Abstract
Objective
We examined whether the chest-to-head circumference ratio at birth was associated with breech presentation and transverse lie. We also described the obstetric management of such pregnancies in the Japan Environment and Children’s Study (JECS).
Methods
We performed a cross-sectional evaluation of data collected between January 2011 and March 2014 in a nationwide prospective birth cohort study, the JECS. We analyzed 83,822 non-anomalous singletons born at 34–41 weeks’ gestation to mothers with no history of previous cesareans or uterine surgery. We defined low, normal (reference group), and high chest-to-head circumference ratios as <10th percentile, 10th to 90th percentiles, and >90th percentile, respectively. Logistic regression models were used to estimate odds ratios (ORs) and 95% confidence intervals (95% CIs) for breech presentation and transverse lie. The timing and mode of delivery of such pregnancies were examined.
Results
Breech presentation was recorded in 2.6% and transverse lie in 0.2%. A low chest-to-head circumference ratio was associated with increased rate of breech presentation (5.2%; adjusted OR 2.36, 95% CI: 2.10–2.65) and transverse lie (0.3%; adjusted OR 2.33, 95% CI: 1.50–3.60), whereas a high ratio was linked to reduced breech presentation (1.1%; adjusted OR 0.51, 95% CI: 0.39–0.66). Subgroup analysis of children delivered by cesarean (n = 7971) showed a similar association, albeit with slightly reduced strength for breech presentation. Eighty-three percent of breech births and 46.3% of transverse lie births occurred at 37–38 weeks’ gestation. Cesarean section was performed in 96.8% of breech presentations and 63.4% of transverse-lie ones.
Conclusions
These findings imply that the fetal chest-to-head circumference ratio may influence presentation at birth.
Introduction
The birth of a breech fetus requires extra considerations for both the mothers and clinicians; clinical practice guidelines have therefore been published by several leading obstetric organizations [Citation1–4]. These guidelines suggest that clinicians offer an external cephalic version to every woman carrying a term singleton breech fetus to reduce the rate of breech presentation at birth. If the offer is declined or the attempt has failed, in the presence of experienced clinicians and under hospital-specific criteria (including informed consent and eligibility), a planned vaginal breech birth can be an alternative to an elective cesarean. However, some breech pregnancies are discovered only in labor [Citation5]. Moreover, recent studies suggest that the number of clinicians with expertise in vaginal breech birth has been decreasing [Citation6–8]. Therefore, among near-term babies, it is essential to identify those with the potential for non-cephalic presentation to avoid the maternal and neonatal risks associated with complicated vaginal breech birth or emergency cesarean.
In a study of 45,847 singleton pregnancies, the incidence of non-cephalic presentation at 35–36 week’s ultrasonography was 5.3% (n = 2431); spontaneous cephalic version occurred in 30.4% (n = 738) of these cases before birth [Citation9]. The corresponding figure for spontaneous cephalic version in a recent Japanese study was 25.8% [Citation10]. However, in practice, clinicians do not know whether or not this spontaneous rotation to cephalic presentation will occur. Many suggest that fetuses with suboptimal growth have a reduced chance of turning to a cephalic presentation [Citation11–14]. Fetal growth is commonly determined in utero or at birth using anthropometric measurements such as weight, length, body circumferences, or their ratios [Citation15]. Our recent study suggests that newborns with chest-to-head circumference ratio at the lower extreme may have experienced pathologic growth restriction in utero [Citation16]. We considered that the chest-to-head circumference ratio might have a role in determining fetal presentation at birth. Therefore, our aims were to examine whether the chest-to-head circumference ratio at birth is associated with breech presentation and transverse lie; and to describe the obstetric management of such pregnancies in the Japan Environment and Children’s Study (JECS). We hypothesized that non-cephalic presentation would increase as the ratio decreased.
Materials and methods
This cross-sectional study is a secondary analysis of data from JECS, which recruited pregnant women throughout Japan between January 2011 and March 2014. The JECS protocol was approved by the Institutional Review Board on Epidemiological Studies of the Ministry of the Environment (no. 100910001) and the Ethics Committees of all participating institutions. Written informed consent was obtained from all participants. Detailed maternal, newborn, and pregnancy-related information was collected through standardized questionnaires (distributed during the first trimester and the second or third trimester) or from medical records (retrieved during the first trimester and at birth). The detailed protocol and the baseline information of participants have been reported previously [Citation17,Citation18].
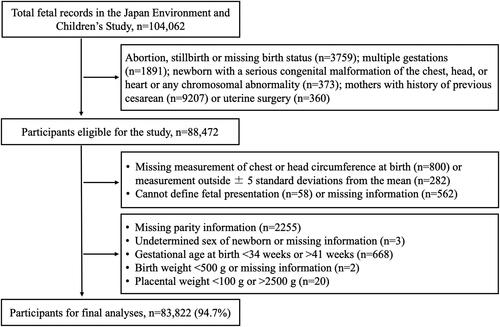
Our study was restricted to non-anomalous live-birth singleton pregnancies without maternal history of previous cesareans or uterine surgery. Of the 88,472 eligible pregnancies, we excluded those that were missing measurements of the chest or head circumference and those with values above or below five standard deviations (SDs) from the means (i.e. outliers); we also excluded those for whom we could not define fetal presentation, or this information was missing. Also excluded were records with missing parity information or newborn sex, the child’s gestational age at birth was <34 weeks or >41 weeks, missing birth weight data or <500 g, and those with placental weight <100 g or >2500 g ().
Measurements of the chest and head circumferences at birth were transcribed from medical records. These measurements are routinely performed on newborns within 24 h of birth by a midwife, following standard methods. Head circumference is measured along the line passing the glabella and the external occipital protuberance. Chest circumference is measured mid-respiration on the nipple line, perpendicular to the body axis. Non-stretchable tape is used, and measurements are recorded to the nearest 0.1 cm. The chest-to-head circumference ratio was calculated as (chest circumference (cm)/head circumference (cm)) × 100. We used an internally constructed gestational age-, sex-, and parity-specific reference chart to define a low chest-to-head circumference ratio as <10th percentile and a high ratio as >90th percentile, with the range between these thresholds considered normal [Citation16].
Information on fetal presentation and obstetric management was also transcribed from the medical records. We grouped fetal presentations into head, breech, and transverse lie. The “head” group included all records with a cephalic presentation, whereas “breech” included all types of breech presentation (i.e. frank, complete, and footling). Obstetric management was determined based on the timing (34–36 weeks, 37–38 weeks, 39–40 weeks, or 41 weeks) and mode (spontaneous vaginal, induced, instrumental or cesarean) of the birth. Gestational age at birth was ascertained from the first trimester ultrasonographic measurement, or the last menstrual period.
Maternal and newborn information collected included maternal age, parity, height, pre-pregnancy body mass index (BMI), weight gain during pregnancy, smoking during pregnancy, medical morbidities (anemia, diabetes, or hypertension), receipt of assisted conception, pregnancy complications (oligo- or polyhydramnios, or placenta previa), newborn sex, birth weight, and placental weight. Fetoplacental ratio (a measure of placental efficiency) was calculated as birth weight divided by placental weight. We categorized birth weight by using two criteria, namely as <2500 g, 2500–3800 g, and >3800 g by using absolute birth weight; and as small for gestational age (<10th percentile), appropriate for gestational age (10th–90th percentiles), and large for gestational age (>90th percentile) by using the gestational-age-, sex-, and parity-specific birth weight percentile chart for Japanese [Citation19].
Statistical analysis
First, we examined the association of chest-to-head circumference ratio with breech presentation or transverse lie. Maternal and newborn characteristics were compared among chest-to-head circumference ratio groups. We also compared newborn measurements for breech presentation and transverse lie with those for head presentation. The occurrence of pregnancies presenting as breech or transverse lie among the newborn groups was determined, and logistic regression models were used to estimate crude and adjusted odds ratios (ORs) with 95% confidence intervals (95% CIs) for such pregnancies with a low or high chest-to-head circumference ratio, using a normal ratio as the reference. To account for newborns delivered head-first vaginally, often with molded heads that might result in falsely low head circumference estimates (Supplemental Table S1), we conducted an additional analysis by excluding these cases. Considering a priori knowledge and the causal association between chest-to-head circumference ratio and fetal presentation [Citation9,Citation11–14], we controlled for the following factors: maternal age, parity, pre-pregnancy BMI, maternal height, gestational weight gain, tobacco use, anemia, hypertension, diabetes, receipt of assisted conception, oligohydramnios, polyhydramnios, placenta previa, fetoplacental ratio, newborn sex, birth weight, and gestational age. Second, we examined the obstetric management (i.e. the timing and mode of birth) of breech presentation and transverse lie.
We did not attempt to apply statistical methods (e.g. multiple imputation) to evaluate the sensitivity to missing data, because only a small percentage of participants had missing information on covariates (). Descriptive statistics were reported as means ± SD for continuous variables and numbers and percentages (%) for categorical variables. Comparisons among groups were conducted using one-way ANOVA or independent-sample Student’s t-test (for continuous variables) and Pearson’s Chi-square (for categorical variables). A p value of <.05 was considered statistically significant. Statistical analyses were performed by using Stata/MP 17.0 software (StataCorp., College Station, TX).
Table 1. Maternal, neonatal, and pregnancy-related information according to chest-to-head circumference ratio.
Results
Out of 88,472 potentially eligible pregnancies, we excluded 4650 in accordance with predetermined criteria (). Among the 83,822 pregnancies analyzed, 11.3% (n = 9490) had a low chest-to-head circumference ratio at birth, while 7.6% (n = 6351) had a high ratio. Non-cephalic presentation occurred in 2.8% (n = 2306) of pregnancies, including 2.6% (n = 2183) breech presentations and 0.2% (n = 123) transverse lie. presents the maternal, neonatal, and pregnancy-related information for the newborn groups. Compared with those in the normal-ratio group, mothers in the low-ratio group were slightly more likely to be aged 35 or older, have pre-pregnancy BMI <18.5 kg/m2, experience less weight gain during pregnancy, have hypertension, receive assisted conception, and have pregnancies complicated by oligo- or polyhydramnios. Conversely, mothers in the high-ratio group were slightly less likely to have these characteristics compared to the normal-ratio group. The mean gestational age did not differ clinically among the ratio groups. Birth weight and placental weight were lowest in the low-ratio group and highest in the high-ratio group; however, fetoplacental ratios were similar across the groups.
compares the measurements of newborns with breech presentation and transverse lie to those with head presentations. Newborns in the breech group had a smaller chest circumference but larger head circumference, resulting in a lower chest-to-head circumference ratio compared to those with head presentation. They also had a shorter gestation, lower birth weight, placental weight, and fetoplacental ratio. Compared with a normal chest-to-head circumference ratio, breech presentation was higher with a low ratio and lower with a high ratio. Breech presentation was also more frequent in newborns with birth weight <2500 g and less common in those with birth weight >3800 g; however, there were no differences across newborn groups stratified by gestational age-, sex-, and parity-specific birth weight percentile. The measurements of newborns in transverse lie showed lower mean chest circumference, chest-to-head circumference ratio, gestational length, birth weight, and fetoplacental ratio compared to those with head presentation. Transverse lie was more common in the low chest-to-head circumference ratio group and in newborns with birth weight <2500 g compared to the other ratio and birth weight groups.
Table 2. Newborn measurements according to fetal presentation.
presents the association between the chest-to-head circumference ratio and breech presentation as well as transverse lie. A low ratio was associated with an increased likelihood of breech presentation (5.2%; adjusted OR 2.36, 95% CI: 2.10–2.65) and transverse lie (0.3%; adjusted OR 2.33, 95% CI: 1.50–3.60), whereas a high ratio was linked to a reduced likelihood of breech presentation (1.1%; adjusted OR 0.51, 95% CI: 0.39–0.66). Subgroup analysis of children delivered by cesarean (n = 7971) showed a similar association, albeit with a slightly reduced strength for breech presentation (adjusted OR 1.28, 95% CI: 1.09–1.52) ().
Table 3. Occurrence and odds ratio (95% CI) for breech presentation and transverse lie with low or high chest-to-head circumference ratio.
Table 4. Occurrence and odds ratio (95% CI) for breech presentation and transverse lie with low or high chest-to-head circumference ratio.
presents obstetric management according to fetal presentation. The birth of 83% of breech fetuses and 46.3% of transverse lie occurred at 37–38 weeks’ gestation, whereas this occurred in 72.1% of head-presenting fetuses at or after 39 weeks’ gestation. Birth by cesarean section was observed in 96.8% of breech presentations and 63.4% of transverse lie.
Table 5. Obstetric management according to fetal presentation.
Discussion
We analyzed data on 83,822 live-born, non-anomalous singletons without a maternal history of cesareans or uterine surgery. Our analysis revealed that a low chest-to-head circumference ratio at birth was associated with an increased likelihood of breech presentation and transverse lie, whereas a high ratio was associated with a reduced occurrence of these presentations. Controlling for maternal, neonatal, and pregnancy factors did not substantially change these associations.
Our findings suggest that a low chest-to-head circumference ratio likely predisposes a fetus to non-cephalic presentation. Although the mean fetoplacental ratio (a surrogate measure for fetal nutrition adequacy) was similar across the ratio groups, the low-ratio group exhibited the lowest birth weight and placental weight, indicating proportional growth reduction. In our recent study, newborns with a low chest-to-head circumference ratio are at higher risk of adverse obstetric and neonatal outcomes, such as the need for cesarean birth, lower Apgar score, respiratory complications, and prolonged hospitalization [Citation16]. We suggest that newborns in the low-ratio group might have survived despite the chronic undersupply of the oxygen, nutrients, growth factors, and hormones by the small placenta.
Additionally, we observed that the mean head circumference was larger in breech fetuses than in those with head presentation, whereas in transverse lie, it was similar to that in those with head presentation. Head circumference is commonly used as a surrogate measure of brain size. However, brain sparing in placental insufficiency does not ensure normal neurodevelopment [Citation20], and poor fetal neuromuscular development may contribute to non-cephalic presentation [Citation21]. Furthermore, fetal movements, such as sudden extension of the legs and active whole-body movement, favor spontaneous cephalic version [Citation22,Citation23]. We hypothesized that a fetus with a low chest-to-head circumference ratio may be less active and may have reduced capability to turn to a cephalic position. This hypothesis merits further investigation.
Contrary to past reports associating low birth weight with an increased risk of breech presentation [Citation11–14], we found that other factors, including gestational age, likely influenced the association between birth weight and fetal presentation (Supplemental Tables S2 and S3). Moreover, the occurrence of breech or transverse lie was similar across newborn groups stratified by gestational age-, sex-, and parity-specific birth weight percentile.
Our study highlights the variation in clinical practices regarding the timing and mode of birth for breech presentation. In a German survey, most participating hospitals preferred external cephalic version after 37 weeks’ gestation as the primary obstetric management for breech pregnancies [Citation24]. In Ireland, every woman carrying a singleton breech fetus at 37–38 weeks’ gestation is counseled and offered external cephalic version or elective cesarean section at 39 weeks’ gestation [Citation7]. One-third of breech pregnancies in France planned for vaginal birth at term [Citation1]. In contrast, it is common in Japan for singleton breech babies to undergo elective cesarean at 37–38 weeks’ gestation, except in some specialized centers that offer vaginal breech deliveries [Citation25]. In our study, we found that cesarean births occurred in 96.8% of breech pregnancies, whereas the reported rates in Canada, Europe, and the United States range from 65.7% to 97% [Citation26–28]. In our population, 83% of breech births occurred at 37–38 weeks’ gestation, with only 8.6% occurring at or after 39 weeks. In contrast, in a large population-based Belgian study, of the 26,565 breech births that occurred at or after 34 weeks’ gestation, only 52.4% occurred at 37 to 38 weeks [Citation14]; 9.8% of the breech births occurred at 34–36 weeks’ gestation, and 37.8% occurred at or after 39 weeks. The higher week-specific rate of cesarean breech birth in our study may be attributed to the aim of avoiding stillbirth after 39 weeks’ gestation and the limited availability of experienced obstetricians for vaginal breech births in Japan.
While a cesarean birth can be life-saving for both the mother and the child in certain circumferences, the procedure is not without adverse sequelae. These sequelae include complications for the mother, such as puerperal infection, hemorrhage, issues associated with anesthesia or blood transfusion, and venous thromboembolism [Citation29]. Similarly, the child may experience respiratory complications, reduced intestinal microbiome diversity, obesity, and emotional and behavioral problems [Citation29,Citation30]. Subsequent pregnancies may be impacted by complications such as uterine rupture, stillbirth, and abnormal placentation [Citation29]. Additionally, compared to full-term births, those occurring at early term (37+0 to 38+6 gestational weeks) are associated with an increased risk of neonatal respiratory complications, regardless of the mode of birth [Citation31–33], as well as the risk of neurodevelopmental impairments in childhood [Citation34,Citation35], and the risk of death from noncommunicable diseases in later life [Citation36]. Several studies have demonstrated the safety of external cephalic version [Citation26,Citation37] and vaginal breech birth [Citation6,Citation25], especially in an upright birth position [Citation38]. However, the success and safety of these procedures are largely dependent on the experience and skill of the providers. The practice of vaginal breech birth has been decreasing, and obstetricians have limited opportunities for training [Citation6–8]. To promote external cephalic version and vaginal breech birth as alternative to elective cesareans, the obstetric community should encourage the establishment of specialized obstetric teams or centers dedicated to breech birth.
This cross-sectional study found that newborn chest-to-head circumference ratio <10th percentile was associated with an increased likelihood of breech presentation and transverse lie, whereas a ratio >90th percentile was associated with reduced occurrence of these presentations. Giving the stabilization of fetal presentation [Citation10] and the fact that most fetuses presenting as breech at birth have already done so by the 32nd week of pregnancy [Citation39], we propose that evaluating the chest-to-head circumference ratio during the 34- to 36-week scan, in conjunction with known risk factors, may be predictive of fetal presentation at birth. It would be worthwhile to prospectively test this hypothesis in an antenatal population. Such findings could provide valuable insights for clinicians when counseling expectant mothers on their choice of birth mode.
Our study focused on live-born, non-anomalous singletons without maternal history of cesarean sections or uterine surgery, minimizing potential confounding. A large number of records enabled us to adjust for several important factors and allowed precise estimation of the associations that we found. As the JECS population is relatively homogenous, our findings should not have been influenced by racial and ethnic disparity, although their generalizability to other populations needs further research. The primary limitation of this study was potential misclassification of the chest-to-head circumference ratio groups, particularly among children delivered with a head-first presentation. Children born vertex vaginally have molded head, which might result in falsely low measurement of their head circumference. However, it is worth noting that those who delivered by cesarean may have maternal or fetal conditions that can affect a child’s chest size differently. Such factors could potentially obscure the true association between the chest-to-head circumference ratio and fetal presentation. Therefore, we suggest cautious interpretation of this study findings. Additionally, it is worth noting that the data were retrieved from medical records, which could potentially introduce some misclassification or omission of information regarding birth presentation. Furthermore, information on attempted external cephalic version was unavailable, although this procedure is uncommon in Japan. Therefore, its omission likely did not significantly affect our findings.
Conclusions
In conclusion, we found that the chest-to-head circumference ratio at birth influenced birth presentation: a low ratio was associated with an increased occurrence of breech presentation and transverse lie, whereas a high ratio was associated with a decreased occurrence of these presentations. Ultrasound evidence of a low fetal chest-to-head circumference ratio at 34–36 weeks’ gestation, combined with other risk factors, may predict non-cephalic presentation at birth. Prospective testing of this hypothesis in an antenatal population is warranted.
Author contributions
Naw Awn J-P: conceptualization and design, data curation, analysis and interpretation of data, drafting and revising the manuscript. Takafumi Watanabe: analysis and interpretation of data, critical revision of the manuscript. Masamitsu Eitoku: data curation, analysis and interpretation of data, critical revision of the manuscript. Keiko Yamasaki: data curation, analysis and interpretation of data, critical revision of the manuscript. Naomi Mitsuda: data curation, analysis and interpretation of data, critical revision of the manuscript. Nagamasa Maeda: analysis and interpretation of data, critical revision of the manuscript. Mikiya Fujieda: analysis and interpretation of data, critical revision of the manuscript. Narufumi Suganuma: funding acquisition, data curation, analysis and interpretation of data, critical revision of the manuscript. JECS Group members: data curation, critical revision of the manuscript. All authors have read and approved the final version.
Supplemental Material
Download MS Word (37.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are unsuitable for public deposition due to ethical restrictions and legal framework of Japan. It is prohibited by the Act on the Protection of Personal Information (Act No. 57 of 30 May 2003, amended on 9 September 2015) to publicly deposit the data containing personal information. Ethical Guidelines for Medical and Health Research Involving Human Subjects enforced by the Japan Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labor and Welfare, also restricts the open sharing of the epidemiologic data. All inquiries about access to data should be sent to: [email protected]. The person responsible for handling enquires sent to this e-mail address is Dr. Shoji F. Nakayama, JECS Programme Office, National Institute for Environmental Studies.
Additional information
Funding
References
- Sentilhes L, Schmitz T, Azria E, et al. Breech presentation: clinical practice guidelines from the French College of Gynaecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol. 2020;252:1–10. doi: 10.1016/j.ejogrb.2020.03.033.
- ACOG Committee Opinion No. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018;132(2):e60–e63. doi: 10.1097/AOG.0000000000002755.
- Management of breech presentation: green-top guideline no. 20b. BJOG. 2017;124(7):e151–e177. doi: 10.1111/1471-0528.14465.
- Minakami H, Maeda T, Fujii T, et al. Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2014 edition. J Obstet Gynaecol Res. 2014;40(6):1469–1499. doi: 10.1111/jog.12419.
- Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999;106(7):638–641. doi: 10.1111/j.1471-0528.1999.tb08360.x.
- Sagawa K, Suzuki S, Takeda S, et al. Trends in mode of breech delivery in Japan. Hypertens Res Pregnancy. 2021;9(2):26–29. doi: 10.14390/jsshp.HRP2020-017.
- Hehir MP, O’Connor HD, Kent EM, et al. Changes in vaginal breech delivery rates in a single large metropolitan area. Am J Obstet Gynecol. 2012;206(6):498.e1–498.e4. doi: 10.1016/j.ajog.2012.03.029.
- Post WM, Vlemmix F, de Hundt M, et al. Does vaginal breech delivery have a future despite low volumes for training? Results of a questionnaire. Eur J Obstet Gynecol Reprod Biol. 2018;229:123–126. doi: 10.1016/j.ejogrb.2018.08.020.
- De Castro H, Ciobanu A, Formuso C, et al. Value of routine ultrasound examination at 35–37 weeks’ gestation in diagnosis of non-cephalic presentation. Ultrasound Obstet Gynecol. 2020;55(2):248–256. doi: 10.1002/uog.21902.
- Kato K, Nagamatsu T, Yamaguchi S, et al. Changes in fetal presentation in the preterm period and the prediction of non-cephalic delivery. J Matern Fetal Neonatal Med. 2023;36(1):2141564. doi: 10.1080/14767058.2022.2141564.
- Toijonen AE, Heinonen ST, Gissler MVM, et al. A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study. Arch Gynecol Obstet. 2020;301(2):393–403. doi: 10.1007/s00404-019-05385-5.
- Noli SA, Baini I, Parazzini F, et al. Preterm birth, low gestational age, low birth weight, parity, and other determinants of breech presentation: results from a large retrospective population-based study. Biomed Res Int. 2019;2019:9581439. doi: 10.1155/2019/9581439.
- Zsirai L, Csákány GM, Vargha P, et al. Breech presentation: its predictors and consequences. An analysis of the Hungarian Tauffer Obstetric Database (1996–2011). Acta Obstet Gynecol Scand. 2016;95(3):347–354. doi: 10.1111/aogs.12834.
- Cammu H, Dony N, Martens G, et al. Common determinants of breech presentation at birth in singletons: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2014;177:106–109. doi: 10.1016/j.ejogrb.2014.04.008.
- Hiersch L, Melamed N. Fetal growth velocity and body proportion in the assessment of growth. Am J Obstet Gynecol. 2018;218(2S):S700–S711.e1. doi: 10.1016/j.ajog.2017.12.014.
- J-P NA, Mitsuda N, Eitoku M, et al. Influence of chest/head circumference ratio at birth on obstetric and neonatal outcomes: the Japan Environment and Children’s Study. Am J Hum Biol. 2023;35(6):e23875. doi: 10.1002/ajhb.23875.
- Michikawa T, Nitta H, Nakayama SF, et al. Baseline profile of participants in the Japan Environment and Children’s Study (JECS). J Epidemiol. 2018;28(2):99–104. doi: 10.2188/jea.JE20170018.
- Kawamoto T, Nitta H, Murata K, et al. Rationale and study design of the Japan Environment and Children’s Study (JECS). BMC Public Health. 2014;14(1):25. doi: 10.1186/1471-2458-14-25.
- Itabashi K, Miura F, Uehara R, et al. New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr Int. 2014;56(5):702–708. doi: 10.1111/ped.12331.
- Miller SL, Huppi PS, Mallard C. The consequences of fetal growth restriction on brain structure and neurodevelopmental outcome. J Physiol. 2016;594(4):807–823. doi: 10.1113/JP271402.
- Andersen GL, Irgens LM, Skranes J, et al. Is breech presentation a risk factor for cerebral palsy? A Norwegian birth cohort study. Dev Med Child Neurol. 2009;51(11):860–865. doi: 10.1111/j.1469-8749.2009.03338.x.
- Suzuki S, Yamamuro T. Fetal movement and fetal presentation. Early Hum Dev. 1985;11(3–4):255–263. doi: 10.1016/0378-3782(85)90079-9.
- Sekulic SR. Possible explanation of cephalic and noncephalic presentation during pregnancy: a theoretical approach. Med Hypotheses. 2000;55(5):429–434. doi: 10.1054/mehy.2000.1083.
- Kohls F, Gebauer F, Flentje M, et al. Current approach for external cephalic version in Germany. Geburtshilfe Frauenheilkd. 2020;80(10):1041–1047. doi: 10.1055/a-1127-8646.
- Owada M, Suzuki S. Outcomes of "one-day trial of vaginal breech delivery of singleton pregnancy" at 37–38 weeks’ gestation at a Japanese perinatal center. J Matern Fetal Neonatal Med. 2021;34(21):3510–3513. doi: 10.1080/14767058.2019.1686471.
- Zielbauer AS, Louwen F, Jennewein L. External cephalic version at 38 weeks’ gestation at a specialized German single center. PLOS One. 2021;16(8):e0252702. doi: 10.1371/journal.pone.0252702.
- Hehir MP, Ananth CV, Siddiq Z, et al. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. Am J Obstet Gynecol. 2018;219(1):105.e1–105.e11. doi: 10.1016/j.ajog.2018.04.012.
- Lyons J, Pressey T, Bartholomew S, et al. Delivery of breech presentation at term gestation in Canada, 2003–2011. Obstet Gynecol. 2015;125(5):1153–1161. doi: 10.1097/AOG.0000000000000794.
- Sandall J, Tribe RM, Avery L, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018;392(10155):1349–1357. doi: 10.1016/s0140-6736(18)31930-5.
- Zhang T, Sidorchuk A, Sevilla-Cermeno L, et al. Association of cesarean delivery with risk of neurodevelopmental and psychiatric disorders in the offspring: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(8):e1910236. doi: 10.1001/jamanetworkopen.2019.10236.
- Thomas J, Olukade TO, Naz A, et al. The neonatal respiratory morbidity associated with early term caesarean section – an emerging pandemic. J Perinat Med. 2021;49(7):767–772. doi: 10.1515/jpm-2020-0402.
- Horiuchi S, Shinohara R, Otawa S, et al. Elective cesarean delivery at term and its effects on respiratory distress at birth in Japan: the Japan Environment and Children’s Study. Health Sci Rep. 2021;4(4):e421. doi: 10.1002/hsr2.421.
- Kotecha SJ, Gallacher DJ, Kotecha S. The respiratory consequences of early-term birth and delivery by caesarean sections. Paediatr Respir Rev. 2016;19:49–55. doi: 10.1016/j.prrv.2015.12.002.
- Crump C, Sundquist J, Sundquist K. Preterm or early term birth and risk of attention-deficit/hyperactivity disorder: a national cohort and co-sibling study. Ann Epidemiol. 2023;86:119–125.e4. doi: 10.1016/j.annepidem.2023.08.007.
- Rabie NZ, Bird TM, Magann EF, et al. ADHD and developmental speech/language disorders in late preterm, early term and term infants. J Perinatol. 2015;35(8):660–664. doi: 10.1038/jp.2015.28.
- Risnes K, Bilsteen JF, Brown P, et al. Mortality among young adults born preterm and early term in 4 Nordic nations. JAMA Netw Open. 2021;4(1):e2032779. doi: 10.1001/jamanetworkopen.2020.32779.
- Cobec IM, Varzaru VB, Kövendy T, et al. External cephalic version—a chance for vaginal delivery at breech presentation. Medicina. 2022;58(11):1619. doi: 10.3390/medicina58111619.
- Louwen F, Daviss BA, Johnson KC, et al. Does breech delivery in an upright position instead of on the back improve outcomes and avoid cesareans? Int J Gynaecol Obstet. 2017;136(2):151–161. doi: 10.1002/ijgo.12033.
- Westgren M, Edvall H, Nordström L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985;92(1):19–22. doi: 10.1111/j.1471-0528.1985.tb01043.x.
Appendix 1
We are grateful to all the participants and staff involved in the Japan Environment and Children’s Study (JECS). The members of the JECS Group as of 2023: Michihiro Kamijima (principal investigator, Nagoya City University, Nagoya, Japan), Shin Yamazaki (National Institute for Environmental Studies, Tsukuba, Japan), Yukihiro Ohya (National Center for Child Health and Development, Tokyo, Japan), Reiko Kishi (Hokkaido University, Sapporo, Japan), Nobuo Yaegashi (Tohoku University, Sendai, Japan), Koichi Hashimoto (Fukushima Medical University, Fukushima, Japan), Chisato Kishi (Fukushima, Japan), Chisato Mori (Chiba University, Chiba, Japan), Shuichi Ito (Yokohama City University, Yokohama, Japan), Zentaro Yamagata (University of Yamanashi, Chuo, Japan), Hidekuni Inadera (University of Toyama, Toyama, Japan), Takeo Nakayama (Kyoto University, Kyoto, Japan), Tomotaka Sobue (Osaka University, Kyoto, Japan), Tomotaka Sobue (Osaka University, Osaka, Japan) Tomotaka Sobue (Osaka University, Suita, Japan), Masayuki Shima (Hyogo Medical University, Nishinomiya, Japan), Seiji Kageyama (Tottori University Yonago, Japan), Narufumi Suganuma (Kochi University, Nankoku, Japan), Shoichi Ohga (Kyushu University, Fukuoka, Japan), and Takahiko Katoh (Kumamoto University, Kumamoto, Japan).