Abstract
Objective: This systematic review investigated if hearing aid use was associated with acute improvements in cognitive function in hearing-impaired adults.
Design: The review question and inclusion/exclusion criteria were designed using the Population, Intervention, Control, Outcomes, and Study design (PICOS) mnemonic. The review was pre-registered in the International Prospective Register of Systematic Review (PROSPERO) and performed in accordance with the statement on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Study sample: Thirteen articles, of various designs, published between 1990 and 2018, were identified via a search of five electronic databases.
Results: Most studies reported 1–2 cognitive outcome measures. Nine studies reported a significant improvement in outcome and four studies reported no significant change. None of the 13 studies received a high score on a quality assessment checklist. Due to concerns over risk of bias and indirectness, the overall quality of evidence was graded as low.
Conclusions: Only a few studies were identified, some of which report a small improvement in cognitive outcome; however, the overall quality of evidence was low. Further research is very likely to have an important impact on our confidence in answering the review question.
Introduction
It is well documented that successful listening requires effective cognitive processing, especially in circumstances that degrade the auditory input (Akeroyd Citation2008; Peelle Citation2017) or when listening goals are complex (Neher et al. Citation2011; Woods et al. Citation2013; Xia et al. Citation2017). On the other hand, less established is that successful hearing leads to improvement in cognition. The aim of this systematic review was to investigate if amplification by hearing aids leads to acute (i.e. rapid) improvements in cognitive function in adults.
There are several explanations for why hearing-aid use may acutely improve performance on a cognitive test. First, by improving access to auditory information, hearing aids may reduce the cognitive resources consumed by listening and thereby lead to improved performance on a concurrent cognitively demanding task (Sarampalis et al. Citation2009). Such concurrent task measurements are useful adjuncts to conventional measures of hearing-aid outcome, even if they are not necessarily indicative of improved cognitive ability. Second, the neural circuitry mediating a cognitive function can be strengthened and refined through repeated use (Merzenich, Van Vleet, and Nahum Citation2014). Hearing aids may promote such neural plasticity because an enriched auditory input enables the greater exercise of cognitive skills involved in listening (e.g. more audible sound sources may call for greater engagement of the neural mechanisms of selective attention). Finally, generalised improvement in cognitive health, perhaps through greater activity and social engagement giving rise to a cognitively-active lifestyle (Plassman Citation2010), may strengthen neural circuitry underlying domain-general cognitive skills that contribute to effective listening (Dawes et al. Citation2015). Repeated test-taking may result in performance improvements on a cognitive task; however, practice effects are not relevant to this review.
A large literature is available on the acute effects of hearing aids in relation to the effort of listening (reviewed recently in Ohlenforst et al. (Citation2017)). This effort is often assumed to be related to the allocation of cognitive resources to the listening task. Hearing-aid interventions are thought to improve the auditory input and free up cognitive resources. Studies have used dual-task procedures, physiological measures of brain activity and subjective self-reports. In the studies employing dual-task procedures, performance improvements on putative cognitive tasks were momentary consequences of cognitive resource reallocation rather than an improvement of cognitive ability per se. More generally, cognitive function was inferred indirectly in most of these listening effort studies; thus, these studies were not included in the review.
One reason to focus on acute effects rather than long-term effects is that the research community has shown considerable interest in the latter (with several studies underway), but it has not examined the former. A previous review (Kalluri and Humes Citation2012) noted overall weak evidence in support of an improvement of cognitive function due to long-term hearing-aid use, although the most rigorous studies in the review had failed to observe such effects. No corresponding systematic review of acute effects has been completed. Acute effects on cognitive function, if related to daily-life listening outcomes, may serve as clinically useful outcome measures. Reviewing the evidence about acute effects may help clarify the nature of long-term cognitive outcomes of hearing-aid use and its mechanisms by informing about the time course of changes in cognitive function.
Our aim was to review the evidence for acute improvements in cognitive abilities that result from hearing-aid use by adults. Accordingly, we defined the following research question for this systematic review: Is hearing-aid use associated with acute changes of cognitive function in adult listeners with hearing impairment? We were also interested in the potential for measurement of cognitive abilities to be deployed in clinical practice, so we originally posed two additional questions. First, are acute cognitive effects of hearing-aid use related to daily-life outcomes for adults with hearing impairment? Second, are acute cognitive effects sensitive to hearing-aid settings? Our search did not yield any studies that addressed these two additional questions, so they have not been discussed further.
We performed the review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. We reviewed studies that included real-life hearing-aid use. We also sought studies that employed hearing-aid simulations in the laboratory so that we could include all experiments that might be informative about immediate effects of hearing aids. Our criterion for effects to be considered acute was a generous 6 months after the onset of intervention. This was, in part, a reaction to the small number of studies that met our inclusion criteria when we initially used a 3-month period. We took account of these selection considerations in defining the inclusion and exclusion strategy according to the Population, Intervention, Control, Outcomes, and Study design (PICOS) criteria for systematic reviews (see below for details).
Methods
Before undertaking the review, we registered the study protocol in the International Prospective Register of Systematic Reviews (PROSPERO). The protocol can be accessed at www.crd.ac.uk/PROSPERO/display_record.asp?ID=CRD42017069075. In the protocol, we referred to “changes in cognition”: in this article, we have used the more specific term “improvements in cognition”.
Search strategy
Articles for inclusion in the review were identified through systematic searches of five electronic databases (Pubmed, Web of Science, ScienceDirect, GoogleScholar and EBSCOhost). We searched by using terms combining (hearing aid OR amplification OR hearing loss OR hearing impairment) AND (cognition OR cognitive OR attention OR working memory OR recall OR memory OR processing speed OR inhibition) AND (adult or NOT child*)1 and no date restrictions. We also identified additional articles by combing reference lists of applicable publications, as well as searching in Google using the terms “attention improvement” and “hearing aid” followed by a related article search of authors of papers of potential relevance. We conducted the search originally in May 2017 and then repeated it again in November 2018 in order to include papers published since the original search. After the many thousands of titles and abstracts from the search were reviewed for relevance, the total identified for examination was 29. Seven of these titles had newly emerged from the search that was repeated in November 2018.
Inclusion and exclusion
The PICOS criteria helped form the inclusion and exclusion rationale for screening the studies that emerged from our search strategy. summarises the PICOS criteria used.
Table 1. PICOS criteria for inclusion and exclusion of studies.
Two authors (SK and BA) independently assessed the titles and abstracts with respect to the PICOS criteria, conferred with each other and excluded several articles because they were deemed irrelevant. There was no disagreement between the two reviewers. The full-text of the remaining articles was then retrieved and assessed against PICOS criteria for further selection to arrive at the final set of articles included in the review.
Data extraction
For each included study, we extracted a number of elements about the study design and study results (see ). The extracted elements were chosen according to a checklist that was formulated based on relevance for assessing the acute cognitive effects of hearing-aid use. This comprised authors and publication year, and information regarding details of study design and intervention, participants (number, age and hearing level characteristics), hearing aid features and duration of use, outcome measures, timing of outcome measurement, main findings and significance of findings.
Table 2. Summary of studies that examined the acute cognitive effects of hearing aids on adult users.
Quality of evidence
We evaluated the quality of the evidence supporting acute cognitive effects of hearing-aid use according to the checklist of Downs and Black (Citation1998). This checklist has 27 questions pertaining to the quality of reporting, representativeness, external and internal validity (bias and confounding) and statistical power (see Supplementary Appendix for examples of questions from the checklist). Two authors (SK, KJM) independently assessed each study on each item of the checklist and arrived through discussion at the consensus ratings reported here. Given the relatively small number of studies that passed our inclusion criteria, we deemed it unnecessary to evaluate the risk of bias at the level of outcome assessment pooled across studies as is often done in systematic reviews (e.g. Ohlenforst et al. Citation2017).
The final step was to rate the overall quality (across studies) of outcome evidence using the quality elements developed by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group: (i) risk of bias, (ii) indirectness, (iii) inconsistency and (iv) imprecision (Guyatt et al. Citation2011).
Results
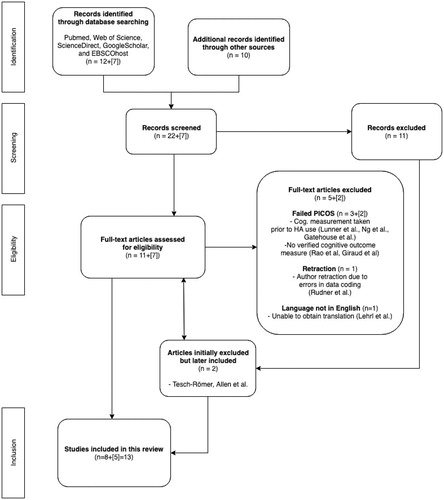
The PRISMA flow diagram in shows how studies included in the review were selected. In summary, 13 articles emerged as eligible for the review from an initial pool of 29 articles that we identified from database searching and additional manual searching. This pool of 29 articles was whittled down through application of the PICOS criteria and other factors (see Supplementary Appendix for articles that were eliminated during screening of the full text).
Figure 1. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram showing how the studies included in the study were identified, screened, assessed for eligibility and included. Numbers within square brackets are from the new search that was conducted in November 2018.
Data extraction
summarises the evidence about acute cognitive effects from the included studies. All studies involved older listeners in the age range of typical first-time adult hearing-aid users and sufficient hearing losses to merit the prescription of hearing aids in conventional clinical practice.
Two of the studies were conducted at least two decades ago (Mulrow Citation1990; Tesch-Römer Citation1997). One notable feature of these two older studies is the very high proportion of monaural hearing-aid fittings. Two more recent studies in our pool did not specify if the hearing-aid fittings used were bilateral (Acar et al. Citation2011; Choi et al. Citation2011).
Nine studies noted an improvement in cognitive outcome measures. In two of these cases, cognition was assessed using general dementia screening tools that provided little insight about the nature of cognition improvement (Acar et al. Citation2011; Mulrow Citation1990). Six studies assessed cognitive function after three or more months of hearing-aid use (Acar et al. Citation2011; Choi et al. Citation2011; Deal et al. Citation2017; Karawani, Jenkins, and Anderson Citation2018; Mulrow Citation1990; Zarenoe et al. Citation2017), a considerable amount of time that is perhaps more relevant to long-term effects rather than momentary or acute effects.
In six studies, within-subject comparisons assessed the cognitive effects of hearing-aid use (Doherty and Desjardins Citation2015; Desjardins Citation2016; Hällgren et al. Citation2005; Zarenoe et al. Citation2017; Saunders et al. Citation2018). For example, one of these studies assessed the momentary cognitive effect of amplification by comparing the aided versus unaided performance on an auditory cognitive test at a given point in time (Doherty and Desjardins Citation2015). In this and two other such within-subject designs that used auditory cognitive tests (Desjardins Citation2016; Hällgren et al. Citation2005), acute effects were attributable to improved auditory processing of the acoustic input rather than to improvements in domain-general cognitive abilities that would manifest in tests administered through other modalities such as vision. Within-subject comparisons of two other studies (Castiglione et al. Citation2016; Zarenoe et al. Citation2017) yielded improvements of cognitive measures, but these did not have suitable control conditions to rule out practice or placebo effects.
Four of the thirteen studies failed to observe any improvement in cognitive function (Allen Citation2003; Hällgren et al. Citation2005; Tesch-Römer Citation1997; Saunders et al. Citation2018). It is worth noting that one of these studies was on patients with a diagnosis of primary dementia (Allen Citation2003), a patient group that is not representative of most users of hearing aids. Another study used experienced users of hearing aids (Hällgren et al. Citation2005). These users may not readily show the acute improvements that might ensue from a newly enriched auditory experience of new hearing-aid users.
Quality of evidence
Quality of individual studies
shows the result of our assessment of the methodological quality of the individual studies according to the checklist of Downs and Black (Citation1998). None of the studies passed our locally determined threshold of quality of 75% of the maximum possible score (range 28–68%). While the quality of reporting and internal validity was generally high, most studies had poor external validity and exhibited selection biases.
Table 3. Methodological quality of individual studies assessed according to the checklist of Downs and Black (Downs and Black Citation1998).
The low scores for external validity were most frequently due to inadequate demonstration that subject populations and treatments were representative for the general population (e.g. a single audiologist performed the best fit and fine-tuning of hearing aids for all participants in Acar et al. Citation2011). The low scores for selection bias were a consequence of non-random assignment, absence of control groups (Acar et al. Citation2011; Desjardins Citation2016; Hällgren et al. Citation2005) and absence of treatment blinding to patient and researcher alike.
Furthermore, information about confounding factors such as prior hearing-aid experience, quality of hearing-aid fitting and amount of daily hearing-aid use was sometimes missing or unaccounted for. Two studies reported that participants had prior hearing aid experience (Hällgren et al. Citation2005; Castiglione et al. Citation2016), five studies did not report this information at all (Mulrow Citation1990; Allen Citation2003; Choi et al. Citation2011; Zarenoe et al. Citation2017; Saunders et al. Citation2018), while the remainder reported no prior hearing-aid experience. Similarly, confirmation of daily use and information about wear time were sometimes missing, although in the cases where these were reported, daily use generally exceeded 5 h.
Quality of the overall evidence base
There were multiple concerns about overall quality, primarily over risk of bias (from lack of blinding) and indirectness (differences between the study sample and the population of interest). Therefore, the overall quality of outcome evidence was graded as low. Further research is very likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Discussion
The aim of this study was to review the evidence for acute improvement of cognitive abilities due to hearing-aid use by adults. The search identified 13 studies that examined this question directly. Overall, nine studies indicated a significant positive effect of hearing aids on cognitive function after hearing-aid use of a few weeks while four found no change. This finding of improved cognitive function should be interpreted cautiously for the following reasons:
Where cognitive outcomes were significantly improved, the effects were modest in size.
Studies reporting positive outcomes used designs generally with low external validity and furthermore, they failed to account adequately for confounders that lead to selection biases. As such, the wider applicability of their positive findings is debateable.
Several studies reported positive effects of hearing-aid use on cognitive function after four to six months of hearing-aid use, which leaves unknown if such effects would be seen more rapidly.
Low external validity and selection bias characterised all of the studies, so that the generalisability of those studies that did not find an acute effect of hearing-aid use can be questioned. For example, Hällgren et al. (2005) did not find an acute effect of hearing-aid use; however, participants in the experiment had prior experience with hearing aids that may have diminished or eliminated any acute effects. For another example, considerable numbers of participants across the studies in this review might have experienced unilateral rather than bilateral fits. Putative cognitive effects may have been underestimated in these participants.
The relatively small number of studies that met our inclusion criteria is somewhat surprising given the significant activity in the audiology research community devoted to exploring links between cognition and hearing. This, however, can be attributed to many articles failing our inclusion criteria because they did not directly assess cognitive functions or satisfy all PICOS criteria.
There is a large body of literature, which did not meet our inclusion criteria, that examines the effect of hearing impairment and hearing aids on listening effort. This literature was recently reviewed by Ohlenforst et al. (Citation2017). These measures of effort are interpreted frequently in cognitive terms. However, we left out these studies because direct links of the listening effort measures to explicit cognitive abilities have yet to be clearly demonstrated (McGarrigle et al. Citation2014).
Overall, few studies have directly examined acute cognitive effects of hearing-aid use and none have employed designs with high enough quality to unambiguously assess the existence of acute cognitive effects. As such, there is a need for high-quality randomised control trials (RCTs) that directly address the presence of acute cognitive effects. There is especially a need for examining effects at short intervals of a few days to 1–2 weeks of hearing-aid use because there are hardly any studies that have examined such short intervals. Such data will help clarify the cognitive effects of hearing aids and how any such putative effects might be applied in a clinical context.
Conclusions
Thirteen studies were identified in the review and nine reported a small but significant acute improvement in cognitive outcome. However, there are important limitations in the design of many of these studies and the overall quality of evidence is low. Further research, including RCTs investigating changes in cognitive outcome within days/weeks of hearing aid fitting, is very likely to have an important impact on our confidence in answering the review question.
Acknowledgements
The authors gratefully acknowledge the help of Rebekah Bruckner for searching and screening studies for inclusion in the review. They are also grateful to the two anonymous reviewers and the editor for helping improve the manuscript.
Disclosure statement
The authors report no declarations of interest.
Note
Additional information
Funding
Notes
1 ScienceDirect yielded 11,863 results using terms “hearing aid” AND “cognitive function” AND “adult”; Web of Science yielded 284 records using terms Hearing aid (215,003) AND cognition (544,563) AND adult (1,439,003); Google Scholar yielded 401,000 results using terms “hearing aid” AND “adult” AND “cognition” OR “attention”; Using EBSCOhost, the search “hearing aid” OR “hearing impairment” AND “cognition” NOT “child*” limited to Scholarly (Peer Reviewed) Journals, Magazines and Reviews returned 167,521 results.
References
- Acar, B., M. F. Yurekli, M. A. Babademez, H. Karabulut, and R. M. Karasen. 2011. “Effects of Hearing Aids on Cognitive Functions and Depressive Signs in Elderly People.” Archives of Gerontology and Geriatrics 52 (3): 250–252. doi:10.1016/j.archger.2010.04.013.
- Akeroyd, M. 2008. “Are Individual Differences in Speech Reception Related to Individual Differences in Cognitive Ability? A Survey of Twenty Experimental Studies with Normal and Hearing-Impaired Adults.” International Journal of Audiology 47 (2): S53–S71. doi:10.1080/14992020802301142.
- Allen, N. H. 2003. “The Effects of Improving Hearing in Dementia.” Age and Ageing 32 (2): 189–193. doi:10.1093/ageing/32.2.189.
- Bolia, R. S., W. T. Nelson, M. A. Ericson, and B. D. Simpson. 2000. “A Speech Corpus for Multitalker Communications Research.” Journal of the Acoustical Society of America 107 (2): 1065–1066. doi:10.1121/1.428288.
- Castiglione, A., A. Benatti, C. Velardita, D. Favaro, E. Padoan, D. Severi, M. Pagliaro., et al. 2016. “Aging, Cognitive Decline and Hearing Loss: Effects of Auditory Rehabilitation and Training with Hearing Aids and Cochlear Implants on Cognitive Function and Depression among Older Adults.” Audiology and Neurotology 21 (1): 21–28. doi:10.1159/000448350.
- Choi, A., H. Young, J. Shim, S. H. Lee, S. W. Yoon, and E.J. Joo. 2011. “Is Cognitive Function in Adults with Hearing Impairment Improved by the Use of Hearing Aids?” Clinical and Experimental Otorhinolaryngology 4 (2): 72–76. doi:10.3342/ceo.2011.4.2.72.
- Dawes, P., R. Emsley, K. J. Cruickshanks, D. R. Moore, H. Fortnum, M. Edmondson-Jones, A. McCormack, and K. J. Munro. 2015. “Hearing Loss and Cognition: The Role of Hearing Aids, Social Isolation and Depression.” PLoS One 10 (3): e0119616. doi:10.1371/journal.pone.0119616.
- Deal, J. A., M. S. Albert, M. Arnold, S. I. Bangdiwala, T. Chisolm, S. Davis, A. Eddins., et al. 2017. “A Randomized Feasibility Pilot Trial of Hearing Treatment for Reducing Cognitive Decline: Results from the Aging and Cognitive Health Evaluation in Elders Pilot Study.” Alzheimer’s & Dementia (New York, NY) 3 (3): 410–415. doi:10.1016/j.trci.2017.06.003.
- Desjardins, J. L. 2016. “Analysis of Performance on Cognitive Test Measures Before, During, and After 6 Months of Hearing Aid Use: A Single-Subject Experimental Design.” American Journal of Audiology 25 (2): 127–141. doi:10.1044/2016_AJA-15-0067.
- Doherty, K. A., and J. L. Desjardins. 2015. “The Benefit of Amplification on Auditory Working Memory Function in Middle-Aged and Young-Older Hearing Impaired Adults.” Frontiers in Psychology 6: 721. doi:10.3389/fpsyg.2015.00721.
- Downs, S. H., and N. Black. 1998. “The Feasibility of Creating a Checklist for the Assessment of the Methodological Quality Both of Randomised and Non-Randomised Studies of Health Care Interventions.” Journal of Epidemiology & Community Health 52 (6): 377–384. doi:10.1136/jech.52.6.377.
- Gatehouse, S., G. Naylor, and C. Elberling. 2003. “Benefits from Hearing Aids in Relation to the Interaction between the User and the Environment.” International Journal of Audiology 42: S77–S85. doi:10.3109/14992020309074627.
- Giroud, N., U. Lemke, P. Reich, K. L. Matthes, and M. Meyer. 2017. “The Impact of Hearing Aids and Age-Related Hearing Loss on Auditory Plasticity across Three Months - An Electrical Neuroimaging Study.” Hearing Research 353: 162–175. doi:10.1016/j.heares.2017.06.012.
- Guyatt, G. H., A. D. Oxman, H. J. Schünemann, P. Tugwell, and A. Knottnerus. 2011. “GRADE Guidelines: A New Series of Articles in the Journal of Clinical Epidemiology.” Journal of Clinical Epidemiology 64 (4): 380–382. doi:10.1016/j.jclinepi.2010.09.011.
- Hällgren, M., B. Larsby, B. Lyxell, and S. Arlinger. 2005. “Speech Understanding in Quiet and Noise, with and without Hearing Aids.” International Journal of Audiology 44 (10): 574–583. doi:10.1080/14992020500190011
- Hua, H., M. Emilsson, R. Ellis, S. Widén, and C. Möller, B. Lyxell. 2014. “Cognitive Skills and the Effect of Noise on Perceived Effort in Employees with Aided Hearing Impairment and Normal Hearing.” Noise and Health 16 (69): 79–88. doi:10.4103/1463-1741.132085.
- Kalluri, S., and L. E. Humes. 2012. “Hearing Technology and Cognition.” American Journal of Audiology 21 (2): 338. doi:10.1044/1059-0889(2012/12-0026.
- Karawani, H., K. Jenkins, and S. Anderson. 2018. “Restoration of Sensory Input May Improve Cognitive and Neural Function.” Neuropsychologia 114: 203–213. doi:10.1016/j.neuropsychologia.2018.04.041.
- Lehrl, S., R. Funk, and K. Seifert. 2005. “[The First Hearing Aid Increases Mental Capacity. Open Controlled Clinical Trial as a Pilot Study].” HNO 53 (10): 852–862. doi:10.1007/s00106-005-1253-y.
- Lunner, T., E. Sundewall-Thorén. 2007. “[Interactions Between Cognition, Compression, and Listening Conditions: Effects on Speech-in-Noise].” Journal of the American Academy of Audiology 18 (7): 604. doi:10.3766/jaaa.18.7.7.
- McGarrigle, R., K. J. Munro, P. Dawes, A. J. Stewart, D. R. Moore, J. G. Barry, and S. Amitay. 2014. “Listening Effort and Fatigue: What Exactly Are We Measuring? a British Society of Audiology Cognition in Hearing Special Interest Group ‘White Paper.” International Journal of Audiology 53 (7): 433–445. doi:10.3109/14992027.2014.890296.
- Merzenich, M. M., T. M. Van Vleet, and M. Nahum. 2014. “Brain Plasticity-Based Therapeutics.” Frontiers in Human Neuroscience 8: 385. doi:10.3389/fnhum.2014.00385.
- Mulrow, C. D. 1990. “Quality-of-Life Changes and Hearing Impairment: A Randomized Trial.” Annals of Internal Medicine 113 (3): 188. doi:10.7326/0003-4819-113-3-188.
- Neher, T., S. Laugesen, N. S. Jensen, and L. Kragelund. 2011. “Can Basic Auditory and Cognitive Measures Predict Hearing-Impaired Listeners’ Localization and Spatial Speech Recognition Abilities?” Journal of the Acoustical Society of America 130 (3): 1542–1558. doi:10.1121/1.3608122.
- Ng, E. H. N., E. Classon, B. Larsby, S. Arlinger, T. Lunner, M. Rudner, and J. Rönnberg. 2014. “Dynamic Relation between Working Memory Capacity and Speech Recognition in Noise during the First 6 Months of Hearing Aid Use.” Trends in Hearing 18: 233121651455868. doi:10.1177/2331216514558688.
- Ohlenforst, B., A. A. Zekveld, E. P. Jansma, Y. Wang, G. Naylor, A. Lorens, T. Lunner, and S. E. Kramer. 2017. “Effects of Hearing Impairment and Hearing Aid Amplification on Listening Effort: A Systematic Review.” Ear and Hearing 38 (3): 267–281. doi:10.1097/AUD.0000000000000396.
- Peelle, J. E. 2017. “Listening Effort: How the Cognitive Consequences of Acoustic Challenge are Reflected in Brain and Behavior.” Ear and Hearing Publish Ahead of Print 39: 204–214. doi:10.1097/AUD.0000000000000494.
- Plassman, B. L. 2010. “Systematic Review: Factors Associated with Risk for and Possible Prevention of Cognitive Decline in Later Life.” Annals of Internal Medicine 153 (3): 182. doi:10.7326/0003-4819-153-3-201008030-00258.
- Qian, Z. J., K. Wattamwar, F. F. Caruana, J. Otter, M. J. Leskowitz, B. Siedlecki, J. B. Spitzer, and A. K. Lalwani. 2016. “Hearing Aid Use is Associated with Better Mini-Mental State Exam Performance.” The American Journal of Geriatric Psychiatry 24 (9): 694–702. doi:10.1016/j.jagp.2016.03.005.
- Rao, A., D. Rishiq, Y. Luodi, Z. Yang, H. Abrams, L. Yu, and Y. Zhang. 2017. “Neural Correlates of Selective Attention with Hearing Aid Use Followed by Read My Quips Auditory Training Program.” Ear & Hearing 38 (1): 28–41. doi:10.1097/AUD.0000000000000348.
- Rudner, M., C. Foo, J. Rönnberg, and T. Lunner. 2007. “Phonological Mismatch Makes Aided Speech Recognition in Noise Cognitively Taxing.” Ear & Hearing 28 (6):879–892. doi:10.1097/AUD.0b013e3181576c9c.
- Sarampalis, A., S. Kalluri, B. Edwards, and E. Hafter. 2009. “Objective Measures of Listening Effort: Effects of Background Noise and Noise Reduction.” Journal of Speech, Language, and Hearing Research 52 (5): 1230–1240. doi:10.1044/1092-4388(2009/08-0111).
- Saunders, G. H., I. Odgear, A. Cosgrove, and M. T. Frederick. 2018. “Impact of Hearing Loss and Amplification on Performance on a Cognitive Screening Test.” Journal of the American Academy of Audiology 29 (7): 648–655. doi:10.3766/jaaa.17044.
- Tesch-Römer, C. 1997. “Psychological Effects of Hearing Aid Use in Older Adults.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 52 (3):P127–P138. doi:10.1093/geronb/52B.3.P127.
- Wong, L. L. N., J. K. Y. Yu, S. S. Chan, and M. C. F. Tong. 2014. “Screening of Cognitive Function and Hearing Impairment in Older Adults: A Preliminary Study.” BioMed Research International 2014: 1. doi:10.1155/2014/867852.
- Woods, W. S., S. Kalluri, S. Pentony, and N. Nooraei. 2013. “Predicting the Effect of Hearing Loss and Audibility on Amplified Speech Reception in a Multi-Talker Listening Scenario.” The Journal of the Acoustical Society of America 133 (6): 4268–4278. doi:10.1121/1.4803859.
- Xia, J., S. Kalluri, C. Micheyl, and E. Hafter. 2017. “Continued Search for Better Prediction of Aided Speech Understanding in Multi-Talker Environments.” The Journal of the Acoustical Society of America 142 (4): 2386–2399. doi:10.1121/1.5008498.
- Zarenoe, R., M. Hallgren, G. Andersson, and T. R Ledin. 2017. “Working Memory, Sleep, and Hearing Problems in Patients with Tinnitus and Hearing Loss Fitted with Hearing Aids.” Journal of the American Academy of Audiology 28 (2): 141–151. doi:10.3766/jaaa.16023.

