Abstract
Introduction
Neural tube defects (NTDs) represent a spectrum of heterogeneous birth anomalies characterized by the incomplete closure of the neural tube. In Jordan, NTDs are estimated to occur in approximately one out of every 1000 live births. Timely identification of NTDs during the 18–22 weeks of gestation period offers parents various management options, including intrauterine NTD repair and termination of pregnancy (TOP). This study aims to assess and compare parental knowledge and perceptions of these management modalities between parents of affected children and those with healthy offspring.
Materials and methods
This retrospective case-control study was conducted at Jordan University Hospital (JUH) using telephone-administered questionnaires. Categorical variables were summarized using counts and percentages, while continuous variables were analyzed using mean and standard deviation. The association between exposure variables and outcomes was explored using binary logistic regression. Data analysis was performed using SPSS for Windows version 26 (SPSS Inc., Chicago, IL).
Results
The study sample comprised 143 participants, with 49.7% being parents of children with NTDs. The majority of NTD cases were associated with unplanned pregnancies, lack of folic acid supplementation, and postnatal diagnosis. Concerning parental knowledge of TOP in Jordan, 86% believed it to be legally permissible in certain situations. However, there was no statistically significant difference between cases and controls regarding attitudes toward TOP. While the majority of parents with NTD-affected children (88.7%) expressed a willingness to consider intrauterine surgery, this percentage decreased significantly (to 77.6%) after receiving detailed information about the procedure’s risks and benefits (p = .013).
Conclusions
This study represents the first case-control investigational study in Jordan focusing on parental perspectives regarding TOP versus intrauterine repair of myelomeningocele following a diagnosis of an NTD-affected fetus. Based on our findings, we urge the implementation of a national and international surveillance program for NTDs, assessing the disease burden, facilitating resource allocation toward prevention strategies, and promoting early diagnosis initiatives either by using newly suggested diagnostic biomarkers or early Antenatal ultrasonography.
Introduction
Neural tube defects (NTDs) represent a diverse group of congenital birth anomalies characterized by incomplete closure of the neural tube during embryonic development, typically occurring between the third and fourth weeks of gestation [Citation1]. Among the most prevalent subtypes of NTDs are spina bifida, anencephaly, and encephalocele [Citation1]. The global prevalence of NTDs exhibits wide variability, ranging from 1.2 to 124.1 per 10,000 births, with Eastern Mediterranean countries demonstrating a median prevalence of 21.9 per 10,000 births [Citation2]. In Jordan, while the absence of a comprehensive surveillance system complicates precise estimation, hospital-based studies report incidence rates ranging from 1.1 to 1.4 per 1000 births [Citation3, Citation4]. These variations worldwide likely stem from genetic disparities, environmental influences, and variances in preventative practices to mitigate NTD occurrences [Citation5].
Few studies explored using biomarkers for the noninvasive prenatal screening of NTDs. Proprotein convertase subtilisin/kexin type 9 (PCSK9) demonstrated the diagnostic efficacy of potential NTD biomarkers, as its expression in the spinal cords and placentas was markedly decreased [Citation6]. It may be involved in the etiopathogenesis of open NTDs at the critical steps of fetal neuronal differentiation, and PCSK9 may be used as an additional biomarker for the screening of NTDs [Citation7].
In our unit, antenatal ultrasonography serves as the primary diagnostic tool for NTDs, typically conducted between 18 and 22 weeks of gestation [Citation5]. The multifactorial etiology of NTDs and the decline in prevalence rates globally are attributed to interventions such as folic acid supplementation and enhanced antenatal screening. Early diagnosis informs management decisions, including the option of termination of pregnancy (TOP) in jurisdictions where legal provisions permit [Citation5]. For cases of myelomeningocele, an NTD subtype, intrauterine or postnatal repair offers alternative management strategies [Citation8]. Intrauterine repair gained prominence following the pivotal Management of Myelomeningocele Study (MOMS) published in 2011 [Citation9], which demonstrated superior outcomes in motor function and reduced complications such as Arnold Chiari II malformation and hindbrain herniation at 30 months compared to traditional postnatal repair, thus diminishing the necessity for shunt placement.
Diverse parental perspectives regarding optimal management modalities for children with NTDs are documented in the literature. Studies from Poland and Saudi Arabia reveal varying attitudes, with preferences ranging from a majority favoring in utero surgeries to significant proportions advocating for pregnancy termination upon early diagnosis of NTDs [Citation10, Citation11]. Yet, no prior investigation has explored parental perspectives on TOP and intrauterine myelomeningocele repair within the Jordanian context. This study addresses this gap, undertaking the first case-control examination in Jordan to compare parental viewpoints between those caring for children with NTDs and those with healthy offspring. Throughout this paper, "abortion" and "termination of pregnancy (TOP)" are used interchangeably.
Methodology
Design and settings
This case-control study was conducted at Jordan University Hospital (JUH) in Amman, Jordan. Cases included parents of children diagnosed with a NTD at JUH between 2010 and 2022, while controls consisted of parents of children born without NTDs via uncomplicated vaginal delivery at JUH during the same timeframe. Parents’ contact details were obtained from JUH’s electronic medical records. NTDs were defined as any live newborn presenting with spina bifida, encephalocele, myelomeningocele, or meningocele, regardless of gestational age at birth.
A simple random sample method was used. The (EpiCalc 2000) program was used to calculate the sample size. A minimum sample size of 143 participants for both arms was calculated for a 95% confidence level, 80% power, and a 5% alpha error level.
This study received approval from the Institutional Review Board (IRB) at JUH (10/2023/28293).
Data collection
An interview-administered survey (questionnaire) was developed by the research team to gather data from both cases and controls. Participants were contacted via phone calls, and verbal consent was obtained before proceeding with the survey. Parents who did not respond to phone calls, declined to participate, or were under 18 years old at the time of their child’s birth were excluded. The survey (questionnaire) covered four main areas: demographic characteristics and obstetric history, perception toward TOP, current child health and functioning, and perception toward intrauterine myelomeningocele repair. The survey items were adapted from existing literature, translated into Arabic, and subjected to back-translation by a linguistic expert. A pilot study involving 10 participants ensured clarity of questions and uniformity in data collection procedures.
Demographic characteristics and obstetric history: Questions encompassed the educational level of the responding parent, residential area, parity, maternal antenatal care utilization, and history of periconceptional folic acid supplementation.
Perception toward termination of pregnancy: Parents were queried about their willingness to consider pregnancy termination in the event of an early NTD diagnosis, along with reasons for their decision. Additionally, their awareness and perceptions of TOP laws in Jordan were assessed.
Current child health and functioning: Parents of children with NTDs provided information on their child’s vital status, timing of NTD diagnosis, prior knowledge of NTDs, consideration of TOP, and assessment of their child’s cognitive and physical capabilities.
Perception toward intrauterine myelomeningocele repair: Parents of children with NTDs indicated their likelihood of opting for intrauterine surgery following a myelomeningocele diagnosis, both before and after receiving detailed information about the procedure’s benefits and risks. Additionally, parents were asked to identify their preferred management approach in the event of an antenatal NTD diagnosis.
Data analysis
Survey data were entered into an Excel spreadsheet, cleaned, and coded. Missing data were obtained through follow-up phone calls. Coded data were then imported into SPSS V26 (SPSS Inc., Chicago, IL) for statistical analysis. Descriptive statistics, including frequencies and percentages, were computed for respondents’ demographics, knowledge, attitudes toward abortion, and NTD patients’ health status.
A multivariate logistic regression model was constructed to identify predictors of attitudes toward abortion. Attitudes toward abortion were quantified as a score out of 24, representing the sum of Likert scale responses to six questions. Cronbach’s alpha assessed the internal consistency of this score. Independent variables included parents’ age, educational level, number of children, residential area, and NTD status of their child, chosen based on both literature relevance and expert opinion.
Parents of NTD patients were evaluated for changes in their willingness to pursue intrauterine surgery before and after receiving detailed information about the procedure. McNemar’s test compared pre- and post-explanation attitudes.
Results
The final sample comprised 143 participants, with 49.7% being parents of children diagnosed with NTDs and 50.3% parents of children without NTD history. Most respondents were mothers (83.9%), with an average age of 42.6 years and an average of 2.9 children per parent. The majority of participants (58.8%) had education beyond high school, and the predominant residential area was in central Jordan (89.5%).
Attitudes and knowledge toward termination of pregnancy
outlines participants’ attitudes and knowledge regarding TOP. Regarding hypothetical scenarios, 73.4% of parents would consider abortion in cases of lethal fetal malformations, which decreased to 8.4% for mild malformations causing slight bodily dysfunction. Most parents believed that the decision for abortion should involve both parents (94.4%), and 86% agreed that TOP is legally permissible in specific situations in Jordan. The most common choice for management in the event of an NTD diagnosis at 19 weeks was abortion (42.7%), whereas at 24 weeks, intrauterine surgery was favored by 58.7% of parents.
Table 1. Attitudes and knowledge of cases and controls’ parents toward TOP.
The multivariate logistic regression model () revealed that parents’ education level significantly influenced attitudes toward TOP. Parents with a bachelor’s degree or higher were more likely to hold negative attitudes toward TOP compared to those with lower education levels (p = .021, OR = 0.417).
Table 2. Demographic characteristics and current health status of NTD patients.
Current status of NTD patients
provides insights into the current status of NTD patients. Approximately, 91.5% of patients were alive at the time of data collection, with females constituting 59% of the cohort. Only 14% of parents were aware of NTDs before pregnancy, and 24% were offered abortions during their affected pregnancy. Although nearly half of the pregnancies were planned, only 20% of parents reported preconceptional folic acid supplementation. The majority of NTD patients (91.5%) had spina bifida, with approximately 72% also presenting hydrocephalus. Most parents described their children’s cognitive function as "normal," and 46.2% reported wheelchair use. The majority (61.6%) rated their child’s medical care as satisfactory or excellent.
Table 3. Demographics and health status of children with NTDs.
Antenatal detection and preferences for pregnancy termination
illustrates that less than 50% of NTD cases in Jordan are detected antenatally, with only 45% of hydrocephalus cases diagnosed prenatally. reveals that 46.3% of parents would be likely or highly likely to opt for abortion if NTD diagnosis occurred before 19 weeks of gestation, decreasing to 29.6% at 24 weeks. The primary reason for considering abortion was to prevent the child’s suffering, cited by 33 parents, while opposition to abortion on religious grounds was the major reason for choosing against it.
Figure 1. Time of diagnosis for NTDs in affected patients. Perception of parents of NTD children toward TOP and intrauterine surgery.
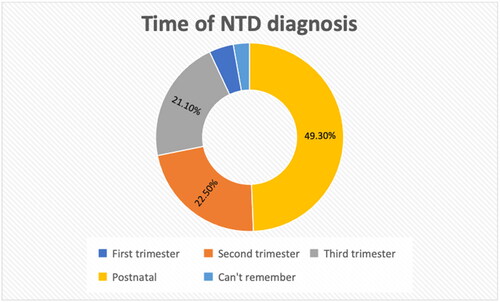
Table 4. Perception of parents of NTD children toward TOP and intrauterine surgery.
Perception toward intrauterine surgery
Initially, 88.7% of parents believed intrauterine surgery was possible for their NTD-affected child. However, after receiving information about the procedure’s risks and benefits, this percentage dropped to 77.6%, as shown by McNemar’s test (p = .013).
Discussion
This study aimed to assess Jordan’s standing regarding NTDs and understand parents’ perspectives on management options. Factors influencing parental decision-making included religious beliefs and educational levels. While there were no significant differences in attitudes toward TOP between cases and controls, religion significantly influenced decisions. Most parents favored abortion in severe cases but were less inclined toward milder malformations, with educational level affecting these attitudes. Antenatal diagnosis rates were suboptimal, often resulting from unplanned pregnancies and lack of folic acid supplementation. Interest in intrauterine repair was evident but tempered by concerns about maternal and fetal risks.
Termination of pregnancy
TOP decisions are multifaceted, and influenced by social, psychological, and legal factors. In Jordan, religious and legal considerations add complexity [Citation12,Citation13]. Although the law criminalizes abortion, Islamic teachings permit it under certain conditions, leading to discrepancies in public understanding [Citation14, Citation15]. While the majority favored TOP for severe malformations, attitudes varied based on educational level [Citation16]. Higher education correlated with less inclination toward TOP, possibly due to better access to information and resources [Citation16]. Contrary to some literature, no significant difference was found between parents of children with NTDs and controls, suggesting shared cultural influences outweigh individual experiences.
Current status of NTD patients
Delayed or missed antenatal diagnoses were common, reflecting gaps in prenatal care and awareness. Unplanned pregnancies and inadequate folic acid supplementation contribute to late diagnoses, limiting parental choices [Citation17]. Most parents desired early diagnosis, highlighting the need for improved screening programs and education. Religious and cultural beliefs strongly influenced decisions, underscoring the importance of culturally sensitive counseling and support services.
Intrauterine repair of myelomeningocele
Interest in intrauterine repair was high but tempered by concerns about risks. Lack of familiarity with the procedure and its outcomes contributed to apprehension. Future research and education efforts should address parental concerns and promote evidence-based decision-making. Establishing a national surveillance program for NTDs can inform policy and resource allocation, enhancing prevention and early diagnosis efforts.
Conclusions
This study sheds light on the complexities of NTD management in Jordan, highlighting the interplay of cultural, religious, and educational factors. It underscores the need for comprehensive support services, improved prenatal screening, and culturally sensitive counseling to empower parents in decision-making. Establishing clear guidelines and resources for NTD management can mitigate suffering and improve outcomes for affected families.
Consent form
Informed consent was signed by each participant after a clear understanding of the study objective.
Acknowledgements
Limitations: NTD is an uncommon anomaly. Minor cases can be missed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available upon request.
Additional information
Funding
References
- ten Donkelaar HJ, Lammens M, Hori A. Clinical neuroembryology: development and developmental disorders of the human central nervous system. Netherlands: Springer; 2006.
- Zaganjor I, Sekkarie A, Tsang BL, et al. Describing the prevalence of neural tube defects worldwide: a systematic literature review. PLOS One. 2016;11(4):1. doi: 10.1371/journal.pone.0151586.
- Masri A. Neural tube defects in Jordan: a hospital based study. J Pediatr Neurol. 2015;4(4):245–8. doi: 10.1055/s-0035-1557337.
- Neural tube defects: overview of prenatal screening, evaluation, and pregnancy management – UpToDate; 2023. Available from: https://0l10hcqq6-y-https-www-uptodate-com.ju.proxy.coe-elibrary.com/contents/neural-tube-defects-overview-of-prenatal-screening-evaluation-and-pregnancy-management?source=history_widget#H1944028399
- Yamashiro KJ, Farmer DL. Fetal myelomeningocele repair: a narrative review of the history, current controversies and future directions. Transl Pediatr. 2021;10(5):1497–1505. doi: 10.21037/tp-20-87.
- Erol SA, Tanacan A, Firat Oguz E, et al. A comparison of the maternal levels of serum proprotein convertase subtilisin/kexin type 9 in pregnant women with the complication of fetal open neural tube defects. Congenit Anom. 2021;61(5):169–176. doi: 10.1111/cga.12432.
- An D, Wei X, Li H, et al. Identification of PCSK9 as a novel serum biomarker for the prenatal diagnosis of neural tube defects using iTRAQ quantitative proteomics. Sci Rep. 2015;5(1):17559. doi: 10.1038/srep17559.
- Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1004. doi: 10.1056/NEJMoa1014379.
- Koszutski T, Kawalski H, Kudela G, et al. Babies with myelomeningocele in Poland: parents’ attitudes on fetal surgery versus termination of pregnancy. Childs Nerv Syst. 2009;25(2):207–210. doi: 10.1007/s00381-008-0653-1.
- Babgi MA, Al-Jifree HM, AlShehri OA, et al. Awareness of risk factors and preventive measures for neural tube defects: perception towards pregnancy termination in the Saudi population. J Neonatal Perinatal Med. 2019;12(2):195–201. doi: 10.3233/NPM-17165.
- Blencowe H, Kancherla V, Moorthie S. Estimates of global and regional prevalence of neural tube defects for 2015: a systematic analysis. Ann N Y Acad Sci. 2018;1414(1):31–46. doi: 10.1111/nyas.13548.
- Johnson CY, Honein MA, Flanders WD, et al. Pregnancy termination following prenatal diagnosis of anencephaly or spina bifida: a systematic review of the literature. Birth Defects Res A Clin Mol Teratol. 2012;94(11):857–863. doi: 10.1002/bdra.23086.
- Legislator. قانون العقوبات الأردني مع كامل التعديلات حتى 2023 .حُماة الحق- محامي الأردن; [ci2017 [cited 2023 Sep 17]. Available from: https://jordan-lawyer.com/2017/04/05/jordan-criminal-law/
- Jordan. United States Department of State; 2023 [cited 2023 Sep 17]. Available from: https://www.state.gov/reports/2022-report-on-international-religious-freedom/jordan/
- Alnaami IM, Alayad EG. Review on myelomeningocele management and its current status in Saudi Arabia. Neurosciences. 2019;24(1):5–10. doi: 10.17712/nsj.2019.1.20180169.
- Jorde LB, Carey JC, Bamshad MJ. Medical genetics. 5th ed. Salt Lake City (UT): Elsevier; 2015.
- Bitzer J, von Stenglin A, Bannemerschult R. Women’s awareness and periconceptional use of folic acid: data from a large European survey. Int J Womens Health. 2013;5:201–213.

