Abstract
Objective: To conduct a systematic review of the evidence in relation to what hearing healthcare professionals do during hearing aid consultations and identifying which behaviours promote hearing aid use and benefit among adult patients.
Design: Searches were performed in electronic databases MEDLINE, EMBASE, CINAHL, PsycInfo, Web of Science, PubMed and Google Scholar. The Crowe Critical Appraisal Tool and Melnyk Levels of Evidence were used to assess quality and level of evidence of eligible studies. Behaviours of hearing healthcare professionals were summarised descriptively.
Study Sample: 17 studies met the inclusion criteria.
Results: Twelve studies described behaviours of audiologists and five studies were intervention studies. Audiologists were typically task- or technically-oriented and/or dominated the interaction during hearing aid consultations. Two intervention studies suggested that use of motivational interviewing techniques by audiologists may increase hearing aid use in patients.
Conclusions: Most studies of clinicians' behaviours were descriptive, with very little research linking clinician behaviour to patient outcomes. The present review sets the research agenda for better-controlled intervention studies to identify which clinician behaviours better promote patient hearing aid outcomes and develop an evidence base for best clinical practice.
Introduction
The World Health Organization estimates that 328 million adults globally have a hearing loss greater than 40 dBHL in the better ear (WHO Citation2012). Hearing aids are the primary treatment for hearing loss (Laplante-Lévesque, Hickson, and Worrall Citation2010), yet 24% of the people given a hearing aid(s) do not use them (Hartley et al. Citation2010). Besides waste of resources, non-use of hearing aids could impact on people with hearing loss and their families and friends in terms of unaddressed difficulties in communication, social isolation and reduced mental well-being (Pronk, Deeg, and Kramer Citation2013; Scarinci, Worrall, and Hickson Citation2008; Vas, Akeroyd, and Hall Citation2017).
McCormack and Fortnum (Citation2013) identified various reasons for non-use, including hearing aids being uncomfortable, difficulty handling hearing aids and patients’ attitudes towards hearing loss and hearing aids (for example; not recognising a need for a hearing aid or stigma of hearing aids). McCormack and Fortnum (Citation2013) also highlighted the important role of audiologists in supporting and counselling patients to promote hearing aid use.
An emerging body of evidence supports McCormack and Fortnum’s (Citation2013) assertion that hearing healthcare professionals can exert an important impact on patient outcomes. Kochkin (Citation2000) found that patients who did not use their hearing aids cited hearing healthcare professional-related factors including “poor services provided” and “oversold expectation”. A 2010 MarkeTrack survey found that characteristics of the hearing healthcare professional (including knowledge, professionalism, empathy, creation of realistic expectations and explanations about maintenance of hearing aids) and patient ratings of the quality of the fitting process were positively correlated with patients’ hearing aid use, benefit and satisfaction (Kochkin et al. Citation2010). Qualitative studies reported that patients value interaction with their audiologists and that interaction with audiologists may help patients get used to using hearing aids (Dawes, Maslin, and Munro Citation2014) and motivated patients to use their hearing aids (Aazh Citation2016b). A systematic review of determinants of hearing aid outcomes highlighted the need to explore the dynamics of the patient-hearing healthcare professionals clinical interactions to facilitate patient outcomes (Knudsen et al. Citation2010).
Despite indications that the clinical interaction may be an important factor in promoting hearing aid use and benefit, a Cochrane review of interventions to improve hearing aid use by Barker et al. (Citation2014) found no effect of self-management support and/or service delivery interventions on hearing aid use in adult patients. However, this review included only randomised controlled trials and quasi-randomised trials up to 2013. More recently, Aazh and Moore (Citation2017) described the key content of seven intervention studies to improve hearing aid use between 2000 and 2016. Aazh and Moore (Citation2017) found the interventions were focused on education of patients about hearing aid use and communication strategies. Aazh and Moore (Citation2017) did not find any effect of educational interventions on hearing aid use. However, as with Barker et al.’s review, Aazh and Moore (Citation2017) included only randomised trials. Although randomised controlled trials are the “gold standard” in clinical trials, difficulty with some aspects of design (for example; randomization may not be feasible), may make research designs other than randomised controlled trials the only practical option to provide an evidence base for clinical guidelines.
Following their 2014 Cochrane review, Barker, Munro, De Lusignan (Citation2015) surveyed adult patients with hearing loss, researchers and hearing healthcare professionals to identify behaviours of hearing healthcare professionals that might help people manage hearing loss. The patients, researchers and clinicians in this study identified 16 hearing healthcare professional-related behaviours, including using open-ended questions, using lay-terms, being empathetic and addressing the individual needs of patients. The efficacy of these behaviours in promoting hearing aid use and benefit remains to be tested.
Although little is known about the link between behaviours of hearing healthcare professionals and hearing aid outcomes, there is evidence outside audiology showing that healthcare professionals’ behaviours positively impact on patient outcomes. In their meta-analysis of studies investigating the association between healthcare providers’ communication behaviours and patient treatment adherence, Zolnierek and DiMatteo (Citation2009) found that the risk of non-adherence was 19% higher in patients of healthcare providers with poor communication behaviours. Shay and Lafata (Citation2015) similarly found that 54% of the studies they included in their review reported positive effects of shared decision making on patient-reported outcomes including satisfaction. The associations between communication behaviours with positive patient outcomes could be extrapolated to hearing aid use and benefit.
Identifying particular behaviours of hearing healthcare professionals that facilitate hearing aid outcomes is important to promote effective management of hearing problems in adult patients, minimise waste of resources and support the development of evidence-based audiological education and training programs. Therefore, the purpose of this systematic review was to identify, summarise and assess the quality of evidence; describing behaviours of hearing healthcare professionals during hearing aid consultations with adult patients and identifying which behaviours promote hearing aid use and benefit by adult patients.
Methods
Search strategy
A search of databases MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Literature (CINAHL), PsycInfo, Web of Science, PubMed and Google Scholar was conducted. The search was performed from the earliest possible date up to and including August 2018. Databases were searched without restriction on language or location. Searches were performed using free text terms. The free text terms were categorised in three blocks based on the research questions; “behaviour” (block 1), “hearing healthcare professional” (block 2) and “hearing aid” (block 3) (See ). To ensure all the possible words were included in this review, experienced research librarians assisted with preparation of the word lists. Reference lists from shortlisted papers were searched for additional potentially eligible articles.
Table 1. Search terms and Boolean operator used: Group terms combined by “AND”.
Participants and setting
Studies were included if they described clinical consultations involving patients aged 18 years or above with hearing healthcare professionals including otolaryngologists, audiologists or hearing aid providers who prescribe and dispense hearing aids in any practice setting. The various types of hearing healthcare professionals were included to capture the range of professionals involved in the delivery of hearing services in different countries. Studies conducted with children or involving parents were excluded.
Study characteristics
Descriptive studies were included if they included direct observations of consultations between hearing healthcare professionals and adult patients. Only consultations that involved a discussion of hearing rehabilitation options were included. This included a discussion of hearing rehabilitation options following hearing assessment appointments including fitting appointments or post-fitting appointments. Studies that described the behaviours of hearing healthcare professionals during history-taking or during describing hearing assessment results were excluded. Hearing healthcare professionals’ behaviours were defined as “anything a person does in response to internal or external events” (Michie, Atkins, and West Citation2014, page 234). This included anything that hearing healthcare professionals did in terms of their verbal and/or non-verbal communication behaviours. Studies describing the use of web-based or other remote forms of communication, implantable devices, student clinicians or simulated patients were excluded. Studies of consultations between hearing healthcare professionals and family and friends of patients were also excluded.
Randomised controlled trials (RCTs) and single group design studies that evaluated the effect of interventions that involved face-to-face hearing healthcare professional-patient clinical consultations and measured patient hearing aid outcomes were included. Outcomes of interest included hearing aid use and benefit. Hearing aid use included either data logged hours of hearing aid use or self-reported hearing aid use. Measures of subjective hearing aid benefit included patient self-report measures of hearing aid benefit, satisfaction and hearing handicap reduction. Studies that measured outcomes related to patients’ recall of information pertaining to hearing test results or measures of aided speech recognition were excluded. Other outcomes, for example, mental and psychosocial well-being, were not reported in the present review. Intervention studies that measured hearing healthcare professional-related outcomes only (including intervention fidelity, satisfaction or attitude of hearing healthcare professionals) were excluded.
Studies describing rehabilitation for tinnitus, balance or cochlear implantation were excluded. Editorials, expert opinions or study protocols were excluded. Studies that were not published in peer-reviewed journals were also excluded.
Review procedure
The first author reviewed all the article titles to exclude those that were clearly ineligible. Full text versions of articles were obtained when the abstract reported research involving clinician-patient consultations. All the potentially relevant full-text articles were reviewed independently by the co-author (Dawes). Any disagreement between the two reviewers was resolved by discussion with other authors (Munro and Armitage). The process of review and selection of articles for inclusion was recorded and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al. Citation2009).
Data extraction
The first author carried out data extraction using a structured table. The reliability of data extraction was checked by the co-author (Dawes) with discrepancies resolved through discussion with the co-authors (Munro and Armitage). The data extraction table included key information as follows: author, year of publication, country, study design, participants and the key behaviours of hearing healthcare professionals that were identified in each respective study. The key behaviours reported in the present review were reported using the terminology used by the respective authors of each study to describe the behaviours that they had identified. For intervention studies, additional data on the effect size of each intervention on hearing aid use and benefit outcomes were also extracted.
Quality assessment and level of evidence
The Crowe Critical Appraisal Tool (CCAT) (Crowe and Sheppard Citation2011) was used to assess the methodological quality of eligible studies. The Crowe Critical Appraisal Tool was selected because it was developed as a structured tool for evaluation of health research, can be used to appraise studies of various designs and has established validity and reliability (Crowe, Sheppard, and Campbell Citation2011; Crowe and Sheppard Citation2011). It consists of eight categories including; (1) Preliminaries (title, abstract and text), (2) Introduction, (3) Design, (4) Sampling, (5) Data collection, (6) Ethical matters, (7) Results and (8) Discussion. Each category was scored on a scale from 0 to 5 based on appropriateness of methodology and reporting. The total score for each study was considered as “poor quality” (<50%), “moderate quality” (51–74%) and “high quality” (>74%) based on criteria from a previous study with the Crowe Critical Appraisal Tool (Sznitman and Taubman Citation2016).
The level of evidence of each study was also assessed using the Melnyk Levels of Evidence (Melnyk and Fineout-Overholt Citation2011). Level I is the strongest level of evidence on which to base treatment decisions and includes systematic reviews or meta-analyses of RCTs. Level II evidence includes RCTs. Level III refers to controlled trials without randomization. Level IV includes well-designed case-control and cohort studies. Level V includes systematic reviews of descriptive or qualitative studies. Level VI includes single descriptive or qualitative studies and level VII includes expert opinion or reports of expert committees.
The risk of bias was assessed using the Cochrane Back and Neck Group risk of bias criteria (Furlan et al. Citation2015). The Cochrane Back and Neck Group risk of bias criteria consist of 13 criteria with each criterion scored as “yes”, “unclear”, or “no”. A “yes” indicates a low risk of bias (Furlan et al. Citation2009). A study would be rated as having a low risk of bias when at least 50% of Cochrane Back and Neck Group risk of bias criteria are met and the study has no serious flaws (for example, a high participant drop-out rate) (Furlan et al. Citation2009). The Crowe Critical Appraisal Tool, level of evidence and risk of bias ratings were undertaken independently by two reviewers (Ismail and Dawes) with disagreements being resolved through discussion.
Data analysis
The behaviours of hearing healthcare professionals identified in the present review were summarised descriptively. Heterogeneity across studies in study designs prevented quantitative meta-analysis of results from the intervention studies. Therefore, the results of the intervention studies were reported descriptively.
Results
Study selection
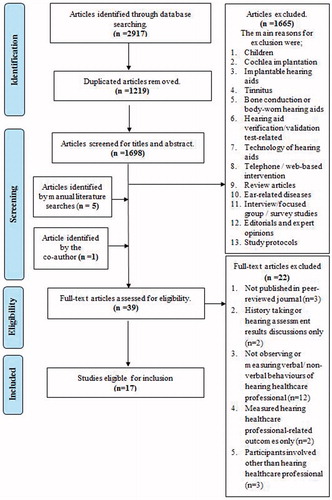
Two thousand nine hundred seventeen potential articles were identified through database searching. 1219 duplicates were identified and removed. The abstracts of 1698 studies were screened, and 1665 articles were discarded due to not meeting the inclusion criteria, leaving 33 potential articles that were assessed for eligibility. Five potential articles were identified by manual searching of the reference list of included articles. One potential article was identified by one of the co-authors (Munro). The full-text versions of 39 potentially eligible articles were retrieved and evaluated for inclusion. 17 of the 39 studies were included in this review. The flow of the literature search and identification process is presented in .
Study characteristics
All 17 studies were set in audiology clinics with seven studies (44%) conducted in Australia (Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ekberg, Hickson, and Grenness Citation2017b; Grenness et al. Citation2015; Meyer et al. Citation2017; Sciacca et al. Citation2017), four (25%) in the United Kingdom (Aazh Citation2016a; Barker, Mackenzie, and De Lusignan Citation2016; Ferguson et al. Citation2016; Pryce et al. Citation2016), three (19%) in the United States (Dockens et al. Citation2017; Nair and Cienkowski Citation2010; Saunders and Forsline Citation2012), one (6%) in Sweden (Naylor et al. Citation2015), one (6%) in Denmark (Hindhede Citation2010) and one (6%) in Norway (Solheim et al. Citation2018). 12 studies observed and described audiologists’ behaviours during discussions about a hearing aid (Barker, Mackenzie, and De Lusignan Citation2016; Dockens et al. Citation2017; Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ekberg, Hickson, and Grenness Citation2017b; Grenness et al. Citation2015; Hindhede Citation2010; Meyer et al.Citation2017; Nair and Cienkowski Citation2010; Pryce et al. Citation2016; Sciacca et al. Citation2017). The remaining five studies were intervention studies that involved face-to-face audiologist-patient clinical consultations and measured patient hearing aid outcomes (Aazh Citation2016a; Ferguson et al. Citation2016; Naylor et al. Citation2015; Saunders and Forsline Citation2012; Solheim et al. Citation2018). The characteristics of all studies are summarised in and (descriptive and intervention studies, respectively).
Table 2. Details of descriptive studies.
Table 3. Details of intervention studies.
Descriptive studies
Nine of the 12 descriptive studies involved audio- or video-recorded post-hearing assessment discussions (Dockens et al. Citation2017; Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ekberg, Hickson, and Grenness Citation2017b; Grenness et al. Citation2015; Meyer et al. Citation2017; Pryce et al. Citation2016; Sciacca et al. Citation2017). Three studies video-recorded hearing aid fitting appointments (Barker, Mackenzie, and De Lusignan Citation2016; Hindhede Citation2010; Nair and Cienkowski Citation2010).
Two studies were rated as “moderate quality” (Crowe Critical Appraisal Tool, score of 58%). The remaining 10 studies were “high quality” (scores from 78 to 95% ()). All studies were rated as level VI according to the Melnyk Levels of Evidence (Melnyk and Fineout-Overholt Citation2011).
Intervention studies
Three of the five intervention studies examined interventions delivered by audiologists targeted at current hearing aid users who under-used and/or reported little benefit from the hearing aid (Aazh Citation2016a; Saunders and Forsline Citation2012; Solheim et al. Citation2018). In the fourth study, new hearing aid users were the population of interest (Ferguson et al. Citation2016). In the remaining study, the effects of audiologist interactions were studied among both experienced and new hearing aid users (Naylor et al. Citation2015).
The Crowe Critical Appraisal Tool scores for quality of methodology ranged from 75 to 100%, all “high quality” (). Four of the studies were rated as having a low risk of bias except for one study according to the Cochrane Back and Neck Group criteria (Furlan et al. Citation2015). The levels of evidence of the intervention studies were Level II, III and IV, according to the Melnyk Levels of Evidence (Melnyk and Fineout-Overholt Citation2011). Three studies were randomised controlled trials (level II), one was a quasi-randomised controlled study (level III) and one was one group pre- and post-test study (level IV).
Hearing healthcare professionals’ behaviours during a hearing aid consultation
Regardless of whether the discussion about a hearing aid followed hearing assessment or hearing aid fitting appointments, audiologists in all 12 descriptive studies were task- or technically-oriented and/or took a dominant role during the clinical consultations (Barker, Mackenzie, and De Lusignan Citation2016; Dockens et al. Citation2017; Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ekberg, Hickson, and Grenness Citation2017b; Grenness et al. Citation2015; Hindhede Citation2010; Meyer et al. Citation2017; Nair and Cienkowski Citation2010; Pryce et al. Citation2016; Sciacca et al. Citation2017). Audiologists were reported to have done most of the talking during clinical interactions (Dockens et al. Citation2017; Doyle Citation1994; Grenness et al. Citation2015). Audiologists were also interpreted as typically being directive in decision making, in that they offered hearing aids and no other hearing rehabilitation options (for example, assistive listening devices or communication training program) (Pryce et al. Citation2016) or offered a limited range of hearing aid cost options (Ekberg, Barr, and Hickson Citation2017a). Rehabilitation options other than hearing aids were only presented when patients rejected hearing aids (Grenness et al. Citation2015).
Examples of task- or technically-oriented behaviour during post-hearing assessment appointments included focusing on introducing the hearing aid with little time discussing patients’ hearing diagnoses (Doyle Citation1994; Ekberg, Grenness, and Hickson Citation2014; Grenness et al. Citation2015), hearing aids being prescribed as a default management option for hearing loss (Doyle Citation1994; Grenness et al. Citation2015; Pryce et al. Citation2016), the content of audiologists’ talk being predominantly about the technical aspects of hearing aids (Doyle Citation1994; Ekberg, Grenness, and Hickson Citation2014; Grenness et al. Citation2015; Meyer et al. Citation2017) with no or limited talk concerning the lifestyle and communication needs of the patient (Ekberg, Grenness, and Hickson Citation2014; Grenness et al. Citation2015; Meyer et al. Citation2017). Audiologists used medical jargon without explaining its meaning (Sciacca et al. Citation2017) and used language that was beyond the literacy level of patients (Nair and Cienkowski Citation2010). Audiologists also performed other tasks while talking to the patients (Ekberg, Hickson, and Grenness Citation2017b).
During hearing aid fitting appointments, audiologists’ interactions were also described as a task- or technically-oriented. The advice and information about hearing aid use provided by audiologists was general (Barker, Mackenzie, and De Lusignan Citation2016; Hindhede Citation2010), with little or no input from the patient (Barker, Mackenzie, and De Lusignan Citation2016). The content of information provided by audiologists was similar across hearing aid fitting consultations (Barker, Mackenzie, and De Lusignan Citation2016; Hindhede Citation2010). The information that audiologists provided related to acclimatisation to hearing aids and technical aspects of hearing aids (Hindhehe Citation2010).
Behaviours of hearing healthcare professionals and hearing aid outcomes
Five studies were identified that included interventions employing: motivational engagement (Ferguson et al. Citation2016), motivational interviewing (Aazh Citation2016a; Solheim et al. Citation2018), diagnostic and interactive narratives (Naylor et al. Citation2015) and performance perceptual counselling (Saunders and Forsline Citation2012) in relation to hearing aid use and benefit outcomes.
In chronological order, Saunders and Forsline (Citation2012) examined the effectiveness of informational counselling only versus informational plus performance perceptual counselling on hearing aid use and benefit in 69 adult patients who were dissatisfied with their hearing aids (Saunders and Forsline Citation2012). In informational counselling, patients were counselled about their hearing loss, hearing aids and communication strategies. Performance perceptual counselling involved providing information related to the performance perceptual discrepancy (PPDIS) score of patients (the difference between the measured and patient judgement of their ability to understand speech in noise). Patients who scored negatively on the PPDIS were defined as under-estimating their hearing ability; patients with positive PPDIS scores were judged as over-estimating their hearing ability. It was hypothesized that those who either under-estimated or over-estimated their hearing ability could benefit from performance perceptual counselling. Saunders and Forsline (Citation2012) analysed self-reported hearing aid use and benefit questionnaires. There was no significant change in hearing aid use or benefit in either the informational or performance perceptual counselling groups at 8 or 10 weeks post fitting.
Naylor et al. (Citation2015) evaluated the effect of audiologists’ interactions on patients’ hearing aid use and benefit. Naylor et al. described the clinical interaction as embodying a “narrative” that may impact on patient outcomes. Adult patients (24 experienced and 16 new hearing aid users) were randomized to an “interactive” narrative or a “diagnostic” narrative alternately. In the interactive narrative, patients were involved in decision making with their audiologists and were led to believe that their hearing aid was set-up to their preferences. In the diagnostic narrative, patients were passive, and no input or response was required from them. In both conditions, hearing aids were adjusted based on each patient’s hearing thresholds so that the hearing aids were acoustically identical across both narratives. Hearing aid benefit was measured at two weeks post-intervention using self-report questionnaires. Results were reported in terms of the patient’s “preferred” interaction (diagnostic or interactive). 20 of the 24 experienced and 14 of the 16 new hearing aid users preferred either the interactive narrative or the diagnostic narrative. Patients without a preference were excluded from analysis. Among experienced hearing aid users, there were better ratings of hearing aid benefit and reduced hearing disability (Cohen’s d = 0.48; Hearing Aid Performance Questionnaire (HAPQ) (Gatehouse, Naylor, and Elberling Citation2006), d = 0.43; Hearing Handicap Inventory for the Elderly (HHIE) (Ventry and Weinstein Citation1982), and d = 0.68; International Outcome Inventory for Hearing Aids (IOI-HA) (Cox and Alexander Citation2002)) in the preferred versus the non-preferred narrative. In the smaller group of new hearing aid users, there were higher ratings of hearing aid benefit and reduced hearing disability for the preferred versus the non-preferred narrative (Cohen’s d = 0.30; HAPQ (Gatehouse, Naylor, and Elberling Citation2006), d = 0.45; HHIE (Ventry and Weinstein Citation1982)), but no difference between narratives for the IOI-HA (Cox and Alexander Citation2002).
Ferguson et al. (Citation2016) trained two out of five study audiologists to deliver “Line, Box and Circle” motivational tools. The “Line, Box and Circle” was developed by the Ida Institute to be used by audiologists to encourage patients to engage with their own audiological management (Clark Citation2010). For example, patients were asked questions related to their motivation to improve hearing. The motivational tools were delivered during fitting consultations to first-time hearing aid patients. Ferguson et al. found that although adult patients who received the motivational tools reported greater self-efficacy in managing their hearing aid following hearing assessment and greater engagement with their audiologist during hearing aid fitting, there was no significant difference between intervention and control groups in hearing aid use measured via data logging, self-reported hearing aid use, benefit or satisfaction at 10 weeks follow-up.
Aazh (Citation2016a) explored the feasibility of a full-scale randomised controlled trial of motivational interviewing on hearing aid use. This feasibility study was conducted with 37 adult hearing aid users who used their hearing aid fewer than four hours per day (Aazh Citation2016a). Patients were randomized into two groups; standard consultation from an audiologist (standard care) or a combination of standard consultation and motivational interviewing (motivational interviewing group). In the motivational interviewing group, the audiologist discussed personal motivation to use hearing aids with the patient based on motivational interviewing principles (Miller and Rollnick Citation2012). Adult patients who received motivational interviewing (n = 20) showed greater hearing aid use (7 ± 3.7 hours per day) compared to the standard care group (4 ± 3.6 hours per day; large effect size Cohen’s d = 0.82) according to the hearing aid data logging. There was no significant difference in hearing aid questionnaire scores IOI-HA (Cox and Alexander Citation2002), International Outcome Inventory for Hearing Aid for the Significant Other (IOI-HA-SO)(Noble Citation2002), Client Oriented Scale of Improvement (COSI) (Dillon, James, and Ginis Citation1997) or Glasgow Hearing Aid Benefit Profile (GHABP) (Gatehouse Citation1999) at one month post-intervention.
In 2018, Solheim et al. investigated the effectiveness of motivational interviewing provided by an audiologist to 47 adult patients, who attended six-month follow-up appointment and used their hearing aid(s) fewer than 90 minutes per day (measured using data logging). Based on motivational interviewing principles (Miller and Rollnick Citation2013), adult patients’ experiences and personal obstacles to hearing aid use were discussed for 30 minutes. Hearing aid use was measured using data logging at three months post-intervention. Hearing aid benefit was measured based on informal patient reports of perceived benefit at three months post-intervention. Solheim et al. found that hearing aid use increased from 21 minutes per day on average (standard deviation ±29 minutes) at baseline (6 months post-fitting) to 1 hour and 52 minutes per day on average (standard deviation ±1 hour and 40 minutes) at three months post-intervention. Moreover, 21 of 37 (57%) adult patients reported an increase in hearing aid benefit at three months post-intervention.
Discussion
This review sought to understand and clarify the impact of hearing healthcare professionals’ behaviours on patient hearing aid use and benefit. We identified 12 descriptive observational studies and five intervention studies of the impact of changing audiologist-patient interactions on hearing aid use and benefit. Audiologists displayed a limited range of behaviours that did not include any of the behaviours recommended by Barker, Munro, and De Lusignan (Citation2015) including using open-ended questions, using lay-terms, being empathetic and addressing the individual needs of patients. Implications for future interventions and clinical practice are discussed below.
The behaviours of hearing healthcare professionals with adult hearing aid patients during a hearing aid consultation.
A limited range of behaviours is employed by audiologists. The behaviours of audiologists reported in the 12 studies above were characterised by being task- or technically-oriented and/or being led by the audiologist (Barker, Mackenzie, and De Lusignan Citation2016; Dockens et al. Citation2017; Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ekberg, Hickson, and Grenness Citation2017b; Grenness et al. Citation2015; Hindhede Citation2010; Meyer et al. Citation2017; Nair and Cienkowski Citation2010; Pryce et al. Citation2016; Sciacca et al. Citation2017). Although clinical guidelines and researchers recommend that audiologists should engage in shared-decision making, address patients’ individual needs, and engage in patient-centred practice (British Society of Audiology Citation2016; Grenness et al. Citation2015), these behaviours have not typically been reported in relation to audiological practice. Audiologists’ behaviours are consistent with a traditional medical model of impairment that focuses on diagnosis and treatment of disease or impairment rather than addressing the person with the health problem in a more holistic fashion (Bauman, Fardy, and Harris Citation2003). Not attending to the individual psychosocial needs of a patient was identified as a barrier to the development of an effective audiologist-patient relationship (Grenness et al. Citation2014). Failure to attend to individual psychosocial needs may result in failure to impact patients’ attitudes and thoughts concerning hearing aid use and benefit.
It was striking that the behaviours reported by Doyle in 1994 were similar to those reported in studies in the 2000s (for example Ekberg, Grenness, and Hickson (Citation2014) and Grenness et al. (Citation2015)). The behaviours of audiologists have apparently remained similar over the last 20 years. Perhaps, the lack of improvement in rates of hearing aid use and benefit over this time period, despite advances in hearing aid technology might be partially attributable to the persistent use of ineffective behaviour change strategies during audiological consultations. There is a scope to employ additional or alternative behaviour change strategies that might promote hearing aid use and benefit (Barker, Mackenzie, and De Lusignan Citation2016).
The quality and level of evidence of descriptive studies of audiologists’ behaviours included in the present review were moderate or good. A descriptive observational design was appropriate for the aim of describing audiologists’ practice, so the moderate level of evidence is not necessarily a limitation. However, in the majority of the studies, there were limitations regarding methodological quality in relation to sampling. Most studies used convenience sampling to recruit audiologists, which may have resulted in sampling bias. Perhaps, selecting audiologists who were willing to be involved in research resulted in the selection of audiologists with more progressive professional development and practice than is usual.
Behaviours that lead to better hearing aid use and benefit by adult patients.
The intervention studies were the only studies that allowed any inference to be made about causal links between audiologist behaviours and outcomes. The present review identified five intervention studies that investigated the effects of interventions provided during audiologist-patient interactions on patient hearing aid outcomes. These interventions included performance perceptual counselling (Saunders and Forsline Citation2012), diagnostic and interactive narratives (Naylor et al. Citation2015), motivational tools (Ferguson et al. Citation2016) and motivational interviewing (Aazh Citation2016a; Solheim et al. Citation2018). Three of the five intervention studies reported a significant effect of the intervention on hearing aid use and benefit. Aazh (Citation2016a) and Solheim et al. (Citation2018) reported a positive impact of the motivational interviewing on hearing aid use measured via data-logging at one-month post-intervention (Aazh Citation2016a) and at three-months post-intervention (Solheim et al. Citation2018) on adult patients, who under-used their hearing aids. Naylor et al. (Citation2015) found differences in self-reported hearing aid benefit between preferred and non-preferred narratives in experienced and first-time hearing aid users.
Aazh (Citation2016a) and Solheim et al. (Citation2018) suggested that incorporating an individualised approach to motivate hearing aid use into routine clinical interactions might promote hearing aid use and benefit. However, there were several limitations in both studies. Aazh’s study was a feasibility study rather than a fully powered randomised control trial. Solheim et al.’s study was a pre- and post-test study without a control group. The small sample size in both studies raises uncertainty about the precision and reliability of the results. The lack of a control group in Solheim et al.’s study makes it difficult to draw conclusions about the impact of the motivational intervention. Hearing aid outcomes were limited to one-month and three-month post-intervention with no long-term outcomes were assessed, so it is unknown whether the benefits of intervention persist.
Naylor et al. (Citation2015) suggested that clinical “narratives” provided by audiologists influence hearing aid benefit. According to Naylor et al., each hearing aid user had his or her own preference for the style of clinical interaction during hearing aid fitting and that preference impacted upon hearing aid outcomes. However, Naylor et al.’s (Citation2015) study also involved a small sample size and short-term outcome measures two weeks after each intervention. Additional clinical trials testing the effectiveness of motivational interviewing, clinical narratives and other potential audiologist behaviours that may promote hearing aid outcomes are needed.
Clinical guidelines and researchers recommend particular behaviours and interactional styles (British Society of Audiology Citation2016; Grenness et al. Citation2015), including shared-decision making and patient-centred practice. However, without controlled experimental studies looking at the impact of these behaviours on patient hearing aid outcomes, it would be premature to draw the conclusion that behaviours of audiologists promote hearing aid use and benefit. Current clinical recommendations appear to be based only on expert opinion, which is the weakest level of evidence (Melnyk and Fineout-Overholt Citation2011). Exactly how audiologists can best promote hearing aid use and benefit in adult patients via their clinical interactions has yet to be established. This represents a yawning gap in knowledge that is not unique to audiology (Shay and Lafata Citation2015; Zolnierek and DiMatteo Citation2009).
Given that previous review found that the non-use of hearing aids is partly dependent on the thoughts and attitudes of people with hearing loss (McCormack and Fortnum Citation2013), it is important to test whether clinical interactions with audiologists could change the thoughts and attitudes of patients and promote hearing aid use and benefit. While knowledge (about hearing aid care and its maintenance) may be necessary (Aazh and Moore Citation2017), knowledge alone may not be sufficient to achieve the behaviour change required to sustain hearing aid use and benefit. Creating a behavioural plan for hearing aid use (i.e. an “action plan”) may be important to translate motivation to use a hearing aid into consistent hearing aid use (Sawyer et al. Citationin press); evidence suggests that patients are already highly motivated to wear a hearing aid when present in audiology clinics (e.g. Armitage et al. Citation2017; Sawyer et al. Citationin press). The challenge is translating good intentions into behaviour. Future behaviour change-based interventions for audiologists to promote the use of behaviour change strategies targeting “volitional processes” (i.e. those that translate motivation into action) in adult patients are needed.
In future, research to supply the evidence to support clinical practice, interventions to change the practice of audiologists in the clinic should be clearly described in a way that would allow interpretation and replication. Use of standard methods of describing the content of interventions, for example, the Behaviour Change Techniques Taxonomy version 1 (Michie et al. Citation2013) alongside standard outcome measures including objective measures of hearing aid use and validated self-reported hearing aid questionnaires would facilitate comparison of results across studies and populations. Intervention studies would provide an ideal paradigm for testing, which behaviours are most effective in promoting hearing aid use and establishing the utility of skills training programs for audiologists.
Intervention studies should be robustly designed (e.g. by including active control groups to minimise the impact of research participation effects and double-blind assessment of outcomes to minimise bias). Intervention studies should also include a process evaluation in order to understand contextual factors that impact the effectiveness of the intervention (Moore et al. Citation2015). For example, Aazh (Citation2016b) conducted interviews with participants to understand factors that may influence outcomes in a study of motivational interviewing to promote hearing aid use.
Strengths and limitations of the literature and presence review
The findings of this review were limited by the quality of the study design of the available studies. Most literature was descriptive, and no inferences about which behaviours are effective in promoting outcomes were possible on the basis of these studies. Secondly, because audiologists were the only hearing healthcare professional group found in this review, we cannot infer whether the same behaviours are employed by other hearing healthcare professionals.
The average age of patients involved in the majority of studies was around 70 years (Aazh Citation2016a; Doyle Citation1994; Ekberg, Barr, and Hickson Citation2017a; Ekberg, Grenness, and Hickson Citation2014; Ferguson et al. Citation2016; Grenness et al. Citation2015; Meyer et al. Citation2017; Nair and Cienkowski Citation2010; Sciacca et al. Citation2017; Solheim et al. Citation2018) which is typical of first time adult hearing aid users. Findings of these studies may, therefore, be generalizable. The behaviours of audiologists in Australia, the United Kingdom, the United States and Denmark were reported to be similar across studies. However, it is notable that most studies were carried out in the West and it may be that different audiologist behaviours are appropriate for particular cultures and models of hearing health service provision in each country. More international studies of the behaviours of audiologists are needed.
Although hearing aid use was the main outcome measured in the present review and Aazh and Moore’s review, our review question was different from Aazh and Moore. Aazh and Moore (Citation2017) investigated audiological rehabilitation programs that were delivered in a variety of settings (e.g. individual or group session). Our review was restricted to the effect of interventions delivered face-to-face between the hearing healthcare professional and the patient in a clinical setting. Identifying which interventions promote hearing aid use and benefits are important if they are to be integrated into clinical practice.
Despite using five major databases and extensive key terms, a manual search of reference lists of included papers identified four studies that were not identified in the database search. Manual searches are therefore recommended for reviews in audiology, in line with practice in other fields (dermatology, for example (Vassar, Atakpo, and Kash Citation2016)). One article included in the present review (Naylor et al. Citation2015) was identified by a co-author but was not identified in either the database search or the manual search. This paper may have been missed due to use of idiosyncratic terminology (“embodied narrative”). Future systematic reviews might survey clinical and research leaders to identify a broader range of potentially relevant search terms.
Conclusions
The conclusions of the present systematic review are, first, audiologists typically employ a limited range of behaviours that are mostly task- or technically-oriented. Second, there is some evidence from good quality studies that audiologists’ behaviour does impact hearing aid outcomes in adult patients, although the small number of studies precludes identification of which behaviour(s) these include. There is scope to trial additional or alternative behaviours that might promote hearing aid use and benefit. Such behaviours could be tested via well-designed controlled trials, contributing to an evidence base for clinical practice and education. A renewed focus on the impact of human interactions in the clinical management of hearing loss may be beneficial in a clinical practice paradigm that has been dominated by technological advancement.
Declaration of interest
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aazh, H., and B. C. J. Moore. 2017. “Audiological Rehabilitation for Facilitating Hearing Aid Use: A Review.” Journal of the American Academy of Audiology 28:248–260 doi:10.3766/jaaa.16035.
- Aazh, H. 2016a. “Feasibility of Conducting a Randomized Controlled Trial to Evaluate the Effect of Motivational Interviewing on Hearing-Aid Use.” International Journal of Audiology 55 (3): 149–156. doi:10.3109/14992027.2015.1074733.
- Aazh, H. 2016b. “Patients' Experience of Motivational Interviewing for Hearing Aid Use: A Qualitative Study Embedded Within a Pilot Randomised Controlled Trial.” Journal of Phonetics and Audiology 2 (1):1–13. doi:10.4172/2471-9455.1000110.
- Armitage, C. J., D. Lees, K. Lewis, and K. J. Munro, 2017. “Preliminary Support for a Brief Psychological Intervention to Improve First-Time Hearing Aid Use Among Adults.” British Journal of Health Psychology 22: 686–700. doi:10.1111/bjhp.12244.
- Barker, F., E. Mackenzie, and S. De Lusignan. 2016. “Current Process in Hearing-Aid Fitting Appointments: An Analysis of Audiologists’ Use of Behaviour Change Techniques Using the Behaviour Change Technique Taxonomy (v1).” International Journal of Audiology 55 (11): 643–652. doi:10.1080/14992027.2016.1197425.
- Barker, F., E. Mackenzie, L. Elliott, S. Jones, and S. De Lusignan. 2014. “Interventions to Improve Hearing Aid Use in Adult Auditory Rehabilitation (Review).” Cochrane Database of Systematic Reviews (7): CD010342. doi:10.1002/14651858.CD010342.pub3
- Barker, F., K. J. Munro, and S. De Lusignan. 2015. “Supporting Living Well with Hearing Loss: A Delphi Review of Self-Management Support.” International Journal of Audiology 54 (10): 691–699. doi:10.3109/14992027.2015.1037019.
- Bauman, A., H. Fardy, and H. Harris. 2003. “Getting it Right; Why Bother with Patient Centred Care?” Medical Journal of Australia 179 (5): 253–256.
- British Society of Audiology. 2016. “Practice Guidance Common Principles of Rehabilitation for Adults in Audiology Services Date.” [Accessed date: 1st January 2018] http://www.thebsa.org.uk/wp-content/uploads/2016/10/Practice-Guidance-Common-Principles-of-Rehabilitation-for-Adults-in-Audiology-Services-2016.pdf
- Clark, J. G. 2010. “The Geometry of Patient Motivation Circles, Lines, and Boxes.” Audiology Today 22: 32–40.
- Cox, R. M., and G. C. Alexander. 2002. “The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric Properties of the English Version: El Inventario International de Resultados para Auxiliares Auditivos (IOI-HA): propiedades psicometricas de la version en ingles.” International Journal of Audiology 41 (1): 30–35. doi:10.3109/14992020209101309.
- Cox, R. M., and G. C. Alexander. 2001. “Validation of the SADL Questionnaire.” Ear and Hearing 22: 151–160. doi:10.1097/00003446-200104000-00008.
- Cox, R. M., and G. C. Alexander. 1995. “The Abbreviated Profile of Hearing Aid Benefit.” Ear and Hearing 16: 176–186. doi:10.1097/00003446-199504000-00005.
- Crowe, M., and L. Sheppard. 2011. “A Review of Critical Appraisal Tools Show They Lack Rigor: Alternative Tool Structure is Proposed.” Journal of Clinical Epidemiology 64 (1): 79–89. doi:10.1016/j.jclinepi.2010.02.008.
- Crowe, M., L. Sheppard, and A. Campbell. 2011. “Comparison of the Effects of Using the Crowe Critical Appraisal Tool Versus Informal Appraisal in Assessing Health Research: A Randomised Trial.” International Journal of Evidence-Based Healthcare 9 (4): 444–449. doi:10.1111/j.1744-1609.2011.00237.x.
- Dawes, P., M. Maslin, and K.J. Munro. 2014. “‘Getting used to’” Hearing Aids from the Perspective of Adult Hearing-Aid Users.” International Journal of Audiology 53 (12): 861–870. doi:10.3109/14992027.2014.938782.
- Dillon, H., A. James, and J. Ginis. 1997. “Client Oriented Scale of Improvement (COSI) and its Relationship to Several Other Measures of Benefit and Satisfaction Provided by Hearing Aids.” Journal of the American Academy of Audiology 8: 27–43.
- Dockens, A. L., M. L. Bellon-harn, E.S. Burns, V. Manchaiah, and O. Hinojosa. 2017. “Examination of an Audiologist’ s Response to Patient’s Expression of Symptoms: A Pilot Study.” Journal of Audiology and Otology 21 (2): 115–119. doi:10.7874/jao.2017.21.2.115.
- Doyle, J. 1994. “Initial Consultations in Hearing Aid Clinics in Australia.” Journal of the American Academy of Audiology 5 (3): 216–225.
- Ekberg, K., C. Barr, and L. Hickson. 2017a. “Difficult Conversations: Talking About Cost in Audiology Consultations with Older Adults.” International Journal of Audiology 56 (11): 854–861. doi:10.1080/14992027.2017.1339128.
- Ekberg, K., L. Hickson, and C. Grenness. 2017b. “Conversation Breakdowns in the Audiology Clinic: The Importance of Mutual Gaze.” International Journal of Language and Communication Disorders 52 (3): 346–355. doi:10.1111/1460-6984.12277.
- Ekberg, K., C. Grenness, and L. Hickson. 2014. “Addressing Patients’ Psychosocial Concerns Regarding Hearing Aids within Audiology Appointments for Older Adults.” American Journal of Audiology 23 (3): 337–350. doi:10.1044/2014_AJA-14-0011.
- Ferguson, M., D. Maidment, N. Russell, M. Gregory, and R. Nicholson. 2016. “Motivational Engagement in First-Time Hearing Aid Users: A Feasibility Study.” International Journal of Audiology 55 (3): 23–33. doi:10.3109/14992027.2015.1133935.
- Furlan, A. D., A. Malmivaara, R. Chou, C. G. Maher, R. A. Deyo, M. Schoene, G. Bronfort, et al. 2015. “Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group.” Spine 40 (21): 1660–1673. doi:10.1097/BRS.0000000000001061.
- Furlan, A. D., V. Pennick, C. Bombardier, and M. Van Tulder. 2009. “Updated Method Guidelines for Systematic Reviews in the Cochrane Back Review Group.” Spine 34 (34), 1929–1941. doi:10.1097/BRS.0b013e3181b1c99f.
- Gatehouse, S. 1999. “Glasgow Hearing Aid Benefit Profile: Derivation and Validation of.” Journal of the American Academy of Audiology 10: 80–103.
- Gatehouse, S., G. Naylor, and C. Elberling. 2006. “Linear and Nonlinear Hearing Aid Fittings –1. Patterns of Benefit.” International Journal of Audiology 45: 130–152. doi:10.1080/14992020500429518.
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014. “Patient-Centred Audiological Rehabilitation: Perspectives of Older Adults who Own Hearing Aids.” International Journal of Audiology 53: 68–75. doi:10.3109/14992027.2013.866280
- Grenness, C., L. Hickson, A. Laplante-Lévesque, C. Meyer, and B. Davidson. 2015. “The Nature of Communication Throughout Diagnosis and Management Planning in Initial Audiologic Rehabilitation Consultations.” Journal of the American Academy of Audiology 26 (1): 36–50. doi:10.3766/jaaa.26.1.5.
- Hartley, D., E. Rochtchina, P. Newall, M. Golding, and P. Mitchell. 2010. “Use of Hearing Aids and Assistive Listening Devices in an Older Australian Population.” Journal of the American Academy of Audiology 21 (10): 642–653. doi:10.3766/jaaa.21.10.4.
- Hindhede, A. L. 2010. “Disciplining the Audiological Encounter.” Health Sociology Review 19 (1): 100–113. doi:10.5172/hesr.2010.19.1.100.
- Knudsen, L. V., M. Oberg, C. Nielsen, G. Naylor, and S. E. Kramer. 2010. “Factors Influencing Help Seeking, Hearing Aid Uptake, Hearing Aid Use and Satisfaction with Hearing Aids: A review of the Literature.” Trends in Amplification 14 (3): 127–154. doi:10.1177/1084713810385712.
- Kochkin, S. 2000. “MarkeTrak V: ‘Why my hearing aids are in the drawer’: The consumers’ perspective.” The Hearing Journal 53 (2): 34–41. doi:10.1097/00025572-200002000-00004.
- Kochkin, S., D. L. Beck, L. A. Christensen, C. Compton-Conley, B. J. Fligor, P. B. Kricos, J. B. McSpaden, et al. 2010. “MarkeTrak VIII: The Impact of the Hearing Healthcare Professional on Hearing Aid User Success.” Hearing Review 17: 12–34.
- Laplante-Lévesque, A., L. Hickson, and L.Worrall. 2010. “Rehabilitation of Older Adults with Hearing Impairment: A Critical Review.” Journal of Aging and Health 22 (2): 143–153. doi:10.1177/0898264309352731.
- McCormack, A., and H. Fortnum. 2013. “Why do People Fitted with Hearing Aids not Wear Them?” International Journal of Audiology 52: 360–368. doi:10.3109/14992027.2013.769066.
- Melnyk, B. M., and E. Fineout-Overholt. 2011. Evidence-Based Practice in Nursing and Healthcare: A Guide to Best Practice. Philadelphia, US: Lippincott Williams and Wilkins.
- Meyer, C., C. Barr, A. Khan, and L. Hickson. 2017. Audiologist-patient communication profiles in hearing rehabilitation appointments. Patient Education and Counseling 100 (8): 1490–1498.
- Michie, S., L. Atkins, and R. West. 2014. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback.
- Michie, S., M. Richardson, M. Johnston, C. Abraham, J. Francis, W. Hardeman, M. P. Eccles, and J. Cane. 2013. “The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions.” Annals of Behaviour Medicine 46: 81–95. doi:10.1007/s12160-013-9486-6.
- Miller, W. R. and S. Rollnick. 2013. Motivational Interviewing: Helping People Change. 3rd Edition. New York: Guilford Press.
- Miller, W. R. and S. Rollnick. 2012. Motivational Interviewing: Helping People Change. New York: Guilford Press.
- Moher, D., A. Liberati, J. Tetzlaff, D. G. Altman, and The PRISMA Group. 2009. “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement.” PLoS Medicine 6 (7), 1–6. doi:10.1371/journal.pmed.1000097.
- Moore, G. F., S. Audrey, M. Barker, L. Bond, C. Bonell, W. Hardeman, L. Moore, et al. 2015. Process Evaluation of Complex Interventions: Medical Research Council Guidance. British Medical Journal 350: 1258. doi:10.1136/bmj.h1258.
- Nair, E. L., and K. M. Cienkowski. 2010. “The Impact of Health Literacy on Patient Understanding of Counseling and Education Materials.” International Journal of Audiology 49 (2): 71–75. doi:10.3109/14992020903280161.
- Naylor, G., M. Öberg, G. Wänström, and T. Lunner. 2015. “Exploring the Effects of the Narrative Embodied in the Hearing Aid Fitting Process on Treatment Outcomes.” Ear and Hearing 36 (5): 517–526. doi:10.1097/AUD.0000000000000157.
- Newman, C., B. Weinstein, G. Jacobson, and G. Hug. 1990. “The Hearing Handicap Inventory for Adults: Psychometric Adequacy and Audiometric Correlates.” Ear and Hearing 11: 430–433. doi:10.1097/00003446-199012000-00004.
- Noble, W. 2002. “Extending the IOI to Significant Others and to Non-Hearing- Aid-Based Interventions.” International Journal of Audiology 41: 27–29. doi:10.3109/14992020209101308.
- Pronk, M., D. J. H. Deeg, and S. E. Kramer. 2013. “Hearing Status in Older Persons: A Significant Determinant of Depression and Loneliness? Results from the Longitudinal Aging Study Amsterdam.” American Journal of Audiology 22 (2): 316–320. doi:10.1044/1059-0889(2013/12-0069).
- Pryce, H., A. Hall, A. Laplante-Levesque, and E. Clark. 2016. “A Qualitative Investigation of Decision Making During Help-Seeking for Adult Hearing Loss.” International Journal of Audiology 55 (11): 658–665. doi:10.1080/14992027.2016.1202455.
- Saunders, G. H., and A. Forsline. 2012. “Hearing-Aid Counseling: Comparison of Single-Session Informational Counseling with Single-Session Performance-Perceptual Counseling.” International Journal of Audiology 51 (10): 754–764. doi:10.3109/14992027.2012.699200.
- Sawyer, C., K. Munro, P. Dawes, M.O'Driscoll, and C. Armitage. In press. “Beyond Motivation: Identifying Target for Intervention to Increase Hearing Aid Use in Adults.” International Journal of Audiology.
- Scarinci, N., L. Worrall, and L. Hickson. 2008. “The Effect of Hearing Impairment in Older People on the Spouse.” International Journal of Audiology 47 (3): 141–151. doi:10.1080/14992020701689696.
- Sciacca, A., C. Meyer, K. Ekberg, C. Barr, and L. Hickson. 2017. “Exploring Audiologists’ Language and Hearing Aid Uptake in Initial Rehabilitation Appointments.” American Journal of Audiology 26: 110–118. doi:10.1044/2017_AJA-16-0061.
- Shay, L. A., and J. E. Lafata. 2015. “Where is the Evidence? A Systematic Review of Shared Decision Making and Patient Outcomes.” NIH Public Acess 35 (1): 114–131. doi:10.1177/0272989X14551638
- Solheim, J., C. Gay, A. Lerdal, L. Hickson, and K.J. Kvaerners. 2018. “An Evaluation of Motivational Interviewing for Increasing Hearing Aid Use: A Pilot Study.” Journal of the American Academy of Audiology 29 (8): 696–705. doi:10.3766/jaaa.16184.
- Sznitman, S. R., and D. S. Taubman. 2016. “Drug Use Normalization: A Systematic and Critical Mixed-Methods Review.” Journal of Studies on Alcohol and Drugs 77 (5), 700–709. doi:10.15288/jsad.2016.77.700.
- Vassar, M., P. Atakpo, and M. J. Kash. 2016. “Manual Search Approaches Used by Systematic Reviewers in Dermatology.” Journal of the Medical Library Association 104 (4): 302–304. doi:10.3163/1536-5050.104.4.009.
- Vas, V., M. A. Akeroyd, and D. A. Hall. 2017. “A Data-Driven Synthesis of Research Evidence for Domains of Hearing Loss, as Reported by Adults with Hearing Loss and their Communication Partners.” Trends in Hearing 21: 1–25. doi: 10.1177/2331216517734088.
- Ventry, I. and B. Weinstein. 1982. “The Hearing Handicap Inventory for the elderly: A New Tool.” Ear and Hearing 3: 40–46.
- World Health Organization. 2012. “WHO global estimates on prevalence of hearing loss.” Accessed date: 15th December 2017. http://www.who.int/pbd/deafness/estimates/en/.
- Zolnierek, H. K. B., and M. R. DiMatteo. 2009. “Physician Communication and Patient Adherence to treatment. A Meta-Analysis.” Medical Care 47 (8): 826–834. doi:10.1097/MLR.0b013e31819a5acc.