?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: To evaluate the changes in cardiac morphology of fetuses with congenital heart disease (CHD) using the fetal heart quantitative technique (fetalHQ).
Methods: A total of 20 normal pregnant women (control group) and 20 pregnant women suspected of fetal CHD (case group) were included in this study. The dynamic images of the four-chamber view of the fetal heart were recorded and analyzed using fetalHQ. The global sphericity index (GSI) and 24-segment SI of the two groups were compared. The differences in the left and right ventricular 24-segment SI for each group were investigated.
Results: There was no statistically significant difference in the GSI between the two groups (p > 0.05). The difference in the SI values of left ventricular segments 1–2 between the case group and control group was statistically significant (all p < 0.05), while the intergroup difference in SI of left ventricular segments 3–24 was not significant (all p > 0.05). The SI of the 24 segments of the right ventricle showed no significant intergroup difference (all p > 0.05). The difference in the left and right ventricular 24-segment SI in the case group did not reach statistical significance (all p > 0.05). In the control group, the SI values between the left and right ventricles were significantly different in segments 18–24 (all p < 0.05), and no significant difference was found in segments 1–17 (all p > 0.05). There was a statistically significant intergroup difference in the percentage of unusual left ventricular SI, determined based on Z-score (p < 0.05), and the percentage of outliers for the right ventricle between the two groups showed no significant difference (p > 0.05).
Conclusion: The fetalHQ is regarded as a straightforward and reliable approach for assessing the cardiac GSI and 24-segment SI of left and right ventricles in fetuses diagnosed with CHD. While CHD may not significantly impact the overall shape of the fetal heart or the geometric shape of the right ventricle, in this study, a notable increase in SI values for the left ventricular 1–2 segments was observed, indicating a more flattened ventricular chamber. Additionally, the morphological distinctions between the left and right ventricles in fetuses with CHD are no longer discernible.
Introduction
Congenital heart disease (CHD) is the most common birth defect during the fetal period. It often leads to cardiac dysfunction and blood circulation disorders and is recognized as the most prevalent cause of death in newborns. The evaluation of fetal cardiac function is an essential part of fetal echocardiography, which can provide important information on fetal hemodynamic status and cardiovascular adaptation. The information can help to assess intrauterine conditions, determine the optimal delivery time, and reduce perinatal morbidity and mortality [Citation1]. The fetal heart quantitative technique (fetalHQ) is a new approach developed based on speckle-tracking technology. It can evaluate the global sphericity index (GSI) and divide the left and right ventricles into 24 segments, respectively, and automatically measure the SI of each segment. Our previous study has demonstrated that fetalHQ can reliably evaluate GSI and 24-segment SI of the fetal heart [Citation2]. In the current study, the GSI and 24-segment SI of the fetal heart with CHD were assessed using fetalHQ to explore its clinical application value.
Subjects and methods
A retrospective study was conducted at the Maternal and Child Health Care Hospital of Hunan Province from September to October 2022. A total of 20 normal pregnant women with a gestational age (GA) of 29.0 ± 3.5 weeks (control group) and 20 pregnant women suspected of fetal CHD with a GA of 26.7 ± 4.3 weeks (case group) were included in this study. The average age of the two groups of pregnant women was 30.7 ± 3.5 years and 32.1 ± 5.4 years, respectively. Data on normal fetuses were collected from low-risk and healthy pregnant women. The pregnant women in the case group all meet the following inclusion criteria: singleton pregnancies; a GA of 20–40 weeks; the presence of fetal congenital heart defects, such as ventricular septal defect, aortic coarctation, and persistent left superior vena cava (); the absence of oligohydramnios or polyhydramnios, fetal growth restriction, and maternal metabolic and systemic diseases, such as gestational diabetes and hypertension; good-quality images. Written informed consent was obtained from all families involved. This study was approved by the Ethics Committee of Hunan Provincial Maternal and Child Health Care Hospital.
Table 1. The types of fetuses with suspected CHD in 20 cases.
All examinations were performed using a Voluson E10 ultrasound system (GE Healthcare Ultrasound, Milwaukee, WI, USA) with a curved array transabdominal transducer (1–7 MHz). Fetal echocardiographic examinations were conducted by two experienced examiners (LYC and ZC). After routine ultrasound examinations and fetal biometric parameter measurement, a four-chamber dynamic view was obtained using a transabdominal probe with the recommended frame rate (greater than 80 Hz). In addition, images were collected when the fetus was relatively still, as recommended.
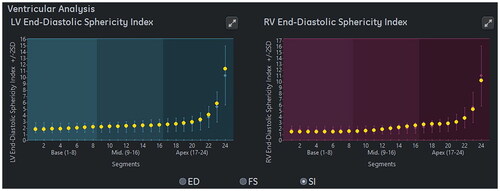
Fetal cardiac SI was evaluated using fetalHQ by one operator (ZMX) who was blinded to the clinical data. As described in previous research [Citation3,Citation4], GSI, ventricular 24-segment SI and Z scores were calculated automatically by fetalHQ based on speckle-tracking imaging. Z scores > 2 or < −2 indicate outliers. As shown in , fetalHQ displayed the SI values of left and right ventricular 24 segments at end-diastole.
Figure 1. fetalHQ displayed the SI values of left and right ventricular 24 segments at end-diastole.

Data analyses were performed using SPSS 26 for Windows (IBM, Armonk, NY, USA). Continuous data were presented as the mean ± standard deviation. The Shapiro-Wilk test was carried out to assess the normality of the distribution. The left and right ventricular 24-segment SI values in each group were compared by the paired-sample t-test. The fetal GSI and ventricular 24-segment SI between the two groups were compared by the independent samples t-test. The interclass correlation coefficient (ICC) was adopted to assess interobserver agreement for 10 randomly selected observations. Fisher’s exact test and chi-square test were performed to compare the percentage of unusual left and right ventricular SI values, determined based on Z-scores, between the two groups. p < 0.05 was considered statistically significant.
Results
Comparison of the GSI between the two groups of fetuses
The GSI of the case group was 1.27 ± 0.12, and one fetus (5%, 1/20) had an unusual GSI (Z-score > 2). The GSI of the control group was 1.27 ± 0.08, with one case (5%, 1/20) of unusual value (Z-score > 2). There was no statistically significant difference in the GSI of the two groups (p > 0.05).
Comparison of the ventricular 24-segment SI between the two groups of fetuses
There were significant differences in the SI values in segments 1–2 of the left ventricle between the case group and control group (all p < 0.05), but there was no significant difference in the SI values of segments 3–24 (all p > 0.05). Specifically, the SI values of the left ventricular segments 1–2 in the case group were greater than those in the control group, indicating that the left ventricular segments 1–2 of the case group were more like a bullet (). In contrast, the SI values of the 24 right ventricle segments in the two groups did not show significant differences (all p > 0.05), as shown in .
Table 2. Comparison of left ventricular 24-segment SI between the two groups.
Table 3. Comparison of right ventricular 24-segment SI between the two groups.
Ten fetuses (50%, 10/20) in the case group had unusual left ventricular 24-segment SI values, which were found in a total of 69 segments (14.38%, 69/480), including 39 segments with Z-scores > 2 and 30 segments with Z-scores < −2. Seven fetuses in the case group (35.00%, 7/20) had unusual right ventricular 24-segment SI values, which occurred in a total of 57 segments (11.89%, 57/480), including 50 segments with Z-scores > 2 and 7 segments with Z-scores < −2. For the 20 fetuses in the control group, their left ventricular 24-segment SI values were usual. However, five fetuses (25.00%, 5/20) had unusual right ventricular 24-segment SI values, which were found in a total of 50 segments (10.42%, 50/480) (all Z-scores > 2). There was a statistically significant difference in the percentage of unusual left ventricle SI between the two groups (p < 0.05), and the differences in the percentage of unusual right ventricular SI between the two groups were not significant (p > 0.05).
Comparison of the left and right ventricular 24-segment SI in each group
There was no statistically significant difference in the left and right ventricular 24-segment SI of the case group (all p > 0.05). In the control group, the SI values of segments 18–24 of the left and right ventricles were significantly different (all p < 0.05), but there was no significant difference in the SI values of segments 1–17 (all p > 0.05) (as shown in and ).
Table 4. Comparison of left and right ventricular 24-segment SI in the case group (n = 20).
Table 5. Comparison Of left and right ventricular 24-segment SI in the control group (n = 20).
Repeatability evaluation
The ICCs for the fetal GSI in the case group and control group were 0.872 (95% CI, 0.706–0.947) and 0.809 (95% CI, 0.579–0.920), respectively, which indicates good consistency. The left and right ventricular 24-segment SI in each group showed high consistency (all ICC > 0.75).
Discussion
The congenital structural defects in the fetal heart may change the left and right heart loads, potentially leading to abnormal cardiac morphology and function. Moreover, the deterioration of cardiac function is closely related to ventricular remodeling; specifically, it may change the ventricular shape (from oval to spherical) and increase the end-diastolic volume [Citation4,Citation5]. Usually, fetal cardiac function is evaluated through M-mode ultrasound and Doppler. Over the years the advances in ultrasound technology, speckle-tracking technique and three-dimensional ultrasound have gradually been used for fetal heart function assessment [Citation6]. Previous studies have shown that speckle-tracking technique can effectively evaluate the shape, size, and function of the fetal heart in CHD and intrauterine growth restriction, and even to evaluate the fetus at risk for interventricular septum hypertrophy by measuring of the area and length of the interventricular septum in the four-chamber view [Citation7–15]. FetalHQ is an automatic fetal cardiac function assessment tool. It not only evaluates the size and shape of the fetal heart, but also uses speckle-tracking technique to perform 24-segment analysis of the left and right ventricle of the fetal heart, thereby more accurately quantitatively assessing the systolic function of the left and right ventricle. In a previous study, we demonstrated that fetalHQ is a simple and reliable method for evaluating the GSI and 24-segment SI, and the information obtained by this method can provide a theoretical basis for quantitative clinical evaluation of fetal heart geometry [Citation2].
In the present study, unusual GSI was present in only one fetus (5%) in each group. The GSI of the fetal heart between the case group and control group was compared, and no statistically significant differences were found (p > 0.05), indicating that CHD had no significant impact on the overall morphology of the fetal heart. However, DeVore et al. showed that the GSI below the 5th percentile (< 1.08) was responsible for abnormal fetal ultrasound findings, such as fetal heart malformations and aneuploidy [Citation16], with a positive predictive value of up to 96%, which was inconsistent with the result of the present study. The reason for this inconsistency may be that the focus of the two studies is different. In addition, Tan et al. reported that hypertensive disorders during pregnancy had no significant effect on fetal heart morphology [Citation17].
The present study showed that the SI values of left ventricular segments 1–2 in the case group were significantly greater than those in the control group, suggesting that fetal CHD significantly impacted the morphology of left ventricular segments 1–2, and led to a more flattened ventricular chamber. DeVore et al. reported that fetuses with cardiac structural abnormalities and growth abnormalities had unusual SI values, resulting in a more spherical or flat morphology of ventricles [Citation3]. Our study further confirmed that fetal CHD could cause unusual left ventricular SI values, leading to left ventricular flattening. The difference in right ventricular 24-segment SI between the two groups was not significant, suggesting that fetal CHD had no significant effect on right ventricular morphology. In summary, fetal CHD did not significantly affect the overall shape of the fetal heart and the morphology of the right ventricle but changed the shape of the left ventricle, especially the basal segments 1–2, which were made more like a bullet. The percentage of unusual left ventricular SI of fetuses with CHD was significantly higher than that in the control group, while the percentage of unusual right ventricular SI between the two groups had no significant statistical difference. DeVore et al. used speckle-tracking technique to analyze the right and left ventricular contractility of fetuses with tetralogy of Fallot, indicating significant abnormalities in global contractility, longitudinal contractility, and transverse contractility of the mid and apical segments of the left ventricle in fetuses with tetralogy of Fallot. However, right ventricle contractility demonstrated no significant difference between tetralogy of Fallot and control group for right ventricle global contractility [Citation10], which is similar to our study. Our finding also indicated that CHD had a significant impact on fetal left ventricular morphology.
Previous studies have indicated that normal fetuses exhibit morphological dissimilarities between their left and right ventricles, with the left ventricle showing a more conical shape and the right ventricle exhibiting a morphology more like a bullet. The present study found that in the control group, the SI values of segments 18–24 of the left ventricle were significantly smaller than the values of the right ventricle; in other words, there is a statistically significant difference, which aligns with the finding in previous studies [Citation2,Citation3,Citation17]. In contrast, in the case group, there was no statistically significant difference in the 24-segment SI between the fetal left and right ventricles, suggesting that the morphological differences between the left and right ventricles of the fetuses with CHD were no longer evident.
The conventional approach for assessing fetal heart and ventricle morphology is the visual description, which is subjective and qualitative and cannot achieve precise quantification of individual ventricular segments. In contrast, the fetalHQ can measure fetal cardiac GSI and automatically analyze left and right ventricular 24-segment SI using a speckle-tracking technique. This advanced technology facilitates a comprehensive evaluation of overall cardiac morphology and ventricular geometry. Increasing studies have demonstrated the potential of fetalHQ in evaluating fetal cardiac morphology and functional alterations in pregnant women with anemia, gestational hypertension, gestational diabetes, premature closure of the ductus arteriosus and intrauterine growth restriction [Citation17–24].
Research on the application of fetalHQ to evaluate cardiac morphology and function in fetuses with CHD is scarce. This study sought to address this gap and assessed the global cardiac morphology and geometric morphology of the left and right ventricles in CHD-affected fetuses by fetalHQ. The results revealed that fetal CHD has no significant impact on the global cardiac morphology and right ventricle morphology but has a significant effect on the left ventricle morphology. The study revealed a significant increase in the SI values of basal segments 1–2, indicating a more bullet-shaped ventricular cavity in these segments. Normal fetuses exhibit morphological distinctions between the left and right ventricles, with the former exhibiting conical shapes and the latter showing bullet-like morphologies. The research findings suggested that such differences in fetuses with CHD are not evident.
Although this study achieved fruitful results, it has limitations. Specifically, it is a single-center investigation with a limited sample size. The results of this study indicate that fetal CHD does not exert a significant influence on the general shape of the heart and the right ventricle morphology. Further research is necessary to corroborate these findings, and a larger sample size is required. We did not to use other methods to evaluate the cardiac function of CHD fetuses and compare it with fetalHQ. With fetalHQ, various parameters can be evaluated, including cardiac GSI, ventricular 24-segment SI, ventricular end-diastolic diameter and volume, ventricular area, and ventricular fractional area change. However, this study solely focuses on the alterations in fetal heart GSI and left and right ventricular 24-segment SI.
Conclusions
The fetalHQ presents a straightforward and dependable approach for assessing the cardiac GSI and 24-segment SI of the left and right ventricles in fetuses diagnosed with CHD. While CHD may not significantly impact the overall shape of the fetal heart or the geometric shape of the right ventricle, in this research, there is a notable increase in SI values for the left ventricular segments 1–2, indicating a higher degree of interventricular septal flattening. Additionally, in the presence of CHD, the morphological distinctions between the left and right ventricles in fetuses are no longer discernible.
Disclosure statement
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability statement
The data are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Bravo-Valenzuela NJ, Peixoto AB, Carrilho MC, et al. Fetal cardiac function by three-dimensional ultrasound using 4D-STIC and VOCAL - an update. J Ultrason. 2019;19(79):287–294.
- Luo Y, Xiao F, Long C, et al. Evaluation of the sphericity index of the fetal heart during Middle and late pregnancy using fetalHQ. J Matern Fetal Neonatal Med. 2022;35(25):8006–8011. doi:10.1080/14767058.2021.1940934.
- DeVore GR, Klas B, Satou G, et al. 24-segment sphericity index: a new technique to evaluate fetal cardiac diastolic shape. Ultrasound Obstet Gynecol. 2018;51(5):650–658. doi:10.1002/uog.17505.
- Izumo M, Lancellotti P, Suzuki K, et al. Three-dimensional echocardiographic assessments of exercise-induced changes in left ventricular shape and dyssynchrony in patients with dynamic functional mitral regurgitation. Eur J Echocardiogr. 2009;10(8):961–967. doi:10.1093/ejechocard/jep114.
- Cotran RS, Collins T, Schoen FJ, editors. Robbins pathologic basis of disease. Philadelphia (PA): W.B. Saunders; 1999.
- Vasciaveo L, Zanzarelli E, D'Antonio F. Fetal cardiac function evaluation: a review. J Clin Ultrasound. 2023;51(2):215–224. doi:10.1002/jcu.23421.
- DeVore GR, Satou G, Sklansky M, et al. Speckle tracking analysis in fetuses with D-Transposition: predicting the need for urgent neonatal balloon atrial septostomy. Pediatr Cardiol. 2023;44(6):1382–1396. doi:10.1007/s00246-023-03131-y.
- DeVore GR, Satou G, Sklansky M, et al. Speckle tracking analysis to evaluate the size, shape, and function of the atrial chambers in fetuses with d-transposition of the great arteries to predict the need for neonatal urgent balloon atrial septostomy. Echocardiography. 2023;40(3):204–216. doi:10.1111/echo.15533.
- DeVore GR, Cuneo B, Sklansky M, et al. Abnormalities of the width of the four-chamber view and the area, length, and width of the ventricles to identify fetuses at High-Risk for D-Transposition of the great arteries and tetralogy of fallot. J Ultrasound Med. 2023;42(3):637–646. doi:10.1002/jum.16060.
- DeVore GR, Afshar Y, Harake D, et al. Speckle-Tracking analysis in fetuses with tetralogy of fallot: evaluation of right and left ventricular contractility and left ventricular function. J Ultrasound Med. 2022;41(12):2955–2964. doi:10.1002/jum.15987.
- DeVore GR, Satou GM, Afshar Y, et al. Evaluation of fetal cardiac size and shape: a new screening tool to identify fetuses at risk for tetralogy of fallot. J Ultrasound Med. 2021;40(12):2537–2548. doi:10.1002/jum.15639.
- DeVore GR, Haxel C, Satou G, et al. Improved detection of coarctation of the aorta using speckle-tracking analysis of fetal heart on last examination prior to delivery. Ultrasound Obstet Gynecol. 2021;57(2):282–291. doi:10.1002/uog.21989.
- DeVore GR, Jone PN, Satou G, et al. Aortic coarctation: a comprehensive analysis of shape, size, and contractility of the fetal heart. Fetal Diagn Ther. 2020;47(5):429–439. doi:10.1159/000500022.
- DeVore GR, Portella PP, Andrade EH, et al. Cardiac measurements of size and shape in fetuses with absent or reversed end-diastolic velocity of the umbilical artery and perinatal survival and severe growth restriction before 34 weeks’ gestation. J Ultrasound Med. 2021;40(8):1543–1554. doi:10.1002/jum.15532.
- DeVore GR, Klas B, Satou G, et al. Measuring the area of the interventricular septum in the 4-chamber view: a new technique to evaluate the fetus at risk for septal hypertrophy. J Ultrasound Med. 2022;41(12):2939–2953. doi:10.1002/jum.15980.
- DeVore GR, Satou G, Sklansky M. Abnormal fetal findings associated with a global sphericity index of the 4-chamber view below the 5th centile. J Ultrasound Med. 2017;36(11):2309–2318. doi:10.1002/jum.14261.
- Tan F, Yang J, Shen Y, et al. Evaluating fetal heart morphology in hypertensive disorders of pregnancy using the fetal heart quantitative technique. Transl Pediatr. 2022;11(11):1804–1812. doi:10.21037/tp-22-492.
- Shen Y, Tan F, Yang J, et al. A preliminary study on fetal cardiac morphology and systolic function of normal and anemic pregnant women by fetal heart quantification technology. Transl Pediatr. 2022;11(8):1336–1345. doi:10.21037/tp-22-315.
- Wang D, Liu C, Liu X, et al. Evaluation of prenatal changes in fetal cardiac morphology and function in maternal diabetes mellitus using a novel fetal speckle-tracking analysis: a prospective cohort study. Cardiovasc Ultrasound. 2021;19(1):25. doi:10.1186/s12947-021-00256-z.
- Zhao L, Wu P, Jiao X, et al. Characteristics and outcomes of fetal ventricular aneurysm and diverticulum: combining the use of a new technique, fetal HQ. Front Pediatr. 2023;11:1165972. doi:10.3389/fped.2023.1165972.
- DeVore GR, Zaretsky M, Gumina DL, et al. Right and left ventricular 24-segment sphericity index is abnormal in small-for-gestational-age fetuses. Ultrasound Obstet Gynecol. 2018;52(2):243–249. doi:10.1002/uog.18820.
- Ma J, Cao H, Hong L, et al. Cardiac function assessment in fetuses with ductus arteriosus constriction: a two-Dimensional echocardiography and FetalHQ study. Front Cardiovasc Med. 2022;9:868675. doi:10.3389/fcvm.2022.868675.
- Gireadă R, Socolov D, Mihălceanu E, et al. Evaluation of fetal cardiac geometry and contractility in gestational diabetes mellitus by two-Dimensional speckle-tracking technology. Diagnostics. 2022;12(9):2053. doi:10.3390/diagnostics12092053.
- Li T, Han J, Han Y, et al. Evaluation of changes of cardiac morphology and function in fetuses with ductus arteriosus constriction by speckle-tracking echocardiography. Front Pediatr. 2023;11:1085352. doi:10.3389/fped.2023.1085352.