Abstract
Objective
Elective induction of labor versus expectant management at 39 weeks gestation in low-risk nulliparous patients was shown in the ARRIVE randomized trial of over 6000 patients to decrease risks of cesarean delivery without significant change in the composite perinatal outcome. We aimed to pragmatically analyze the effect of offering elective induction of labor (eIOL) to all low-risk patients.
Methods
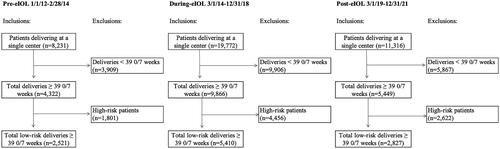
Retrospective cohort study of low-risk nulliparous and multiparous patients delivering live, non-anomalous singletons at a single center at greater than or equal to 39 0/7 weeks gestational age. Those with prior or planned cesarean delivery, ruptured membranes, medical comorbidities, or contraindications to vaginal delivery were excluded. Patients were categorized as before (pre-eIOL; 1/2012–3/2014) or after (post-eIOL; 3/2019–12/2021) an institution-wide policy offering eIOL at 39 0/7 weeks. Births occurring April 2014 to December 2018 were allocated to a separate cohort (during-eIOL) given increased exposure to eIOL as our center recruited participants for the ARRIVE trial. The primary outcome was cesarean birth. Secondary outcomes included select maternal (e.g. chorioamnionitis, operative delivery, postpartum hemorrhage) and neonatal morbidities (e.g. birthweight, small- and large-for gestational age, hypoglycemia). Characteristics and outcomes were compared between the pre and during-eIOL, and pre and post-eIOL groups; adjusted OR (95% CI) were calculated using multivariable regression. Subgroup analysis by parity was planned.
Results
Of 10,758 patients analyzed, 2521 (23.4%) were pre-eIOL, 5410 (50.3%) during-eIOL, and 2827 (26.3%) post-eIOL. Groups differed with respect to labor type, age, race/ethnicity, marital and payor status, and gestational age at care entry. Post-eIOL was associated with lower odds of cesarean compared to pre-eIOL (aOR 0.83 [95% CI 0.72–0.96]), which was even lower among those specifically undergoing labor induction (aOR 0.58 [0.48–0.70]. During-eIOL was also associated with lower odds of cesarean compared to pre-eIOL (aOR 0.79 [0.69–0.90]). Both during and post-eIOL groups were associated with higher odds of chorioamnionitis, operative delivery, and hemorrhage compared to pre-eIOL. However, only among post-eIOL were there fewer neonates weighing ≥4000 g, large-for-gestational age infants, and neonatal hypoglycemia compared to pre-IOL.
Conclusion
An institutional policy offering eIOL at 39 0/7 to low-risk patients was associated with a lower cesarean birth rate, lower birthweights and lower neonatal hypoglycemia, and an increased risk of chorioamnionitis and hemorrhage.
Introduction
The turn of the twenty-first century saw a steady increase in rates of primary cesarean deliveries, with nearly one-third of all deliveries in the United States occurring via cesarean section in 2021 [Citation1,Citation2]. While cesarean deliveries are performed frequently as a routine part of obstetric practice, they are not a benign procedure, with risk of maternal mortality attributable to cesarean mode of delivery as high as 2 per 100,000, as opposed to 0.2 per 100,000 maternal deaths attributable to the vaginal mode of delivery [Citation3]. Efforts toward reducing the rate of cesarean are paramount, with much recent attention being turned to the role of elective induction on subsequent mode of delivery, often with historically conflicting results [Citation4–10].
With elective induction rates as high as one in four United States deliveries in 2019 [Citation11], other potential maternal and fetal effects of elective induction of labor are being increasingly explored. A recent Maternal-Fetal Medicine Unit Network randomized controlled trial including 6106 patients demonstrated that elective induction of labor among low-risk nulliparas decreased cesarean deliveries, with 1 cesarean delivery avoided for every 28 elective labor inductions. Additionally, while there was no significant difference seen in a perinatal composite outcome, induction was associated with shortened length of stay on the labor and delivery and postpartum units, allowed patients greater perceived control during childbirth, reduced pain scores, and reduced rates of hypertensive disorders of pregnancy [Citation5]. Furthermore, retrospective data from our own institution found improved perinatal outcomes among multiparous women undergoing elective induction of labor [Citation12]. As a result of these findings, our department implemented an institution-wide policy offering elective induction of labor to all low-risk patients. Acknowledging that findings from rigorous clinical trials are not always replicated in non-trial settings, we aim to compare outcomes of low-risk pregnant patients before and after implementation of an institution-wide policy universally offering elective induction of labor at 39 weeks gestation.
Materials and methods
We conducted a retrospective cohort study of all low-risk nulliparas and multiparas delivering at greater than or equal to 39 weeks’ estimated gestational age (GA) at a single center from January 2012 to December 2021. Our institution is a large academic, tertiary-care referral center which provides obstetric and gynecologic care to over 7500 patients/year, including approximately 4000 deliveries per year. Institutional Review Board approval (#300001415) was obtained in May 2022 prior to the study initiation. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cohort studies were followed.
Patients who delivered a viable, singleton pregnancy at greater than or equal to 39 0/7 weeks during the study time period were included. Included patients were considered to be “low-risk” for adverse pregnancy outcomes and did not otherwise have a medical or fetal indication for induction prior to 39 weeks. Patients were considered to be “high-risk” for adverse pregnancy outcomes or had an indication for delivery prior to 39 weeks, and therefore excluded if they had any one of the following criteria: ruptured membranes, labor, or fetal demise prior to 39 weeks; fetal growth restriction, defined as an ultrasound estimate of fetal weight <10th percentile, diagnosed prior to 39 weeks; cervical cerclage placement in the current pregnancy; known major congenital anomaly; known or suspected underlying genetic syndrome or aneuploidy; maternal medical comorbidity, including HIV infection, chronic hypertension, gestational or pregestational diabetes mellitus, systemic lupus erythematosus, chronic renal disease, or cardiac disease. Additionally, patients with a history of a prior cesarean delivery, planned primary cesarean (due to suspected macrosomia, history of shoulder dystocia, malpresentation, etc), planned repeat cesarean, prior myomectomy, or placental contraindications to vaginal delivery, e.g. vasa previa, placenta previa, or placenta accreta spectrum, were also excluded.
Our institution’s electronic medical record system (Cerner IMPACT) contains all information for patient encounters anywhere within the hospital system (e.g. emergency departments, outpatient clinic appointments, inpatient admissions). Patients were identified by delivery date using coded data extraction and screened for exclusion using a combination of billing data and diagnosis codes to determine if the patient met characteristics that would be considered “high-risk.” Baseline maternal characteristics and study outcomes were obtained through validated coded data extraction.
At our institution, a memorandum was enacted among obstetric care providers on 14 January 2019 changing the policy to be effective on 4 February 2019 of offering elective labor induction to well-dated low-risk pregnant patients between 39 0/7 and 6/7 weeks GA. This guideline advised that timing of delivery in patients without ultrasound confirmation of gestational age prior to 21 weeks (suboptimal dating), those with a prior cesarean, or patients with medical/obstetrical/fetal complications should be managed using prior guidelines and were not eligible for elective labor induction. Simultaneously, the number of available scheduled labor induction timeslots was increased at our facility to accommodate the anticipated increase in inductions.
Patients were classified by delivery date in relation to the aforementioned policy offering elective induction at 39 0/7 weeks’ gestation to low-risk patients. Deliveries were categorized into 3 epochs – pre-eIOL, during-eIOL, and post-eIOL. Pre-eIOL occurred 1 January 2012 to 28 February 2014, which was prior to the institutional policy liberalizing use of elective induction and prior to the ARRIVE trial [Citation5], for which our center was a participating site. During-eIOL occurred 1 March 2014 to 31 December 2018 and includes the period of the ARRIVE trial at which our site enrolled patients March 2014 to August 2017. Specifically, patients enrolled in the ARRIVE trial were included in this analysis if otherwise appropriate and meeting inclusion criteria. The during-eIOL time period also has the potential for case or provider-specific early adoption of elective induction following publication of the trial results in August 2018. Post-eIOL occurred 1 March 2019 to 31 December 2021 and follows after the implementation of our policy adopting eIOL in all patients. Births occurring 1 January 2019 through 28 February 2019 were excluded as a washout period during which the institutional policy was initially released. Patients undergoing any labor type (spontaneous, augmented, or induced) were included for analysis in their respective time period.
The primary outcome was cesarean birth. Secondary outcomes included GA at delivery; select maternal morbidities: chorioamnionitis, operative vaginal delivery (OVD), postpartum hemorrhage; maternal death; select fetal and neonatal morbidities: stillbirth diagnosed at 39 0/7 weeks or greater, 5-min APGAR ≤3, neonatal birthweight and birthweight ≥4000 g, small-for-GA (<10th percentile) infant, large-for-GA (>90th percentile) infant, neonatal intensive care unit (NICU) admission, hypoglycemia (<35 mg/dL); neonatal death within 28 days of life.
Maternal demographics, pregnancy characteristics, and primary and secondary outcomes were compared among the study groups using the chi-square test of association for categorical variables, and Kruskal Wallis or One-way ANOVA tests for continuous variables, as appropriate. Characteristics were compared across all three study groups and pairwise tests compared pre-eIOL vs. during-eIOL, and pre vs. post-eIOL groups. For binary outcomes, crude odds ratios (ORs) with 95% confidence intervals (CIs) were estimated using logistic regression with pre-eIOL as the referent group. Multinomial multivariable models across all three time epochs adjusted for potentially confounding factors. Covariates identified as being statistically significantly different between exposure groups in bivariate analyses, had biological plausibility in the specific model, and had low correlations with other factors were included as potential confounders in these multivariable models. Additionally, factors which had low variability and did not allow for model convergence were excluded from the multivariate models as well. Additional analysis by receipt of labor induction and by parity was planned. All primary analyses were performed using SAS 9.4 (Cary, NC) and outcomes were evaluated at a 0.05 level of significance without adjustment for multiple comparisons.
Results
Of 19,849 total deliveries between 2012 and 2021, 10,758 occurred at ≥39 0/7 weeks and met final inclusion criteria (). Of those included for analysis, 2521 (23.4%) were pre-eIOL, 5410 (50.3%) during-eIOL, and 2827 (26.3%) post-eIOL. Groups differed with respect to maternal age and advanced maternal age, with increasing age and higher rate of advanced maternal age in the during-eIOL and post-eIOL groups (). Groups also differed by race and ethnicity, with lowest rate of Black patients and highest rate of Hispanic ethnicity in post-eIOL cohort. The post-eIOL group also had the highest rate of married and privately insured patients, as well as the earliest intake GA into prenatal care, compared to the earlier cohorts. Lastly, patients in the post-eIOL had the highest rate of labor induction (64.1%) compared to the pre-eIOL (36.2%) and the during-eIOL (40.9%), as anticipated by the changes in the protocol offering elective induction. Similarly, post-eIOL had lower rates of spontaneous (9.8%) and augmented (26.1%) labor relative to the pre-eIOL (19.2% and 44.6%) and during-eIOL (18.5% and 40.6%) cohorts, respectively ().
Table 1. Demographics of low-risk pregnant patients before and after adoption of institution-wide policy offering elective induction at ≥39 0/7 weeks.
The primary outcome of cesarean birth occurred in 15.3% of the post-eIOL patients and 17.5% of pre-eIOL patients, corresponding to decreased odds of cesarean delivery (OR 0.85 [0.74-0.99]). The odds of cesarean delivery remained lower among the post-eIOL group after adjustment (aOR 0.83 [95% CI 0.72–0.96], ). The model included covariates of maternal age, marital status, and GA of intake into prenatal care. Insurance status was highly correlated with marital status and was therefore not included in the multivariable model. Race/ethnicity was not included in the multivariable models as this variable does not have biologic plausibility. Labor type (spontaneous, augmented, induced) was also excluded from the adjusted model as this covariable occurred along the causal pathway of the exposure and outcome relationship, i.e. the policy change across time epochs directly altered labor type.
Table 2. Primary and secondary outcomes among low-risk pregnant patients before and after adoption of institution-wide policy offering elective induction at ≥39 0/7 weeks.
With regard to secondary maternal outcomes, post-eIOL was associated with higher odds of chorioamnionitis (aOR 1.61 (1.24–2.10]), OVD (aOR 2.84 (2.03–3.98]), and hemorrhage (aOR 1.73 [1.39–2.15]) compared to pre-eIOL (). This remained true of the during-eIOL group compared to the pre-eIOL group as well. There were no maternal deaths in any of the three cohorts (data not shown).
With regard to secondary neonatal outcomes, GA of delivery differed across the 3 time periods (p < 0.001); during-eIOL and post-eIOL were associated with a higher odds of delivery <40 weeks GA and a lower odds of postterm delivery compared to the pre-eIOL group (). Post-eIOL was associated with lower odds of several neonatal morbidities including birthweight ≥4000 g (aOR 0.56 [0.45–0.70]), large-for-GA infants (aOR 0.66 [0.52–0.85]), and neonatal hypoglycemia (aOR 0.44 [0.24–0.81]). However, there was no difference in birthweights ≥4000 g, large-for-GA infants, and hypoglycemia when evaluating the during-eIOL cohort compared to pre-IOL There was also no difference with respect to stillbirth, 5-min APGAR ≤3, or NICU admission (). No neonatal deaths occurred in any of the three groups (data not shown).
In sensitivity analysis including only patients who actually underwent labor induction (i.e. excluding those patients who had spontaneous or augmented labor), results were overall consistent with the primary analysis. The rate of cesarean birth was significantly lower among patients in the post-eIOL group compared to pre-eIOL (18.3% vs 27.7%, aOR 0.58 [0.48–0.70], ). This was also seen in the during-eIOL group compared to pre-eIOL (21.0% vs 27.7%, aOR 0.68 [0.57–0.82]). In contrast to the primary analysis of all patients, there was no difference in the rate of chorioamnionitis among induced patients in the post-eIOL compared to pre-eIOL group. There remained a significant increase in OVD and hemorrhage in the post-eIOL group. Similarly, the improvement of neonatal outcomes persisted among the induced patients, with lower rate of birthweights ≥4000 g, large-for-GA infants, and hypoglycemia among the post-eIOL group ().
Table 3. Primary and secondary outcomes among low-risk patients undergoing labor induction before and after adoption of institution-wide policy offering elective induction at ≥39 0/7 weeks.
When evaluating only nulliparas, outcomes were again overall consistent with the primary analysis. Cesarean birth was significantly reduced among patients in the post-eIOL group compared to pre-eIOL (25.5% vs 29.6%, aOR 0.74 [0.62–0.88], Supplemental Table 1). This was also seen in the during-eIOL group compared to pre-eIOL (24.3% vs 29.6%, aOR 0.71 [0.62–83]). Rates of chorioamnionitis, OVD, and hemorrhage were higher in the post-eIOL compared to pre-eIOL group. However, neonatal benefits remained in the post-eIOL compared to pre-eIOL, with lower rates of birthweights ≥4000 g and large-for-GA infants, and no difference in stillbirth, 5-min APGAR ≤3, small-for-GA infants, NICU admission, or hypoglycemia (Supplemental Table 1).
Lastly, in subgroup analysis of multiparous patients, cesarean birth was lower but was not significantly reduced among patients in the post-eIOL group compared to pre-eIOL (6.1% vs 6.9%, aOR 0.83 [0.70–1.18], Supplemental Table 2). As anticipated, there was no difference in rate of cesarean birth in the during-eIOL group compared to pre-eIOL (6.6% vs 6.9%, aOR 0.91 [0.70–1.18]), as multiparas were not candidates for inclusion in the ARRIVE trial. Rates of OVD and hemorrhage were higher in the post-eIOL compared to pre-eIOL group, however there was no change in rate of chorioamnionitis. There was a higher incidence of 5-min APGAR ≤3 in the post-eIOL group compared to pre-eIOL (aOR 2.83 [1.11–7.24]) though there was no difference in NICU admission. Lastly, the neonatal benefits seen with lower rates of birthweights ≥4000 g, large-for-GA infants, and neonatal hypoglycemia remained in the post-eIOL compared to pre-eIOL (Supplemental Table 2), and was consistent with the primary analysis.
Discussion
In this retrospective cohort study of low-risk patients delivering at ≥39 weeks and at a single tertiary-care center from 2012 to 2021, those who delivered following institutional policy offering elective induction in the 39th week had lower odds of cesarean delivery than those delivering prior to the institutional change. This benefit of decreased cesarean birth rate was also seen among patients who accepted and underwent labor induction. Additionally, patients who delivered in the timeframe offering elective induction realized improved neonatal outcomes, including fewer neonates weights ≥4000 g, large-for-GA infants, and hypoglycemia compared to prior to the institutional protocol with no change in stillbirth or NICU admission; these neonatal benefits were seen among all sensitivity and subgroup analyses, including those undergoing labor induction as well as nulliparas and multiparas. However, the post-eIOL group had higher rates of chorioamnionitis, operative delivery, and hemorrhage compared to pre-eIOL.
In light of the results of the ARRIVE trial, the American College of Obstetricians and Gynecologists’ (ACOG) recently reaffirmed Practice Advisory has deemed it appropriate to offer elective induction to low-risk nulliparous patients [Citation13]. Our findings in a real-world setting note a high rate of labor induction uptake, occurring in more than 60% of the post-eIOL group, as well as confirm the results of the ARRIVE trial noting lower cesarean rates with post-eIOL. While the ARRIVE population noted a rate of cesarean of 18.6% in the eIOL group compared to 22.2% in the expectant management group (relative risk (RR) 0.84, 95% CI 0.76–0.93) [Citation5], our cohort of all patients noted a 15.3% rate of cesarean post-eIOL compared to 17.5% pre-eIOL (aOR 0.83 [0.72–0.96]); this held true in our induction sensitivity analysis (18.3 vs 27.7%, aOR 0.58 [0.48–0.70]) as well as nulliparous subgroup analysis (25.5 vs 29.6%, aOR 0.74 [0.62–0.88]). Additionally, while the ARRIVE trial noted a trend toward improvement in a neonatal composite among those undergoing eIOL although this was not statistically significant (RR 0.8, 95% CI 0.64–1.00) [Citation5], our study noted improvement in several neonatal morbidities including birthweight, large-for-GA infants, and neonatal hypoglycemia. These benefits were seen in those undergoing labor induction as well as in both parity subgroup analyses. While our data are retrospective rather than prospective and randomized, these infant benefits are certainly promising and support institutional policies in favor of elective induction to all comers.
Though ACOG’s organizational approval of elective labor induction has not yet been extended to multiparous patients [Citation13], the results of our study and previous studies [Citation9] suggest several benefits of labor induction in multiparas. Although not statistically significant, the rate of cesarean birth was lower in the post-eIOL compared to pre-IOL (aOR 0.83 [0.70–1.18]). There were no differences in rate of chorioamnionitis or hemorrhage among multiparas in the pre- vs post-eIOL groups. Additionally, the post-eIOL cohort saw notable improvements in neonatal outcomes including birthweight (all birthweights within normal range), birthweights ≥4000 g, large-for-GA infants, and neonatal hypoglycemia with no difference in stillbirth or NICU admission. Overall, our analysis suggests numerous benefits of elective induction in multiparas without an increase in adverse outcomes, paving the way for a future broadening of the current guidelines and a continued shift in practice management for patients who desire elective induction. While the reasons behind the consistent stable cesarean rate and improvement in neonatal outcomes remain unclear, it may be attributable at least in part to the decreased rate of cephalopelvic disproportion and reflected by this study’s finding of a reduced neonatal birthweight, weight ≥4000 g and rate of large-for-GA. We did find an approximately 2-fold increase in the incidence of OVD in the post-eIOL group compared to pre-eIOL group and this was seen in all subgroup analysis. We anticipate this increase in OVD to have contributed to the successful decrease in cesarean rates and is overall considered a safe option for delivery in appropriate candidates. However, we acknowledge that changes in the rate of OVD may be impacted by factors such as fluctuation in training culture and practice patterns among different providers, which may be independent from the changes made to labor induction protocols.
Interestingly, our study found an increased incidence of chorioamnionitis and hemorrhage in the post-eIOL compared to the pre-IOL group. Chorioamnionitis however was not increased among the induction-only sensitivity analysis of post-eIOL compared to pre-eIOL, while postpartum hemorrhage was increased in that analysis. Though less expected findings, this may be tied to a potentially lengthier labor course anticipated with induction rather that spontaneous labor, although duration of labor induction or time spent on Labor and Delivery are not included in our database. The increase in postpartum hemorrhage may be due in part to increased awareness of bleeding at time of delivery, as well as institution of a “hemorrhage protocol” bundle on Labor and Delivery in the post-eIOL timepoint which included denoting a hemorrhage based on a laparotomy sponge count of >30 during a cesarean regardless of the surgeon estimated blood loss. This should be evaluated in other centers. An elevated chorioamnionitis rate was also found in a prospective randomized controlled trial conducted by our group investigating the utility of inpatient versus outpatient cervical ripening in pregnant individuals undergoing induction [Citation14]. In this study, those undergoing inpatient ripening had a 13% rate of chorioamnionitis. Though these findings have not been consistently demonstrated in other studies exploring the effects of 39-week elective induction [Citation15,Citation16], this warrants further investigation and highlights the importance of ongoing studies that can accurately predict spontaneous labor [Citation17].
There are multiple strengths of our study. We utilized a large cohort of nearly 11,000 patients which was diverse in terms of race/ethnicity, payor status, and marital status, making our results applicable to other populations across the country. Adjustment for select baseline maternal and pregnancy characteristics reduced the risk of confounding inherent to all observational studies. Additionally, we were able to perform additional analyses by labor type and parity, adding to the robustness of our study.
Limitations of our project include the retrospective nature of the data ascertainment and its associated confounding and bias. As our data were obtained through coded electronic extraction as opposed to detailed chart review, there is the possibility of misclassification of patient characteristics and outcomes. We lacked data on the indication for cesarean delivery, which could help inform potential reasons why a policy promoting labor induction could be associated with a reduced rate of cesarean. We also lacked data on specific labor induction or augmentation method (e.g. foley catheter, misoprostol, pitocin) and labor duration, which may impact certain outcome measures such as cesarean, infection and hemorrhage. Some patients in the during-eIOL and post-eIOL group had a labor induction for indications other than elective purposes, e.g. non-reassuring antenatal testing, hypertensive disorder, etc. However, as this was a pragmatic analysis, the post-protocol group did experience a reduction in cesarean deliveries. From a hospital management standpoint, this supports the findings of the ARRIVE trial with respect to the lower cesarean rate among elective inductions in a real-word application and among both patients being induced and nulliparas. As our analysis was conducted at a single center, it may not be generalizable to all practice settings. Lastly, given this analysis compares a recent cohort to a historical cohort, there may have been other confounding factors which could have contributed to this result; specifically, changes to management of labor, namely the 2014 care consensus revising guidelines for safe prevention of primary cesarean birth [Citation1], may have impacted our analysis and resulted in a lower rate of cesarean over time.
In this retrospective cohort study of low-risk patients delivering at a single tertiary-care center from 2012 to 2021, those who delivered following institutional policy offering elective induction at 39 weeks had a lower odds of cesarean delivery than those delivering prior to this institutional change. This was consistent in those undergoing labor induction and in nulliparas. Additionally, we saw improvements in several neonatal outcomes likely attributed to decreases in birthweight and large-for-GA status. While future studies should investigate the impact on rates of chorioamnionitis and hemorrhage, future studies should also continue to evaluate ways to decrease labor induction length among low-risk patients desiring elective induction of labor.
Supplemental Material
Download MS Word (21.5 KB)Acknowledgements
None.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data available on request from the authors.
Additional information
Funding
References
- American College of O, Gynecologists, Society for Maternal-Fetal M., et al. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Osterman MJK, Hamilton BE, Martin JA, et al. Births: final data for 2021. Natl Vital Stat Rep. 2023 ;72(1):1–53.
- Clark SL, Belfort MA, Dildy GA, et al. Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. Am J Obstet Gynecol. 2008;199(1):36 e1-5–36.e5. discussion 91-2e7-11. doi: 10.1016/j.ajog.2008.03.007.
- Ehrenthal DB, Hoffman MK, Jiang X, et al. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011;118(5):1047–1055. doi: 10.1097/AOG.0b013e3182319c58.
- Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379(6):513–523. doi: 10.1056/NEJMoa1800566.
- Luthy DA, Malmgren JA, Zingheim RW. Cesarean delivery after elective induction in nulliparous women: the physician effect. Am J Obstet Gynecol. 2004;191(5):1511–1515. doi: 10.1016/j.ajog.2004.07.001.
- Maslow AS, Sweeny AL. Elective induction of labor as a risk factor for cesarean delivery among low-risk women at term. Obstet Gynecol. 2000;95(6 Pt 1):917–922. doi: 10.1097/00006250-200006000-00026.
- Seyb ST, Berka RJ, Socol ML, et al. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol. 1999;94(4):600–607. doi: 10.1097/00006250-199910000-00022.
- Sinkey RG, Blanchard CT, Szychowski JM, et al. Elective induction of labor in the 39th week of gestation compared with expectant management of low-risk multiparous women. Obstet Gynecol. 2019 Aug;134(2):282–287. doi: 10.1097/AOG.0000000000003371.
- Sinkey RG, Lacevic J, Reljic T, et al. Elective induction of labor at 39 weeks among nulliparous women: the impact on maternal and neonatal risk. PLOS One. 2018;13(4):e0193169. doi: 10.1371/journal.pone.0193169.
- Marconi AM. Recent advances in the induction of labor. F1000Res. 2019;8:1829. doi: 10.12688/f1000research.17587.1.
- Elective induction of labor in the 39th week of gestation compared with expectant management of low-risk multiparous women: correction. Obstet Gynecol. 2019;134(4):884
- Bulletins ACoOaGCoOPaCoP. Clinical Guidance for Integration of the Findings of The ARRIVE Trial: labor Induction Versus Expectant Management in Low-Risk Nulliparous Women. 2018.
- Ausbeck EB, Jauk VC, Xue Y, et al. Outpatient foley catheter for induction of labor in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2020;136(3):597–606. doi: 10.1097/AOG.0000000000004041.
- El-Sayed YY, Rice MM, Grobman WA, et al. Elective labor induction at 39 weeks of gestation compared with expectant management: factors associated with adverse outcomes in low-risk nulliparous women. Obstet Gynecol. 2020;136(4):692–697. doi: 10.1097/AOG.0000000000004055.
- Sotiriadis A, Petousis S, Thilaganathan B, et al. Maternal and perinatal outcomes after elective induction of labor at 39 weeks in uncomplicated singleton pregnancy: a meta-analysis. Ultrasound Obstet Gynecol. 2019;53(1):26–35. doi: 10.1002/uog.20140.
- Sanusi A, Ye Y, Battarbee AN, et al. Predicting spontaneous labor beyond 39 weeks among low-risk expectantly managed pregnant patients. Am J Perinatol. 2023;40(16):1725–1731. doi: 10.1055/a-2099-4395.