Abstract
Background
The US still has a high burden of preterm birth (PTB), with important disparities by race/ethnicity and poverty status. There is a large body of literature looking at the impact of pre-pregnancy obesity on PTB, but fewer studies have explored the association between underweight status on PTB, especially with a lens toward health disparities. Furthermore, little is known about how weight, specifically pre-pregnancy underweight status, and socio-economic-demographic factors such as race/ethnicity and insurance status, interact with each other to contribute to risks of PTB.
Objectives
The objective of this study was to measure the association between pre-pregnancy underweight and PTB and small for gestational age (SGA) among a large sample of births in the US. Our secondary objective was to see if underweight status and two markers of health disparities – race/ethnicity and insurance status (public vs. other) – on PTB.
Study design
We used data from all births in California from 2011 to 2017, which resulted in 3,070,241 singleton births with linked hospital discharge records. We ran regression models to estimate the relative risk of PTB by underweight status, by race/ethnicity, and by poverty (Medi-cal status). We then looked at the interaction between underweight status and race/ethnicity and underweight and poverty on PTB.
Results
Black and Asian women were more likely to be underweight (aRR = 1.0, 95% CI: 1.01, 1.1 and aRR = 1.4, 95% CI: 1.4, 1.5, respectively), and Latina women were less likely to be underweight (aRR = 0.7, 95% CI: 0.7, 0.7). Being underweight was associated with increased odds of PTB (aRR = 1.3, 95% CI 1.3–1.3) and, after controlling for underweight, all nonwhite race/ethnic groups had increased odds of PTB compared to white women. In interaction models, the combined effect of being both underweight and Black, Indigenous and People of Color (BIPOC) statistically significantly reduced the relative risk of PTB (aRR = 0.9, 95% CI: 0.8, 0.9) and SGA (aRR = 1.0, 95% CI: 0.9, 1.0). The combined effect of being both underweight and on public insurance increased the relative risk of PTB (aRR = 1.1, 95% CI: 1.1, 1.2) but there was no additional effect of being both underweight and on public insurance on SGA (aRR = 1.0, 95% CI: 1.0, 1.0).
Conclusions
We confirm and build upon previous findings that being underweight preconception is associated with increased risk of PTB and SGA – a fact often overlooked in the focus on overweight and adverse birth outcomes. Additionally, our findings suggest that the effect of being underweight on PTB and SGA differs by race/ethnicity and by insurance status, emphasizing that other factors related to inequities in access to health care and poverty are contributing to disparities in PTB.
Introduction
Poor birth outcomes, including preterm birth (PTB) and small for gestational age (SGA), persist both in the United States (US) and globally [Citation1]. Inequalities in PTB rates exist in both contexts by race/ethnic group, socio-economic status (income, education, and occupation), migration status, age, and insurance type. Understanding inequalities in women’s risk of adverse birth outcomes is important for developing targeted interventions to reduce the incidence of adverse birth outcomes including PTB and SGA birth as well as other adverse outcomes [Citation2]. In the US, Black, Hispanic, and Native American/Pacific islander women have worse birth outcomes than white women. Preterm birth is also associated with poverty (as measured by Medicaid coverage) [Citation3,Citation4] and expansions in Medicaid coverage are associated with improved equity in the birth weight of babies born preterm [Citation5]. As has been discussed and explored in great detail by members of our study team in other publications, for this study, we are assuming that “structural racism creates a hierarchy of power, domination, and privilege in society that impacts the distribution and expression of illness and health as well as access to and utilization of resources…” [Citation6]. Maternal body mass index (BMI) is associated with poor birth outcomes, with much of the focus in the literature in the US on the link between obesity and poor birth outcomes [Citation7]. Evidence also suggests that being underweight (pre-pregnancy BMI ≤18.5) is associated with adverse birth outcomes [Citation8], including an increased risk of preterm and low birth weight [Citation9].
Inequalities in BMI by race/ethnicity and socio-economic status also exist in the US, with Hispanic women being less likely to be underweight than Black and White women, and with White women having the highest rate of being underweight [Citation10]. Poverty in the US is also associated with BMI, especially for women, with poverty being more highly associated with being obese for black compared to white women [Citation11].
As with the research on race/ethnicity and PTB, much of the literature on BMI, PTB, and race/ethnicity has focused on women being overweight before or during pregnancy, with less research looking at race/ethnicity, being underweight, and PTB [Citation12]. A systematic review and meta-analysis of papers from around the world found that being underweight was associated with PTB in developed but not developing countries [Citation9]. Of the studies found in the US, a relationship has been identified between pre-pregnancy low BMI and PTB, though most of these have focused on one race/ethnic group at a time [Citation13–15]. Proposed explanations for this association include lack of nutrients or other potential confounding behavioral factors such as smoking, mental illness, etc. [Citation16,Citation17].
Of note is that many of these studies are over 15 years old. For example, a study using data from the 1980s found that there was an association between being underweight and having a PTB and found that Black and Latina women at the highest risk [Citation18]. In 2014, Shaw et al. used California birth record data (as we do in this study) to study the relationship between BMI and PTB and conducted sub-group analyses by race/ethnicity to explore differences by parity. Though, like others, they mostly focused on findings related to women being overweight or obese, they did find an increased risk of late PTB in underweight women across all race/ethnic groups [Citation19]. Torloni et al. looked at whether race modified the relationship between being underweight and having a PTB and found differences in PTB risk by ethnic groups and BMI categories which were found to differ by timing of PTB (early/late). Torloni et al. study used a very small sample of women from Tennessee, only looked at two race/ethnic groups (African American compared to white women), did not have a measure for poverty, and only looked at PTB as an outcome [Citation20]. It should be noted that a number of studies have looked at race, pregnancy weight gain, and PTB in the US [Citation21,Citation22].
More research is needed that explores the relationship between race/ethnicity, socio-economic status (poverty), low BMI, and adverse birth outcomes using more recent and large-scale data. Furthermore, exploring if race/ethnicity and socio-economic status modify the relationship between low BMI and adverse birth outcomes could help us better understand who is most at risk and how to best design and target interventions.
Study objectives: Using data from over 3.4 million births from the California Birth and Hospital Discharge record cohort files from 2011 to 2017, this study explored disparities in being underweight across race/ethnicity and MediCal groups (wherein MediCal was used as a proxy for poverty), explored disparities in PTB and SGA by underweight status, and this study examined whether race/ethnicity and public insurance/other insurance modify the relationship between being underweight and having a PTB or SGA birth.
Materials and methods
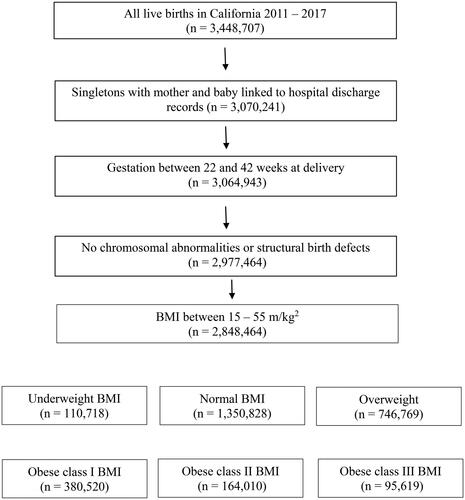
The sample was drawn from all California live born infants between 2011 and 2017. Birth certificates, maintained by California Vital Statistics, were linked to hospital discharge, emergency department, and ambulatory surgery records maintained by the California Office of Statewide Health Planning and Development. These databases contain detailed information on maternal and infant characteristics, hospital discharge diagnoses, and procedures. Hospital discharge, emergency department, and ambulatory surgery files provided diagnoses and procedure codes based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) and International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10) as reported to the California Office of Statewide Health Planning and Development by health care facilities. The study sample was restricted to singletons born between 22 and 44 weeks gestation (viable ages at birth), with linked birth records for mother and infant, and infants without chromosomal abnormalities or major structural birth defects (since these are independent reasons for PTB or SGA). We use only singletons because otherwise mother’s pregnancy data would be included twice, complicating our models, and we use linked data because we have appropriate co-variates for our analysis. Structural birth defects for the study were considered “major” if determined by clinical review as causing major morbidity and mortality that would likely be identified in the hospital at birth or lead to hospitalization during the first year of life [Citation23]. Body mass index was calculated from maternal height and prepregnancy weight, obtained from birth certificate records. Women without recorded height or weight, or with BMI <15 kg/m2 or >55 kg/m2 were excluded from the study ().
Core outcomes set: primary measures: Underweight was defined as having a BMI < 18.5 kg/m2, compared to normal weight women (BMI 18.5–25 kg/m2), as per usual guidelines, including the Centers for Disease Control in the US (https://www.cdc.gov/obesity/basics/adult-defining.html). Primary outcomes were PTB defined as <37 weeks at birth and SGA, defined as <10th percentile for weight by gestational age (calculated using infant sex, GA, and birthweight) [Citation24]. Race was defined as a categorical variable (Black, White, Hispanic, Asian, Other (Native American, Pacific Islander, other race, two or more races, or not stated/unknown)) and we also created a binary variable for BIPOC (Black, Indigenous, People of color) which included everyone who did not identify as white, not Hispanic. Three questions about race and ethnicity were asked separately in the birth certificate and from these questions, we created a single variable that combined data on race and ethnicity. Public insurance status was defined as MediCal compared to not public insurance (included private, other government (military or other), self-pay, none, and no self-pay/private insurance). MediCal is California’s state funded Medicaid for low-income persons, and this was used as a marker for poverty or low socio-economic status as only those with low-income qualify for MediCal. Women on MediCal receive free prenatal and postnatal care up to one year postpartum.
Confounding measures: Variables were created for socio-demographic characteristics including age (categorical <18, 18–34, and over 35), education (<12 years/over 12 years), parity (nulliparous/parous), and maternal country of birth (outside US/in US). Additional variables related to access to and quality of care included WIC participation (yes/no), and adequacy of prenatal care, which takes into account timing of prenatal care entry, number of visits, and gestational age [Citation25]. Finally, we included a number of pregnancy related risk factors known to be associated with PTB including smoking (yes/no), hypertension (yes/no), diabetes (yes/no), drug/alcohol use (yes/no), and mental health diagnosis (yes/no). There is evidence for other risk factors for PTB, such a domestic violence, which we do not have data on in this analysis [Citation26].
Patient involvement: No patients were involved, this study used anonymized birth records data.
Analysis
Race and underweight status: The first set of logistic regression models explored the association between a categorical race variable and being underweight/not, first as uni- and then as multi-variable models controlling for potential confounders. The second set of models looked at the same outcome, and the primary independent categorical variable of payer status (Medicare/Medical vs. other). Again, we ran uni- and multi-variable models, controlling for the same outcomes as above.
Preterm birth, small for gestational age, and underweight status. The next set of logistic regression models explored the relationship between being underweight, having a PTB, or having a baby born SGA. Two sets of models were run, one for each adverse birth outcome: PTB and SGA. The primary independent variable was underweight compared to normal weight. After running uni-variable (unadjusted) models, we controlled for the socio-economic and pregnancy related variables.
Interaction models: Interaction models allow us to operationalize the intersectionality between maternal health characteristics (in this case pre-pregnancy BMI) and race/ethnicity and poverty [Citation6]. We next tested if race/ethnicity and having MediCal/not modified the relationship between being underweight and having a PTB or SGA baby. We ran two sets of logistic regression models for each of the outcome variables described above: PTB and SGA. For each outcome, we looked at whether there was an interaction between (a) race/ethnicity and underweight status and (b) poverty and underweight status, in separate models. The confounders discussed above were included in each set of models.
All analyses were performed using Statistical Analysis Software version 9.4 (Cary, NC). Methods and protocols for the study were approved by the Committee for the Protection of Human Subjects within the Health and Human Services Agency of the State of California. This work was supported by the Population Health and Health Equity Scholars program and the California Preterm Birth Initiative within the University of California, San Francisco, CA.
Results
From an initial sample of just under 3.5 million births in California from 2011 to 2017, we narrowed our sample to 3,070,241 singleton births with linked hospital discharge records (). We further narrowed the sample to babies born at 22–42 weeks with no chromosomal abnormalities/birth defects and mothers with BMI between 15 and 55 m/kg, for a total of 2,848,464 births in our analysis.
shows the socio-demographics of each weight category. A larger proportion of underweight (BMI < 18.5 kg/m2) women were Asian, a larger proportion of overweight women were Latina and Black, and a larger proportion of normal weight women were White. A larger proportion of overweight women had public insurance, whereas normal weight and underweight women had more nonpublic insurance. Similarly, more overweight women were receiving benefits for Women and Children (WIC), compared to the other two groups. Underweight women were younger, and the age distribution was similar among overweight and normal weight women. Underweight and normal weight women had similar educational distributions, with overweight women having lower education levels.
Table 1. Descriptives of the population by weight category status.
In unadjusted (crude) models, all variables explored were significantly associated with underweight status (). In adjusted models, Black and Asian women were more likely to be underweight (RR = 1.0, 95% CI: 1.01, 1.1 and RR = 1.4, 95% CI: 1.4, 1.5, respectively), and Latina women were less likely to be underweight (RR = 0.7, 95% CI: 0.7, 0.7). Public insurance (RR = 1.2, 95% CI: 1.2, 1.2), WIC participation (RR = 1.1, 95% CI: 1.04, 1.1), being born outside the US (RR = 1.2, 95% CI: 1.1, 1.2), and being nulliparous (RR = 1.3, 95% CI: 1.3, 1.4) were associated with an increased likelihood of being underweight. Risk of being underweight decreased with age and education. Hypertension, diabetes, and c-section were associated with lower risk, while smoking and drug/alcohol use associated with higher risk of being underweight. Longer pregnancy interval was associated with lower risk and inadequate quality of prenatal care with higher risk of underweight.
Table 2. Relative risk of underweight by selected sociodemographics, unadjusted and adjusted models (relative risk, 95% confidence interval).
Being underweight was associated with increased odds of PTB (aRR = 1.3, 95% CI 1.3–1.3) (). All race/ethnic groups had increased odds of PTB, after controlling for underweight, compared to white women. Similar trends were observed for births <32 weeks, births 32–36 weeks and SGA.
Table 3. Relative risk of birth outcomes: preterm birth, <32 weeks, 32–36 weeks and small for gestational age (SGA) by underweight status, univariate and multivariate models (relative risk, 95% confidence interval).
In interaction models adjusting for all covariates in , BIPOC (aRR = 1.4, 95% CI: 1.4, 1.4) and underweight status (aRR = 1.5, 95% CI: 1.4, 1.5) were significantly associated with an increased relative risk of PTB; however, the combined effect of being both underweight and BIPOC statistically significantly reduced the relative risk of PTB (aRR = 0.9, 95% CI: 0.8, 0.9) (). Similarly, BIPOC (aRR = 1.4, 95% CI: 1.4, 1.5) and underweight status (aRR = 1.5, 95% CI: 1.5, 1.6) were associated with statistically significant increased relative risk of SGA, and again, the combined effect of being both underweight and BIPOC reduced the relative risk of SGA, again significantly (aRR = 1.0, 95% CI: 0.9, 1.0).
Table 4. Relative risk of preterm and SGA, moderation by race/ethnicity and underweight (relative risk, 95% confidence interval).
In the next set of adjusted interaction models, public insurance status (aRR = 1.1, 95% CI: 1.1, 1.1) and underweight status (aRR = 1.2, 95% CI: 1.2, 1.3) were both significantly associated with an increased relative risk of PTB, and the combined effect of being both underweight and on public insurance additionally and significantly increased the relative risk of PTB (aRR = 1.1, 95% CI: 1.1, 1.2) (). While public insurance status (aRR = 1.1, 95% CI: 1.1, 1.1) and underweight status (aRR = 1.4, 95% CI: 1.4, 1.5) were both significantly associated with an increased relative risk of SGA, there was no additional effect of the two in the interaction models (aRR = 1.0, 95% CI: 1.0, 1.0).
Table 5. Relative risk of preterm and SGA, moderation by public insurance and underweight (relative risk, 95% confidence interval).
Discussion
The present study represents a critically important update to and expansion of what is known about the association between being underweight and having a PTB or a baby born small-for-gestational age. It also expands our understanding of associated race/ethnicity and socioeconomic disparities. It highlights that low BMI is a potential risk factor for poor birth outcomes, especially when compounded by other intersecting social risk factors including structural racism and poverty.
In this sample of more than 2.8 million births in California from 2011 to 2017, we found that being underweight increased the likelihood that a woman would experience a PTB or have a SGA baby. BIPOC women and women with public insurance were more likely than White women and those without public insurance to experience these outcomes. The combined effect of being on public insurance (a marker of low socio-economic status or poverty) and being underweight was found to increase the risk of PTB or being small-for-gestational age.
This study adds to the limited previous evidence showing that underweight status is an important factor to consider when investigating race/ethnic and socioeconomic disparities in birth outcomes [Citation9,Citation13,Citation14]. Similar to Shaw et al., we found that pre-pregnancy underweight was associated with increased risk of PTB, and by not stratifying by race we see that the risk differed by race/ethnicity, similar to Simhan and Bodnar [Citation18,Citation19]. Our study extends the previous research by looking at the interaction between race/ethnicity and poverty on PTB, instead of each outcome on its own.
With respect to pathophysiology, underweight status has been hypothesized to increase the risk of PTB through a number of pathways including, for example, chronic maternal undernutrition, low concentration of macro- or micro-nutrients, endocrine factors, placental growth restriction, and infection/inflammation from an altered immune system [Citation27]. Recent studies have suggested that it may even be possible to predict the risk of PTB by combining information on BMI and metabolomic markers (markers of inflammation) [Citation28]. Others have suggested that maternal thinness associated with low pre-pregnancy BMI may lead to decreased blood volume and reduced uterine blood flow [Citation29]. In exploring the pathophysiological underpinnings of underweight-outcome relationships and associated race/ethnic and socioeconomic disparities, it is critical to note that social-determinants of health and the impact of structural racism on the lives and bodies of minoritized pregnant women, have ties to all of these pathways (e.g. weight, nutrition/food insecurity, endocrine function, placental function, and inflammation) [Citation6,Citation30–33]. As such, as this work progresses it will be critical to examine these interrelationships – particularly as strategies for intervention are developed.
Future research should seek to understand the pathways and mechanisms through which these social disparities interact with pre-pregnancy underweight to put women more (or less) at risk of PTB. Research that engaged women to help identify causes as well as solutions for these findings through community engaged research would be beneficial. Expanding this research to other states in the US which have different demographic distributions by race/ethnicity, different histories especially related to racism, and different types of additional social support and programs for those living in poverty, could help disentangle the causes of these associations and how they differ across populations.
Strengths and limitations
Strengths of the present study include its use of a large diverse population-based sample of births with detailed demographic and clinical information available for use. The study represents an important expansion of what is currently known in this space – this is especially true for the US as a large proportion of previous research on this topic has been in low- and middle-income countries (with higher levels of underweight women and potentially different drivers of underweight status) [Citation9].
As work progresses in this field, it will be important to address the gaps highlighted by the limitations of this study. Notably, BMI was self-reported, and thus may be subject to reporter error or bias. BMI is generally under-estimated, and there is evidence of difference in self-report of BMI by race/ethnicity [Citation34]. The date of recording of BMI is also unknown, and thus may differ between participants. Also, while we have a very large sample size, it is only from one state in the US, and therefore it is possible that the association between race/ethnicity, insurance, underweight, and PTB may differ across the US where women’s health and social experiences may differ greatly. Finally, data analyzed from sources that only include records of live births could be prone to bias from lack of information on competing events (e.g. only some women are able to get pregnant or maintain a pregnancy, and this may differ by the other covariates under study, such as maternal weight) [Citation35].
Conclusions
The findings of this analysis are likely to help programs or policy makers working to reduce adverse birth outcomes as it provides evidence for focusing interventions on populations of pregnant women that are at increased risk (underweight) and carefully considering the interplay of other factors (experiencing poverty or other inequalities due to structural racism) in California and, likely, elsewhere. Additionally, these findings will help broaden the perspective of those focused on prevention by highlighting the importance of pregnancy underweight, in addition to the much-discussed impact of obesity. These findings also provide evidence for the need of multi-pronged interventions that address not only women’s weight but that also address structural determinants.
Author contributions
ND-S: conceptualization, writing – original draft, funding acquisition, and methodology. RJB: formal analysis, writing – review and editing, methodology. LJ-P: conceptualization, writing – review and editing, supervision, funding acquisition.
Ethics statement
Methods and protocols for the study were approved by the Committee for the Protection of Human Subjects within the Health and Human Services Agency of the State of California.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are publicly available upon request from the California Department of Public Health.
Additional information
Funding
References
- Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):1–9. doi: 10.1016/S2214-109X(18)30451-0.
- Ratnasiri AWG, Parry SS, Arief VN, et al. Recent trends, risk factors, and disparities in low birth weight in California, 2005–2014: a retrospective study. Matern Health Neonatol Perinatol. 2018;4(1):15. doi: 10.1186/s40748-018-0084-2.
- Margerison-Zilko C, Cubbin C, Jun J, et al. Beyond the cross-sectional: neighborhood poverty histories and preterm birth. Am J Public Health. 2015;105(6):1174–1180. doi: 10.2105/AJPH.2014.302441.
- Krieger N, Van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York city, 2013–2017. Am J Public Health. 2020;110(7):1046–1053. doi: 10.2105/AJPH.2020.305656.
- Brown CC, Moore JE, Felix HC, et al. County-Level variation in low birthweight and preterm birth: an evaluation of state medicaid expansion under the affordable care act. Med Care. 2020;58(6):497–503. doi: 10.1097/MLR.0000000000001313.
- Scott KA, Chambers BD, Baer RJ, et al. Preterm birth and nativity among black women with gestational diabetes in California, 2013–2017: a population-based retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):593. doi: 10.1186/s12884-020-03290-3.
- Sutherland G, Brown S, Yelland J. Applying a social disparities lens to obesity in pregnancy to inform efforts to intervene. Midwifery. 2013;29(4):338–343. doi: 10.1016/j.midw.2012.01.016.
- Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–451. doi: 10.1016/S0140-6736(13)60937-X.
- Han Z, Mulla S, Beyene J, et al. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. 2011;40(1):65–101. doi: 10.1093/ije/dyq195.
- Headen I, Mujahid MS, Cohen AK, et al. Racial/ethnic disparities in inadequate gestational weight gain differ by pre-pregnancy weight. Matern Child Health J. 2015;19(8):1672–1686. doi: 10.1007/s10995-015-1682-5.
- Do DP, Zheng C. A marginal structural modeling strategy investigating short and long-term exposure to neighborhood poverty on BMI among U.S. black and white adults. Health Place. 2017;46:201–209. doi: 10.1016/j.healthplace.2017.05.010.
- Liu B, Xu G, Sun Y, et al. Association between maternal pre-pregnancy obesity and preterm birth according to maternal age and race or ethnicity: a population-based study. Lancet Diabetes Endocrinol. 2019;7(9):707–714. doi: 10.1016/S2213-8587(19)30193-7.
- Siega-Riz AM, Adair LS, Hobel CJ. Maternal underweight status and inadequate rate of weight gain during the third trimester of pregnancy increases the risk of preterm delivery. J Nutr. 1996;126(1):146–153. doi: 10.1093/jn/126.1.146.
- Johnson AA, Knight EM, Edwards CH, et al. Selected lifestyle practices in urban African American women – relationships to pregnancy outcome, dietary intakes and anthropometric measurements. J Nutr. 1994;124(6 Suppl.):963S–972S.
- Moutquin JM. Socio-economic and psychosocial factors in the management and prevention of preterm labour. BJOG. 2003;110(Suppl. 20):56–60. doi: 10.1046/j.1471-0528.2003.00031.x.
- Linna MS, Raevuori A, Haukka J, et al. Pregnancy, obstetric, and perinatal health outcomes in eating disorders. Am J Obstet Gynecol. 2014;211(4):392.e1–392.e8. doi: 10.1016/j.ajog.2014.03.067.
- Girsen AI, Mayo JA, Carmichael SL, et al. Women’s prepregnancy underweight as a risk factor for preterm birth: a retrospective study. BJOG. 2016;123(12):2001–2007. doi: 10.1111/1471-0528.14027.
- Simhan HN, Bodnar LM. Prepregnancy body mass index, vaginal inflammation, and the racial disparity in preterm birth. Am J Epidemiol. 2006;163(5):459–466. doi: 10.1093/aje/kwj053.
- Shaw GM, Wise PH, Mayo J, et al. Maternal prepregnancy body mass index and risk of spontaneous preterm birth. Paediatr Perinat Epidemiol. 2014;28(4):302–311. doi: 10.1111/ppe.12125.
- Torloni MR, Fortunato SJ, Betrán AP, et al. Ethnic disparity in spontaneous preterm birth and maternal pre-pregnancy body mass index. Arch Gynecol Obstet. 2012;285(4):959–966. doi: 10.1007/s00404-011-2102-8.
- Ogunyemi D, Hullett S, Leeper J, et al. Prepregnancy body mass index, weight gain during pregnancy, and perinatal outcome in a rural black population. J Matern Fetal Med. 1998;7(4):190–193. doi: 10.1002/(SICI)1520-6661(199807/08)7:4<190::AID-MFM5>3.3.CO;2-2.
- Leonard SA, Petito LC, Stephansson O, et al. Weight gain during pregnancy and the black-white disparity in preterm birth. Ann Epidemiol. 2017;27(5):323–328.e1. doi: 10.1016/j.annepidem.2017.05.001.
- Baer RJ, Norton ME, Shaw GM, et al. Risk of selected structural abnormalities in infants after increased nuchal translucency measurement. Am J Obstet Gynecol. 2014;211(6):675.e1–675.e19. doi: 10.1016/j.ajog.2014.06.025.
- Talge NM, Mudd LM, Sikorskii A, et al. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133(5):844–853. doi: 10.1542/peds.2013-3285.
- Kotelchuck M. The adequacy of prenatal care utilization index: its US distribution and association with low birthweight. Am J Public Health. 1994;84(9):1486–1489. doi: 10.2105/ajph.84.9.1486.
- Neggers Y, Goldenberg R, Cliver S, et al. Effects of domestic violence on preterm birth and low birth weight. Acta Obstet Gynecol Scand. 2004;83(5):455–460. doi: 10.1080/j.0001-6349.2004.00458.x.
- Lynch AM, Hart JE, Agwu OC, et al. Association of extremes of prepregnancy BMI with the clinical presentations of preterm birth. Am J Obstet Gynecol. 2014;210(5):428.e1–428.e9. doi: 10.1016/j.ajog.2013.12.011.
- Borkowski K, Newman JW, Aghaeepour N, et al. Mid-gestation serum lipidomic profile associations with spontaneous preterm birth are influenced by body mass index. PLOS One. 2020;15(11):e0239115. doi: 10.1371/journal.pone.0239115.
- Neggers Y, Goldenberg RL. Some thoughts on body mass index, micronutrient intakes and pregnancy outcome. J Nutr. 2003;133(5 Suppl. 2):1737S–1740S. doi: 10.1093/jn/133.5.1737S.
- Slaughter-Acey JC, Talley LM, Stevenson HC, et al. Personal versus group experiences of racism and risk of delivering a small-for-gestational age infant in African American women: a life course perspective. J Urban Health. 2019;96(2):181–192. doi: 10.1007/s11524-018-0291-1.
- Thornburg KL, Boone-Heinonen J, Valent AM. Social determinants of placental health and future disease risks for baby. Obstet Gynecol Clin North Am. 2020;47(1):1–15. doi: 10.1016/j.ogc.2019.11.002.
- Giscombé CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: the impact of stress, racism, and related factors in pregnancy. Psychol Bull. 2005;131(5):662–683. doi: 10.1037/0033-2909.131.5.662.
- Manuck TA. Racial and ethnic differences in preterm birth: a complex, multifactorial problem. Semin Perinatol. 2017;41(8):511–518. doi: 10.1053/j.semperi.2017.08.010.
- Quick V, Byrd-Bredbenner C, Shoff S, et al. Concordance of self-report and measured height and weight of college students. J Nutr Educ Behav. 2015;47(1):94–98. doi: 10.1016/j.jneb.2014.08.012.
- Oken E, Aris IM, Young JG. Pre-pregnancy weight and preterm birth: a causal relation? Lancet Diabetes Endocrinol. 2019;7(9):663–665. doi: 10.1016/S2213-8587(19)30252-9.