Abstract
Objectives
Sonographic evaluation of the basilar artery is challenging, and a limited number of reports are available about the prenatal period, as manual positioning of probes is technically difficult. The objective of this study was to describe a sonographic transabdominal approach based on slowflow HD for screening of the basilar artery during the second trimester scan.
Methods
A total of 49 women who were enrolled in a second trimester screening were included when the fetus was in the occipitoanterior position. Dopper screening of the cerebral artery was performed, which revealed the “Y” sign indicating the basilar trunk arising from two vertebral arteries in the axial oblique view when the probe was located around the junction of the vertebral processes and occipital bone and was superior to the first vertebral body, sloping slightly to the cephalic side. The Doppler ultrasound probe was placed perpendicular to the basilar artery. The flow direction was below the baseline, away from the probe in the basilar artery, consistent with a caudocephalic orientation. Peak systolic and diastolic velocities were measured.
Results
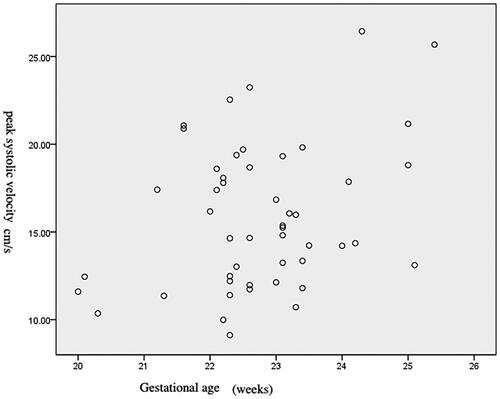
The basilar artery was identified in all 49 fetuses, with a mean gestational age of 22 weeks (range 20 to 26 weeks). The mean peak systolic velocity of the basilar artery was 15.8 cm/second (range 9.12-26.44 cm/second). There was a slight increase in peak systolic velocity according to the gestational age of the fetus.
Conclusions
This study demonstrated that evaluation of the basilar artery can be performed during the second trimester via a new transabdominal approach involving slowflow HD.
Introduction
Congenital morphological abnormalities of the basilar artery, including fenestrations, elongations, and aneurysms, have been reported [Citation1]. However, the available data on prenatal imaging of the basilar artery are limited. The bilateral vertebral arteries and basilar artery can be imaged in the coronal plane even at 12 weeks of gestation using transvaginal ultrasound [Citation2], and transabdominal insonation for the fetal basilar artery by ultrasound is also feasible [Citation3]. The recently developed Doppler tool SlowFlow has been used to visualize low-velocity blood perfusion in small vessels. There have also been two reports on 2D/3D SlowflowHD features of the fetal basilar artery [Citation4,Citation5].
Complex and varied adult cerebral angioarchitecture is inevitably associated with the origins of embryologic development. Both normal components and abnormalities evolve from modifications of primitive vessels. Studying the morphologic features of the basilar artery prenatally may reveal associated variants and/or pathologies. Morphologically, the basilar artery appears when the convergent junction of two vertebral arteries on the ventral side of the rhombencephalon is revealed, usually at the level of the onsoblongata. We performed a study to measure the basilar artery in a coronal view and measured the blood flow velocities via slow-flow HD ultrasound.
Methods
A cohort of fetuses who underwent ultrasound scans as part of routine care at the Third Affiliated Hospital of Zhengzhou University between November 29, 2023, and December 13, 2023, were included. All mothers signed informed consent for the ultrasound scan. The ultrasound scan recorded growth data for all fetuses in addition to several other indices for identifying any growth retardation or congenital malformation.
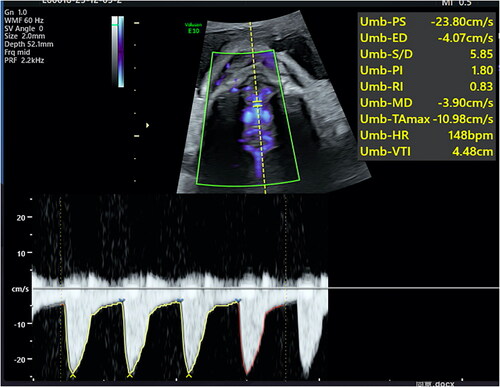
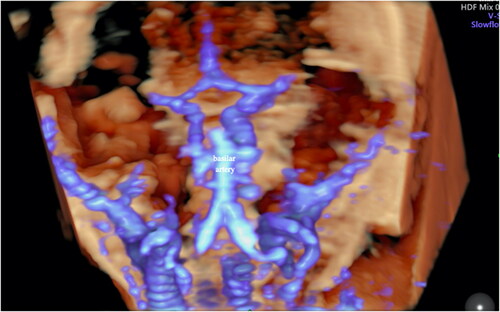
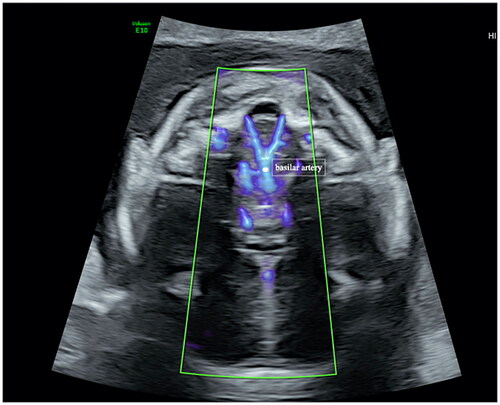
Doppler Doppler imaging was performed using GE10(GE Healthcare, Zipf, Austria) ultrasound devices with a C1-6(2-5MHz) convex probe and RM7C(2-8 MHz) probes. All the data were acquired by transabdominal sonography. The machine settings used were predetermined for slowflow HD (HDF map “5”, radiant flow “Min”, frequency “mid”, flow res “low”, line filter “2”, smooth “5”, and line density “4”). and PW (sweep speed “4”, and WMF 60HZ) with individualized gain and a 3D slow-flow HD volume predetermined brain mode set at a 40° volume angle. Ultrasound examination of the basilar artery was performed by one observer (ZF. Zhu) in all the cases. The basilar artery and vertebral arteris could be identified as “Y” in oblique axial section inferior to the occipital bone as the basilar trunk, arising from two vertebral arteries when the fetus was in an occipitoanterior position using slowflow HD when the probe was around the junction of the vertebral processes and occipital bone and was superior to the first vertebral body, sloping slightly to the cephalic side (). The morphology of the vessel filled with Doppler flow could be observed, and its peak systolic velocities could be measured. The Doppler ultrasound probe was placed perpendicular to the basilar artery. The flow direction was below the baseline and perpendicular to the probe in the basilar artery, consistent with a caudocephalic orientation (). The Doppler beam was directed along the basilar artery, and the sample volume was placed over the proximal section where the basilar artery emerged from the confluence of the vertebral arteries. The insonation angle was 0°. Doppler waveforms were acquired without fetal body movements over at least three consistent heart cycles and were automatically traced. Three-dimensional slowflowHD could help to visualize the morphology of the basilar artery and two vertebral arteries (). It took less than 5 min.
Figure 1. The basilar artery was identified in the oblique axial transabdominal plane at the level of the medulla oblongata in a 21-week, 6-day-old gestational fetus using SlowFlow HD ultrasound.
Results
We attempted to observe the basilar artery in 49 fetuses in the occipitoanterior position; the mean gestational age was 22 weeks (range 22 weeks to 26 weeks), and the fetuses exhibited accompanying fetal motion or maternal discomfort. The median maternal age at examination in the present study was 31 (range, 21–43) years. The conditions of the pregnant women were stable. All 49 fetuses were appropriate-for-gestational-age and morphologically normal singleton fetuses without complications. These fetuses are still under follow-up and have not been delivered. All the basilar arteries could be visualized, and the peak velocity was measured and recorded. The mean peak systolic velocity of the basilar artery was 15.8 cm/second (range 9.12-26.44 cm/second). The peak systolic velocity was 1.145 × (gestational age) −10.172 (F = 5.506, p = 0.023). There was a slight increase in the peak systolic velocity according to the gestational age of the fetus ().
Discussion
Assessment of the fetal cerebral artery provides important information associated with the fetus in the uterus. To date, fetal brain artery evaluation has been performed mainly on the middle cerebral artery for hemodynamic and pericallosal artery reconstruction despite the development of ultrasonic techniques. The value of blood flow Doppler measurements in middle cerebral arteries is well established, aiding in the identification of fetuses at risk of adverse perinatal outcomes. Little is known about prenatal imaging of the basilar artery.
Cerebrovascular maturation occurs at the fourth week of gestation and occurs for the first several years of life. The aortic arches develop at six to eight weeks of gestation, contributing to the basic arterial structure in humans [Citation6]. Several morphological abnormalities of the basilar artery, such as aneurysms, have been reported to be present in the fetal stage [Citation1,Citation7].
Qureshi AI et al. demonstrated the feasibility of visualizing and measuring the flow velocities of the basilar artery of fetuses via transabdominal insonation [Citation3]. Our way to visualize the basilar artery was also through transabdominal insonation. Qureshi AI et al. demonstrated the feasibility of visualizing the basilar artery in the sagittal plane behind the clivus bone using directional color Doppler ultrasound. Our method for observing the basilar artery in the second trimester involved the oblique axial plane, which was different from that used by Qureshi AI et al. and the signs of “Y” formed by the basilar artery and vertebral artery could be clearly displayed. The fetal basilar artery could be observed in all fetuses in the second trimester if the fetus was in an appropriate position. The difference in the mean peak systolic velocity of the basilar artery between our study and that of Qureshi AI et al. might be correlated with the difference in gestational age between the two studies. We used the SlowFlowHD technique to visualize the artery. Slow-flow HD Doppler revealed slow-velocity vessels in the fetal cranial circulation. There have been reports on SlowFlowHD features of the fetal basilar artery [Citation4,Citation5]. We speculated that assessing the basilar artery during the prenatal period is important because of the importance of the basilar artery in humans. This study involved the use of another ultrasound section to observe the basilar artery before delivery. Therefore, there are several questions that need to be answered by sonographers, obstetricians and neurologists. (1) Is the basilar artery meaningful for fetal anomalies? (2) What are the most commonly observed associated anomalies? (3) What is the prognosis of fetuses in the presence of an abnormal basilar artery? (4) Whether the basilar artery replaces the cerebral artery in cases of placental insufficiency needs further discussion.
Conclusion
This study demonstrated that the basilar artery can be evaluated during the second trimester via a new transabdominal approach involving slowflow HD.
Authors’ contribution
Zhengfeng Zhu produced the first draft of the manuscript. All authors sought consent from the patient, contributed to revisions of the final manuscript, and approved the final version of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article.
Additional information
Funding
References
- Vasović L, Trandafilović M, Jovanović I, et al. Human basilar artery abnormalities in the prenatal and postnatal period. World Neurosurg. 2013; 79(3–4):1–4. doi:10.1016/j.wneu.2012.06.033.
- Pooh RK, Aono T. Transvaginal power doppler angiography of the fetal brain. Ultrasound Obstet Gynecol. 1996; 8(6):417–421. doi:10.1046/j.1469-0705.1997.08060417.x.
- Qureshi AI, Miran MS, Degenhardt J, et al. Transabdominal insonation of fetal basilar artery: a feasibility study. J Neuroimaging. 2016; 26(2):180–183. doi:10.1111/jon.12324.
- Hata T, Koyanagi A, Yamanishi T, et al. Three-dimensional SlowflowHD for assessment of fetal organ and placental microvasculature. Donald School J Ultrasound Obstet Gynecol. 2022;16(1):4–10. doi:10.5005/jp-journals-10009-1915.
- Hata T, Koyanagi A, Takayoshi R, et al. Fetal peripheral blood vessels and organ microvasculature depicted by SMI and SlowflowHD. Donald School J Ultrasound Obstet Gynecol. 2021;15(3):272–281.
- Dunbar M, Kirton A. Perinatal stroke. Semin Pediatr Neurol. 2019; 32:100767. doi:10.1016/j.spen.2019.08.003.
- Vasović LP, Jovanović ID, Ugrenović SZ, et al. Normal subtypes of the posterior part of the cerebral arterial circle in human fetuses. Surg Neurol. 2008;70(3):287–294. doi:10.1016/j.surneu.2007.06.087.