between expectant management and higher rates of maternal and neonatal adverse outcomes, especially infections [Citation5,Citation6]. Furthermore, expectant management has been shown to increase the risk for cesarean delivery, cerebral palsy, neonatal chronic lung disease, and neonatal mortality [Citation2,Citation7–10]. It is suggested that the risk for those complications increases proportionally with the longer the duration of ruptured membranes [Citation5,Citation11], but other studies found different results [Citation7,Citation12].
As a consequence, there is contrasting evidence about which strategy is superior, between active and expectant management. Candidates for expectant management include women with vertex presentation, reassuring fetal testing, no contraindications for vaginal delivery, and no signs or symptoms of infection. When PROM occurs, there are several methods for induction of labor, including oxytocin infusion, mechanical induction (balloon ripening), or chemical induction (prostaglandin E1/E2). In contrast to other indications for labor induction, there is no benefit for cervical ripening in PROM induction, compared with direct use of oxytocin, even in women with unfavorable cervix [Citation13–15].
A recent Cochrane review [Citation3] assessed maternal, fetal, and neonatal effects of planned early induction when compared with expectant management for women with term PROM. Data from 23 randomized controlled trials included 8615 women. The largest study in this review was conducted by Hannah et al. in 1998 [Citation4] and included more than 5000 heterogeneous women (nulliparous and multiparous) who were randomized either for induction of labor (by either oxytocin or prostaglandins), or for expectant management (up to 4 d). They found a significant reduction in maternal infectious morbidity (clinical chorioamnionitis and endometritis) in women who were induced with oxytocin versus expectant management, with no difference in neonatal infection or cesarean delivery rate between the groups [Citation7]. As a result of that study, The Cochrane review was in favor of planned intervention following PROM at term [Citation3]. However, most studies in that review were of poor quality, making those conclusions questionable. Additionally, the studies differed in parity, time of expectant management and mode of induction. According to The American College of Obstetricians and Gynecologists (ACOG), it is recommended to initiate early induction in case of term PROM, even when maternal and fetal status are reassuring. However, a short period (12–24 h) of expectant management may be offered [Citation15].
Methods
Study design and population
This was a retrospective cohort study of pregnant women admitted to the labor and delivery unit with PROM beyond 37 + 0/7 weeks of gestation, in a university-affiliated medical center between January 2010 and December 2020. The study was approved by the local Research Ethics Board (RMB-0017-20), waiving informed consent for de-identified patient information acquisition. Information collected from the hospital’s database included access to the following variables: demographic information, medical history, obstetric history, and intrapartum and postpartum maternal-fetal variables.
Women presented with the term PROM who received oxytocin induction were divided into three groups according to induction starting time: within 12 h of membrane rupture (early group); between 12 and 24 h of membrane rupture (intermediate group) and beyond 24 h of membrane rupture (delayed group). Exclusion criteria included women who were in active labor or had regular contractions; women with contraindication for vaginal delivery, had a previous uterine scar, non-vertex presentation; non-reassuring fetal status, positive group B streptococcus colonization, or meconium fluid. We also excluded women who underwent expectant management.
The primary outcome of the study was defined as the time from PROM to delivery. Maternal secondary outcomes included: infectious morbidity (fever >38° or uterine tenderness), mode of delivery, episiotomy rate, postpartum hemorrhage (PPH) rate, and total length of hospitalization following delivery. Prolonged hospitalization was defined as more than 2 d following vaginal delivery, or more than 5 d following cesarean delivery. A composite of adverse maternal events consisted of one or more of the following: PPH, intrapartum fever, chorioamnionitis or endometritis.
Neonatal secondary outcomes included: Apgar score, rate of neonatal intensive care unit (NICU) admissions, antibiotic use, rates of cerebral palsy (CP), apnea, hypotonia, seizures, and need for resuscitation. A composite of adverse neonatal events consisted of one or more of the following: Apgar score at 5 min <7, NICU admission, antibiotic administration, cerebral palsy, apnea, hypotonia, seizures, and resuscitation.
Decision-making has been upon physician consideration at our unit, whether to augment labor or not by oxytocin infusion. This practice has not changed in the last 10 years during the time of the study. The aim of our study was to determine the optimal timing of oxytocin induction in term PROM, regardless of Bishop score.
Statistical analyses
Maternal and neonatal characteristics were compared using the chi-squared test or Fisher exact test for categorical variables, whereas continuous variables were compared using ANOVA (or Kruskal–Wallis test). Pairwise comparisons were made using Chi-square test (or Fisher’s exact test) for categorical variables, and t-test (or Wilcoxon rank sum test). Bonferroni correction was implemented to adjust for multiple comparisons. The statistical analysis was carried out using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA). p < .05 was considered significant unless otherwise stated.
Results
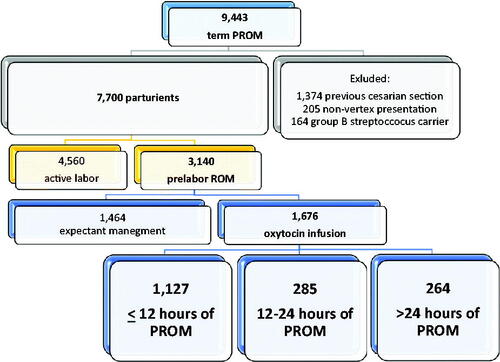
The study included 9443 women who were admitted to labor and delivery unit with ruptured membranes beyond 37 weeks of gestation. Of them, 1374 (14.5%) were excluded due to previous cesarean delivery, 205 (2.1%) due to non-vertex presentation, and 164 (1.7%) due to group B streptococcus carrier status. Of the remaining 7700 patients, 4560 women were admitted with regular contractions in active labor. The final analysis included 3140 women with PROM. Out of them, 1464 had expectant management and 1676 patients received oxytocin infusion: 1127 within 12 h of PROM; 285 between 12 and 24 h of PROM and 264 more than 24 h of PROM initiation ().
Baseline characteristics are presented in . There were no significant differences in baseline characteristics among the three groups who received oxytocin, including age, parity, gestational week at delivery, medical and obstetric history, or cervical dilation at the time of PROM ().
Table 1. Maternal baseline characteristics, by oxytocin administration timing.
Delivery outcomes are details in . Early (within 12 h of PROM) administration induction resulted in a shorter interval from membrane rupture to delivery, compared with intermediate (within 12–24 h of PROM) and delayed oxytocin induction (>24 h of PROM) administration (23.2 h vs. 28.2 h vs. 45 h, respectively, p < .001). There were no differences in cesarean delivery rates among groups, nor the rate of episiotomy. PPH rate was higher in delayed oxytocin infusion group compared with early administration (4.55% vs. 2.04%, p = .034). Intrapartum fever rate was similar between early, intermediate, and delayed groups (5.68% vs. 7.37% vs. 4.92%, respectively, p > .05). Other infectious variables (chorioamnionitis and endometritis) were also similar between all three groups (p > .05). However, women receiving intermediate oxytocin infusion stayed longer in the hospital following their delivery compared with those who received early oxytocin induction (4 d vs. 3 d, p = .002) ().
Table 2. Delivery outcomes, by oxytocin administration timing.
Newborn characteristics are presented in . Gender, birthweight, and Apgar scores were similar between groups (p > .05). NICU admission rate was low in three groups, without significant differences. Yet, when mothers received early oxytocin induction, less newborns needed additional antibiotic treatment, compared with intermediate and delayed induction groups (26.8% vs. 38.6% vs. 33.33%, respectively, p < .001). Neonatal composite adverse outcome, which is reflected especially by neonatal antibiotic use, was less common in early oxytocin induction group, compared with intermediate and delayed groups (27.42% vs. 38.95% vs. 34.47%, respectively, p < .001). We performed a multivariable regression analysis after adjusting to confounding factors and found a significant reduction in neonatal composite adverse outcome with early oxytocin induction compared to intermediate oxytocin induction (RR 1.27, p = .0307, ).
Table 3. Newborn characteristics and outcomes, by oxytocin intake.
Table 4. Multivariable log-binomial regression for the study outcomes.
Discussion
Main findings
In this study, we evaluated maternal and neonatal adverse outcomes in women coming with prelabor rupture of membranes who received oxytocin induction. Women were divided to three groups according to oxytocin infusion beginning time. Our main findings were as follows: (1) Maternal infection rate was similar and unrelated to oxytocin starting time; (2) Women who were induced within 12 h from ruptured membranes delivered sooner than those who received oxytocin later; (3) Newborns of mothers who received early oxytocin were less likely to receive antibiotics; (4) Composite adverse neonatal outcome was less prevalent with early oxytocin induction; (5) Early oxytocin induction shortened maternal hospital stay.
Comparison with existing literature
Previous studies presented maternal infectious morbidity rate ranging from 2-33%, and as expected, the longer the ruptured membrane duration, the higher the infection rate [Citation16–20]. However, those studies used variable definitions for maternal infectious morbidity (clinical diagnosis [Citation19], fever [Citation21,Citation22], leukocytosis [Citation23], and more [Citation17]). Furthermore, they compared oxytocin use versus expectant management and not different initiation time of oxytocin, so there is no data to support the optimal timing of induction in PROM. Hannah et al. [Citation23], which investigated this topic and conducted the largest study to date, showed a significant increase in maternal infectious morbidity in the expectant management group compared to immediate induction group (8.63% vs. 3.97%, RR = 0.61, p < .05) while waiting up to 4 d in the expectant management group. Other studies [Citation19–21,Citation23] did not find a significant difference in maternal infectious morbidity, although study populations were small (62–268 participants). Not showing a difference in maternal infectious rate in our cohort may be related to a small sample size, and a shorter duration for expectant management.
As may have been expected, women in the early induction group were more likely to deliver sooner, up to 23 h on average from ruptured membranes, compared with intermediate and delayed induction groups (28 and 45 h, respectively, p < .001). This is consistent with previous studies [Citation21,Citation24]. Prolonged stay in labor and delivery unit may cause women and their partners to be frustrated and exhausted. Furthermore, women may be restricted to bed due to epidural analgesia. In overall, it may decrease their satisfaction and harm the whole birth experience.
Most studies [Citation19,Citation21,Citation22,Citation24] correlate to ours with regards to antibiotic administration to newborns. The longer women waited to receive oxytocin, the higher the rate of neonate’s antibiotic use. Undiagnosed and/or untreated sepsis can lead to neonatal mortality or long-term morbidity, and antibiotic treatment decrease these devastating outcomes. However, these drugs can exert unintended consequences, including disruption of the neonatal microbiota [Citation25,Citation26] so they should be used with caution. If we can accomplish that by initiating oxytocin sooner (within 12 h) rather than later, that should be taken into consideration while counseling patients with regards to induction versus expectant management, and timing of induction.
Neonatal adverse outcome (cerebral palsy, apnea, seizures, etc.) in term PROM is known to be low [Citation27–31], and likewise in our cohort. We found that babies of women who received oxytocin induction within 12 h of PROM had lower rates of neonatal composite adverse outcome, especially antibiotic treatment. Previous studies did not use a similar composite outcome, but isolated neonatal complications were low and similar between induction and expectant management groups [Citation20,Citation22,Citation24]. A recent study conducted by Mynarek et al. [Citation31] showed that an intervals greater than 24 h between PROM and delivery was associated with CP, although it was not related to neonatal mortality or death during delivery.
Our study presented a shorter median maternal hospitalization in the early oxytocin induction group, and so did Shalev et al. and Wagner et al. [Citation20,Citation21] in their study. Length of hospitalization may pose a financial burden on the health care system, and it should also be considered when opting to induce women with PROM versus managing those women expectantly.
Strengths and limitations
Given the retrospective design of this study, some information was not available. Nonetheless, our study included a relatively large cohort of women with PROM who received oxytocin induction, demonstrating a different aspect of view and its potential effect on care provider management. This management may affect maternal and neonatal outcomes.
Conclusions and implications
Our study demonstrates that early induction of Term PROM shortens the time from PROM-to-Delivery, which can be responsible for a lower rate of antibiotics use for neonates, lower adverse neonatal outcome, and shorter maternal hospital stay. Additionally, there is an economic importance to those findings. We assume that shortening the time to delivery may also influence maternal satisfaction, which should be examined in a prospective study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Duff P. Premature rupture of the membranes in term patients: induction of labor versus expectant management. Clin Obstet Gynecol. 1998;41(4):883–891.
- Cammu H, Verlaenen H, Derde MP. Premature rupture of membranes at term in nulliparous women: a hazard? Obstet Gynecol. 1990;76(4):671–674.
- Middleton P, Shepherd E, Flenady V, et al. Planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more). Cochrane Database of Syst Rev. 2017;1(1):CD005302.
- Hannah ME, Seaward GR. Prelabour rupture of membranes at term: the role of induction of labour. Fet Matern Med Rev. 1998;10(2):61–68.
- Alexander JM, Cox SM. Clinical course of premature rupture of the membranes. Semin. Perinatol. 1996;20(5):369–374.
- Kong AS, Bates SJ, Rizk B. Rupture of membranes before the onset of spontaneous labour increases the likelihood of instrumental delivery. Br J Anaesth. 1992;68(3):252–255.
- Gonen R, Hannah ME, Milligan JE. Does prolonged preterm premature rupture of the membranes predispose to abruptio placentae? Obstet Gynecol. 1989;74(3 Pt 1):347–350.
- Merenstein GB, Weisman LE. Premature rupture of the membranes: neonatal consequences. Semin Perinatol. 1996;20(5):375–380.
- Robson MS, Turner MJ, Stronge JM, et al. Is amniotic fluid quantitation of value in the diagnosis and conservative management of prelabour membrane rupture at term? BJOG. 1990;97(4):324–328.
- Zlatnik FJ. Management of premature rupture of membranes at term. Obstet Gynecol Clin North Am. 1992;19(2):353–364.
- Tan BP, Hannah M. Prostaglandins versus oxytocin for prelabour rupture of membranes at term. Cochrane Database Syst Rev. 2000; CD000159. DOI:10.1002/14651858.CD000159
- Hofmeyr GJ, Gülmezoglu AM, Pileggi C. Vaginal misoprostol for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2010;2010(10):CD000941.
- Lin MG, Nuthalapaty FS, Carver AR, et al. Misoprostol for labor induction in women with term premature rupture of membranes: a meta-analysis. Obstet Gynecol. 2005;106(3):593–601.
- Cecco R, Hannah M, Hodnett E, et al. Prelabor rupture of the membranes (PROM) at term: expectant management at home vs in hospital. Am J Obstet Gynecol. 1998;96(4):533–538. DOI:10.1016/s0029-7844(00)00971-6
- ACOG. Prelabor rupture of membranes: ACOG practice bulletin, number 217. Obstet Gynecol. 2020;135(3):e80–e97.
- Hannah ME, Ohlsson A, Farine D, et al. Induction of labor compared with expectant management for prelabor rupture of the membranes at term. N Engl J Med. 1996;334(16):1005–1010.
- Natale R, Milne JK, Campbell MK, et al. Management of premature rupture of membranes at term: randomized trial. Am J Obstet Gynecol. 1994;171(4):936–939.
- Shalev E, Peleg D, Eliyahu S, et al. Comparison of 12- and 72-Hour expectant management of premature rupture of membranes in term pregnancies. Obstet Gynecol. 1995;85(5 Pt 1):766–768.
- Sperling LS, Schantz AL, Wåhlin A, et al. Management of prelabor rupture of membranes at term: a randomized study. Acta Obstet Gynecol Scand. 1993;72(8):627–632.
- Wagner MV, Chin VP, Peters CJ, et al. A comparison of early and delayed induction of labor with spontaneous rupture of membranes at term. Obstet. Gynecol. 1989;74(1):93–97.
- Akyol D, Mungan T, Unsal A, et al . Prelabour rupture of the membranes at term – No advantage of delaying induction for 24 hours. Aust N Z J Obstet Gynaecol. 1999;39(3):291–295.
- Peterson CT, Sharma V, Elmén L, et al. Immune homeostasis, dysbiosis and therapeutic modulation of the gut microbiota. Clin Exp Immunol. 2015;179(3):363–377.
- Hannah ME, Ohlsson A, Farine D, et al. Induction of labor compared with expectant management for prelabor rupture of the membranes at term. Obstet Gynecol Surv. 1996;334(16):1005–1010.
- Laws M, Shaaban A, Rahman KM. Antibiotic resistance breakers: current approaches and future directions. FEMS Microbiol Rev. 2019;43(5):490–516.
- Oskoui M, Coutinho F, Dykeman J, et al. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55(6):509–519.
- Hirvonen M, Ojala R, Korhonen P, et al. Cerebral palsy among children born moderately and late preterm. Pediatrics. 2014;134(6):e1584–e1593.
- Henderson-Smart DJ. The effect of gestational age on the incidence and duration of recurrent apnoea in newborn babies. J Paediatr Child Health. 1981;17(4):273–276.
- Amiel-Tison C, Maillard F, Lebrun F, et al. Neurological and physical maturation in normal growth singletons from 37 to 41 weeks’ gestation. Early Hum Dev. 1999;54(2):145–156.
- Glass HC, Pham TN, Danielsen B, et al. Antenatal and intrapartum risk factors for seizures in term newborns: a population-based study, California 1998–2002. J Pediatr. 2009;154(1):24.e1–28.e1.
- Ottervanger HP, Keirse MJNC, Smit W, et al. Controlled comparison of induction versus expectant care for prelabor rupture of the membranes at term. J Perinat Med. 1996;24(3):237–242.
- Mynarek M, Bjellmo S, Lydersen S, et al. Prelabor rupture of membranes and the association with cerebral palsy in term born children: a national registry-based cohort study. BMC Pregnancy Childbirth. 2020;20(1):67.