Abstract
Objective: Two studies explored hearing-aid user and audiologist experiences of hearing-aid use and fitting for music in the UK.
Design and sample: One-hundred-seventy-six hearing-aid users (age range: 21–93 years; mean: 60.56 years) answered a 4-item questionnaire on music listening difficulties and discussions about music in clinic. 99 audiologists (age range: 22–71 years; mean: 39.18 years) answered a 36-item questionnaire on the frequency and type of discussions, training received, and strategies for optimizing hearing aids for music. Closed and open-ended questions were included.
Results: Sixty seven percent of hearing-aid users reported some degree of difficulty listening to music with hearing aids, and 58% had never discussed music in clinic. 50% of audiologists surveyed asked 1 in 5 (or fewer) patients about music and 67% had never received music-specific training. Audiologist training on music was significantly associated with confidence in providing advice, confidence in programming hearing aids for music, and programming hearing aids for music for a greater number of patients.
Conclusions: Hearing-aid users’ and audiologists’ experiences of music remain mixed. In the absence of formalised training in optimizing hearing aids for music, there is a need for systematic research relating fitting strategies to clinical outcomes and the development of guidelines for audiologist training.
Introduction
Music listening is ubiquituous and millions of people in Western industrialised contexts engage with music daily for enjoyment, to regulate moods, accompany everyday activities (e.g. housework, travelling, exercise), and for social connectedness (Lamont, Greasley, and Sloboda Citation2016; Schäfer et al. Citation2013). Music listening is also important for the 11 million deaf and hearing impaired people in the UK, a population that is predicted to grow to 15.6 million by 2035 due to increasing rates of noise-induced hearing loss (NIHL) and presbycusis (Action on Hearing Loss Citation2015). Evidence of the efficacy of music amplification using hearing aids however, is mixed (Fulford, Ginsborg, and Greasley Citation2015; Madsen and Moore Citation2014; Looi, Rutledge, and Prvan Citation2019). While audiological case studies exist (Beck Citation2016; Chasin Citation2012, Citation2018), there appear to be none that systematically explore the ways in which audiologists currently programme hearing aids for music in the clinic. This article decribes findings of two questionnaire studies providing novel data on audiologists’ perspectives on fitting hearing aids for music listening in the clinic, and hearing-aid users’ experiences of discussions with audiologists about music listening with hearing aids.
Music listening with hearing aids
In considering the effects of hearing aids on music listening, it is important to acknowledge that the perceptual deficits associated with hearing loss itself can account for some of the difficulties encountered when listening to music. Hearing-impaired listeners perform poorly compared to normally hearing listeners on music perceptual tasks such as pitch discrimination, melodic intonation, and identifying instruments (Kirchberger and Russo Citation2015; Uys and van Dijk Citation2011) due to threshold elevation, reduced frequency selectivity, loudness recruitment, and anomalies in pitch perception (Cai, Zhao, and Zheng Citation2013; Moore Citation2016). For example, using the Adaptive Music Perception (AMP) test, Kirchberger and Russo (Citation2015) found that normally hearing and hearing-impaired listeners performed similarly on metre perception tests, but that those with hearing impairment performed significantly worse on pitch discrimination, intonation and melody detection tasks. Yet there is evidence that hearing aids themselves can contribute to problems by distorting the music signal (Beck Citation2014; Chasin and Russo Citation2004; Chasin and Hockley Citation2012; Madsen and Moore Citation2014).
Alongside studies concerned with cochlear implant technology and music (cf. Looi, Gfeller, and Driscoll Citation2012), there is an increasing literature investigating music perception and/or music listening using hearing aids (e.g. Leek et al. Citation2008; Looi, Rutledge, and Prvan Citation2019; Madsen and Moore Citation2014; Vaisberg et al. Citation2019; Uys and van Dijk Citation2011). In an interview study of 68 elderly hearing-impaired listeners, Leek et al. (Citation2008) found that 41% reported that wearing hearing aids made music more enjoyable, but 37% reported that they made no difference. A larger survey by Madsen and Moore (Citation2014, n = 523) showed that hearing aids were helpful for listening to both reproduced and live music, making sounds clearer and enhancing a person’s ability to hear individual instruments. However, more than 33% of hearing-aid users in their study reported experiencing feedback and more than 50% reported experiencing distortion during music listening. Most recently, another survey by Looi, Rutledge, and Prvan (Citation2019, n = 111) found that hearing-aid users with moderate and severe levels of hearing loss tended to report less enjoyment from music and that their hearing aids made music sound less melodic compared to those with a mild hearing loss.
There is evidence that musicians in particular may find hearing aids more problematic than non-musicians. Interviews and observational research with D/deaf musicians1 have revealed mixed accounts of hearing-aid use; while hearing aids can be a necessity for music performance, many experience pitch distortion and feedback and some opt not to use hearing aids at all (Fulford, Ginsborg, and Goldbart Citation2011; Fulford, Ginsborg, and Greasley Citation2015). Vaisberg et al. (Citation2019) research with amateur musicians highlighted issues with sound quality, and difficulties with perception such as problems with intonation and melodic recognition, and instrumental identification. Difficulty hearing the conductor was found to be a key motivation for wearing hearing aids during music performance in spite of specific musical auditory perception deficits with hearing-aid use.
The mixed sentiment around hearing-aid use for music listening is likely due to the mismatch between design and usage. Digital signal processing (DSP) algorithms in hearing aids have been primarily designed to amplify speech and support verbal-aural communication between people, being programmed around the relatively constant and finite spectral properties (dynamic and frequency range, crest factors) of speech acoustics (Chasin Citation2010; Chasin and Russo Citation2004; Revit Citation2009). DSP algorithms compress amplification for specific frequencies (wide dynamic range compression or WDRC), adapt to sudden loud noises (automatic gain control, fast acting compression) and minimise feedback. Music encompasses a vast array of sounds and has far larger dynamic (up to 100 dB SPL) and frequency (0.02 kHz to 20 kHz) ranges and crest factors (18–20dB) than speech (Chasin and Hockley Citation2014; Tozer and Crook Citation2012). These differences are likely to contribute to the mixed experiences of music listening by hearing-aid users. Many hearing-aid manufacturers include music listening programmes in their devices which are foregrounded in their marketing and claim to help with auditory music perception, yet research on benefit, or perceptual improvements with music programmes is limited. Madsen and Moore (Citation2014) found that only 38% of users had a music programme (n = 198 from total N = 523), and whilst a third of this group reported greater clarity in hearing musical instruments, no differences were found across any other responses (e.g. helping to hear soft passages, improving tone quality). Vaisberg et al. (Citation2019) highlighted that a small number of musicians reported improvements in the balance and brightness of sounds, however the majority did not report benefit from the music programme. Looi, Rutledge, and Prvan (Citation2019) found that only 23% of users (n = 25 of N = 111) had a music programme, and that the majority (69%) of the sample reported their everyday programme provided the best sound quality for music.
Audiologists’ experience of music and hearing aids
Programming hearing aids for music listening is not standard practice or training for audiologists. A review of the content of UK audiological courses conducted in May/June 2019 by the present research team revealed that music is not considered part of routine audiology and no compulsory (or optional) training is provided within curriculums. Globally, a small number of audiology clinics promote expertise in fitting hearing aids for musicians, and a small pool of audiologists specialise in music. However, there is a notable absence of empirical evidence about how audiologists are handling issues with music listening in clinical practice. Despite the widespread marketing of music programmes by commercial manufacturers, there exists no validated outcome measure or empirical evidence base linking acoustic parameters to improved outcomes.
In a special edition of Trends in Amplification dedicated to music, Chasin and Hockley (Citation2012) provide suggestions for audiologists based on their clinical experience. They suggest, for example, that audiologists assess the use of adaptive functions (e.g. feedback cancellation and noise reduction), WDRC parameters and bandwidths depending on degree of hearing loss. For hearing-aid users, they suggest adjusting the volume of the music source and their hearing aids if possible, using tape to cover the microphone of the hearing aids, and even changing their musical instrument (see also Chasin Citation2010). Currently, the extent to which audiologists are using such strategies, whether they lead to improved outcomes for music listening, or to what extent discussions about music listening are taking place in the clinic at all, is not known.
The use of hearing-aid amplification for music listening therefore presents unique challenges. Amplification requirements are likely to be highly idiosyncratic and depend on a wide variety of variables including acoustics, instruments, sound source, level of musical training, hearing loss configuration and the specific hearing-aid technology used. The lack of evidence and standardised protocol around fitting hearing aids for music mean that successful outcomes are likely to be driven by identifying the hearing-aid users’ individual needs as much as the audiologist may have an understanding of musical acoustics. Music programmes themselves may not be uniquely configurable. There is also a lack of technical specification data from manufacturers about their design and function as manufacturers do not typically publish detailed information regarding the DSP used in music programmes. There is a need to understand the extent to which audiologists are presented with issues relating to music in the clinic, and the strategies currently used by audiologists experienced in fitting hearing aids for music. It is also crucial to understand the extent to which strategies are beneficial for the hearing-aid users, before developing guidelines for clinical practice. The lack of mandatory, formalised training suggests that audiologists have not had the opportunity to develop specific skills in this area.
This paper presents the findings of two small-scale surveys conducted as part of the AHRC-funded Hearing Aids for Music project which aimed to research issues surrounding music listening with hearing aids. The first, a survey of hearing-aid users, aimed to explore the prevalence and characteristics of issues around music listening using hearing aids and about outcomes via discussions with their audiologists. The second, a survey of audiologists, aimed to reveal the extent and outcomes of discussions about music listening in the clinic, the strategies adopted in advising on music listening, and the experiences and confidence levels of audiologists in doing so.
Methods
Hearing-aid user survey
A paper-based questionnaire was distributed to patients attending two clinical sites in the UK (Ethics Ref: NS/15/0020). The first was at a large public (National Health Service) audiology clinic. The second site was an independent practice. A total of 176 hearing-aid users completed the survey (see for participant demographics by site).
Table 1. Number of participants, age and gender by hearing clinic.
The questionnaire contained four questions, each with a rating scale (7 pt Likert scale, e.g. 1 “Not at all” to 7 “All the time”) and an open-ended response, asking participants (1) whether they experience any problems with music listening, (2) the extent to which this might affect their quality of life, (3) whether they have discussed music listening with their audiologist and (4) the degree to which this has improved their music listening experiences. The questionnaire was designed to be completed in five minutes in the clinic waiting room.
Audiologists’ survey
An online questionnaire was distributed to audiologists using an electronic mailing list provided by the British Academy of Audiology (BAA), the largest association of hearing professionals in the UK (Ethics Reference: LTMUSC-048). Ninety-nine audiologists took part (see for demographics).
Table 2. Demographic data and general fitting strategies of audiologists.
In addition to demographics, audiologists were asked questions about fitting procedures (e.g. what style of hearing aids they typically fit, whether they fit binaural aids as standard, use real ear verification, and provide patients with volume control). Data from these questions can also be found in . Audiologists were then asked about the frequency and nature of discussions about music (e.g. percentage of appointments in which they ask about music, topics covered, perceived usefulness of hearing aids for music, and how confident they feel in providing advice), any training they had received on the subject of music (e.g. courses, conferences), and their experience of programming hearing aids for music (e.g. adjustments in addition to a manufacturer-defined music programmes, years’ experience programming hearing aids for music, and number of patients for whom they do this).
Analysis
Quantitative data from the surveys including Likert scales were analysed and reported using descriptive statistics. The relationships between categorical variables were explored using chi-square analyses performed in SPSS. Qualitative data from the open-ended responses were analysed thematically using NVivo. Full text responses were uploaded and a thematic analysis performed in which instances of recurrent themes in the data were identified and coded so that the prevalence of each theme could be quantified. We report results of both surveys below as follows: hearing-aid users’ experiences of music listening, discussions in clinic from both user and audiologist perspectives, audiologists’ experience and confidence programming hearing aids for music and finally, training and resources.
Results
Hearing-aid users’ experiences of music listening
Reported experiences of music listening using hearing aids were mixed. The mean response to the question “Do you experience problems when listening to music?” (1 “Not at all” to 7 “All the time”) was 4.14 (SD = 1.94), with the majority of respondents selecting rating 4 “Sometimes” (see ). One third (33%) of respondents (taking response categories 1, 2 and 3) did not experience any (15%) or many (18%) difficulties and open-ended responses attested to the usefulness of hearing aids for listening and performance: “Do not seem to have a problem with music”; “With my new hearing aids, I can hear music better”; “I play guitar and the hearing-aid I use makes a huge difference for me”. Respondents also reported strategies for avoiding problems such as removing hearing aids or adjusting the volume of the music: “Adjusting volume up or down as the songs change”; “I turn down the volume from the default position as it distorts otherwise. This is not a problem”.
Figure 1. Frequency of problems experienced when listening to music (a [n = 175]), and extent to which this negatively affects quality of life ( b [n = 167]) across all participants.
![Figure 1. Frequency of problems experienced when listening to music (a [n = 175]), and extent to which this negatively affects quality of life ( b [n = 167]) across all participants.](/cms/asset/dca17974-1d44-44ff-a63a-91a738e43fdf/iija_a_1762126_f0001_b.jpg)
Around two-thirds (67%) however, experienced problems at least sometimes (). The most commonly reported problem in the open-ended responses was difficulties with pitch perception (see ). Respondents noted difficulties hearing pitches (particularly high frequencies), and music sounding out of tune: “Unable to hear certain pitches”; “when I’m playing the piano I can’t tell if I’m playing the right notes or not”. One reported experiencing diplacusis, a hearing condition when sounds are heard differently (e.g. a single pitch is heard as two different pitches). Some mentioned issues listening to live music as opposed to recorded music, and having to remove hearing aids altogether to avoid feedback or distortion: “I get feedback from my hearing aids at concerts which other concert-goers hear, and as a result I have to remove my aid”; “I always have to remove my hearing aids at live music events, especially loud ones. The bass is always unbearable with the hearing aids, creating distortion, making it impossible to hear”. The third most frequent coded theme in the responses was issues with volume and dynamic ranges: “cannot always hear the range of music”; “I tend to miss the impact of very quiet orchestral parts of a performance or piece of music”; “I often have to play the music too loud thus annoying other people”.
Figure 2. Do you experience problems when listening to music? Thematically coded responses (n = 105, percentages sum >100% as participants contributed to >1 theme).
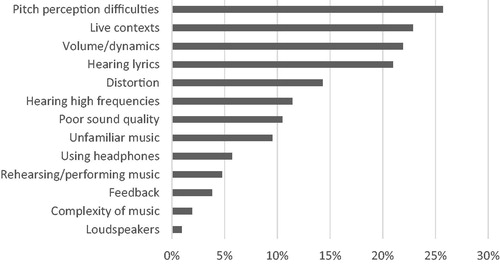
Other problems related to distortion or lack of clarity: “sounds ‘tinny’ and indistinct”; “muffled”; “no fidelity”. Some respondents stated not being able to hear the words in songs which made listening to new or unfamiliar music challenging: “loss of clarity in understanding/following words/vocal parts in singing”; “I do not listen because I cannot hear the words - I want to know the “story” when I listen to singing”. Others reported that even familiar music was distorted when listening using hearing aids.
Participants were asked whether problems listening to music using hearing aids negatively affected quality of life. The modal response was “Not at all” but responses were evenly dispersed (M = 3.81, SD = 2.05, ). One respondent who worked in the broadcasting/record industry reported having to take their hearing aids out to use headphones when editing at work, stating that it is “a constant issue, but ‘quality of life’ is a bit much”. Other respondents indicated that their hearing aids enable at least some level of engagement in musical life. For example, one respondent noted an ongoing compromise between sound quality and attendance:
I go to concerts twice a month on average and hear the music less well than I would if the aid didn’t distort the sound of the music. The effect is relative and doesn’t stop me attending concerts - better than not going!
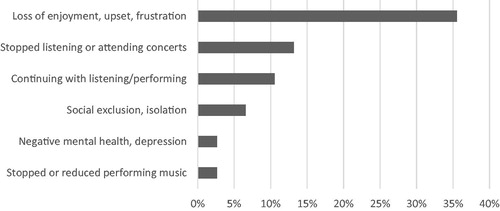
As can be seen from , approximately a third of respondents indicated a loss of enjoyment of music: “Music has always been very important to me, and it’s very frustrating not being able to enjoy it like I used to”; “I can no longer go to concerts or listen to any record/CD collection with any pleasure”. Some reported that they had stopped listening or attending concerts which had led to feeling socially isolated or excluded:
I don’t feel confident to participate in music playing in a group or alone to an audience. Unable to sing along to songs as I cannot hear the words at all. This is often noticed at social occasions. I feel isolated as unable to join in
One respondent commented: “I feel help with better hearing of music will improve my quality of life through lifting depression and giving relief and inspiration and some lifting of loneliness”. Potential impacts on quality of life appeared to be particularly salient for those with musical training and who played instruments: “As a musician and conductor the discernment of sound quality, pitch and balance are crucial. As a result of the deficit I have become frustrated and depressed”; “I now feel scared of playing live gigs”.
Discussions about music listening in the clinic: hearing-aid users
Hearing-aid users were asked whether they had ever discussed music in clinic. The majority (58%) reported that they had “Never” spoken with their audiologist about music listening, whilst roughly a quarter (23%) had held “More than one” discussion. A far smaller number (4%) reported that they were “Planning to” discuss music (see ). Of those who had discussed music in clinic at least once, 42% gave very low ratings for improvements, indicating that discussions do not always facilitate useful interventions (see ).
Figure 4. Frequency of discussions in clinic across all participants (a [n = 173]) and degree to which this has improved music listening experiences among those who had discussed music at least once ( b [n = 50]).
![Figure 4. Frequency of discussions in clinic across all participants (a [n = 173]) and degree to which this has improved music listening experiences among those who had discussed music at least once ( b [n = 50]).](/cms/asset/4aedb0cf-fb0b-49b5-949a-4899a6c536e3/iija_a_1762126_f0004_b.jpg)
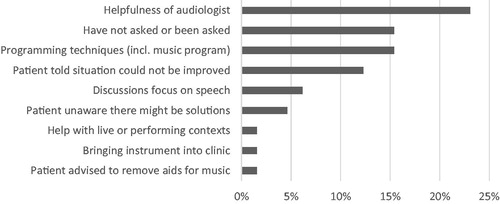
The most prevalent theme coded in the qualitative responses was the helpfulness of audiologists to try and address issues with music (): “Although I have only asked the question on music once, my wife and I are thoroughly pleased with the helpfulness and patience found in my audiologist”; “I am trying different aids under the guidance of my audiologist, who is adjusting the ‘music’ programme in an effort to make it more acceptable”; “The audiology department has been very good to me, allowing me to try a range of hearing aids, inner and behind the ear”. Examples were given of adjustments made to hearing aids that led to improvements:
Figure 5. Have you ever talked to your audiologist about music listening? Thematically coded responses (n = 65, percentages sum >100% as participants contributed to >1 theme).
The audiologist set one of my hearing-aid programs to have no feedback so that it does not attenuate very loud sounds. This enables me to enjoy as much as is possible, for example, the full dynamic range of a Mahler symphony
“With the music program, it is very clear and good”.
There were several reasons specified for why music was not discussed in clinic, which included a focus on speech perception as a priority: “Never come up in appointments”; “Never thought about talking about it, plus they have never mentioned about music to me”; “Music is very important to me but I have other problems related to hearing loss which have been more important to address to enable me to function in daily life”. There was acknowledgement that adjustments can complex and time consuming: “Due to him taking time and experimenting, the margin between having a successful music listening hearing-aid setting and having undesirable oscillation in the form of a constant whistle is quite fine”; and involve compromise: “I have had bi-lateral aids for 20+ years and despite digital aids being an improvement there is still a limitation as to what I hear properly”. For some, clinical fitting strategies were unsuccessful: “All the hearing aids I have tried, and with all the different settings audiology have tried, I still struggle to appreciate music like I used to”; “The problems I have seem to be an unsolvable problem in otherwise excellent hearing aids”.
Discussions about music listening in the clinic: audiologists
Audiologists were asked about the percentage of patients who ask about music listening issues (). Nearly half (46%) reported that 1 in 10 or fewer patients ask about music, and a further quarter (25%) of audiologists reported that 1 in 5 (or fewer) patients ask about music (). Overall, 85% reported that they had discussed music with patients (indicated through a “yes”/“no” response), though there was variation in the frequency of discussions taking place. Some audiologists (13%) reported asking as many as 4 out of 5 patients about music, however, half reported that they ask 1 in 5 patients or fewer ().
Figure 6. Percentage of patients who ask about issues related to music listening (a [n = 93]), and percentage of practitioners who report they ask patients about music in clinic (b, [n = 87]).
![Figure 6. Percentage of patients who ask about issues related to music listening (a [n = 93]), and percentage of practitioners who report they ask patients about music in clinic (b, [n = 87]).](/cms/asset/8ca933c0-08db-45ad-89e6-e6329a856b4e/iija_a_1762126_f0006_b.jpg)
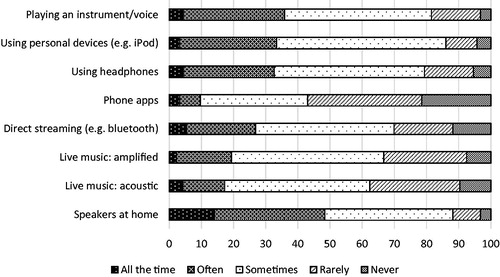
Audiologists were asked how frequently they discussed various topics about music from a list of pre-determined categories (). The most common topics discussed with patients were listening through speakers at home and playing an instrument/voice. The topic of “phone apps” for music listening were the least likely to be discussed, and live contexts were not often discussed. The modal response for all categories was “Sometimes” indicating that no one topic area is being discussed routinely with patients.
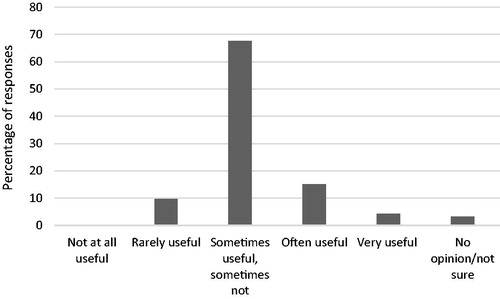
When asked to rate the usefulness of hearing aids for music listening, the majority (68%) responded “Sometimes useful, sometimes not”, reflecting the sentiment from users themselves. A small percentage of audiologists reported that hearing aids were “Often” (15%) or “Very” (4%) useful (see ).
Programming hearing aids for music listening
Audiologists were asked whether they felt confident in providing general advice about music listening. The majority (59%) reported some confidence in providing advice about music while 24% were “not sure” and 17% were “quite reluctant” (). A similar pattern was found regarding confidence in programming a hearing-aid for music. Over half (57%) reported that they were confident in programming a hearing-aid for music, but 25% were not sure, and 18% were reluctant or would not attempt this at all ().
Figure 9. Rated confidence in providing advice about music listening (a [n = 93]) and confidence fitting a music listening programme on hearing aids (b [n = 93]).
![Figure 9. Rated confidence in providing advice about music listening (a [n = 93]) and confidence fitting a music listening programme on hearing aids (b [n = 93]).](/cms/asset/8410bd09-4a48-4c31-8c07-6678c58e8c52/iija_a_1762126_f0009_b.jpg)
Eighty-one percent reported that they made adjustments to hearing aids for music listening other than selecting a manufacturer-defined music programme (indicated through a “yes”/“no” response). A quarter reported having programmed hearing aids for music for more than 10 years, but years of experience varied between audiologists, with around a third having modified listening programmes for music for less than two years (). As shows, 30% of audiologists reported that they provide volume control with a further 67% reporting that they did this “Sometimes”.
Specific fitting strategies
53 audiologists gave examples of the types of adjustments they made to hearing aids for music and analysis has enabled themes in programming to be identified (see ). The most commonly cited strategy was disabling automatic functions designed for speech or speech in noise (e.g. “switching off all adaptive parameters”, “remove adaptive features”), which included turning off automated noise management (e.g. “I have been turning off noise reduction features”, “reducing or turning off features such as whistleblock, echoblock, windblock etc.”), disabling feedback management systems (e.g. “remove feedback management”, “turning off feedback measures”), and adjustments to microphone directionality (e.g. “omnidirectional”, “disable directional microphones”). Adjusting compression characteristics was the next most frequently reported strategy. However, few audiologists gave sufficient detail to clarify the exact nature of changes made (e.g. “change compression settings”, “changing compression type”) and therefore it was unclear if responses were referring to compression speeds (e.g. slow vs fast acting compression) or linear/non-linear strategies (i.e. attempting to optimize compression ratios for prescription of gain across frequency based on patient feedback). A small number of responses were consistent with altering compression ratios (e.g. “reduce compression ratio”, “manipulating compression ratios”) but typically these responses did not specify the nature of changes in relation to frequency response and to which input levels these were applied. Some suggested global changes to compression which again did not contain sufficient consistency in terminology to identify a definitive consenus in applied strategy across practitioners, that is, making hearing aids more linear, softening the compression kneepoint or reducing or removing compression (e.g. “reduce compression”, “turning off compression”).
Figure 11. Strategies for programming hearing aids. Thematically coded responses (n = 53, percentages sum >100% as participants contributed to >1 theme).
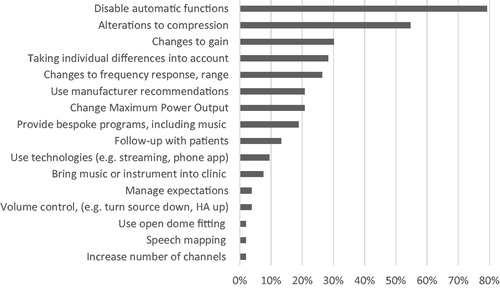
The potential effects of frequency compression were reported by just over half, and this was more clearly defined by respondents who specified removing this feature: “Typically first approach is to try without frequency compression as this alters the pitch for some frequencies and therefore notes. Secondly changing knee points and compression strategies”. The next most common adjustment reported was changes to gain. Reports evidenced a variety of different approaches: “increase gain in higher frequencies”; “low mid gain increases”; “reduce overall gain”; “increase gain for loud levels”; “decrease gains for loud levels”.
Overall however, there was a lack of detail in terminology around the specific increase or reduction in gain, the degree of change, how changes were applied across frequency and for differing input levels, and how this interacted with applied changes to compression ratios. As changes to gain for different input levels will inherently affect compression ratios, this lack of detail prevented further systematic analysis.
Many audiologists acknowledged that there is no “one-size-fits-all” approach: “You need to change setting to suit the type of music […] this can change from person to person and can take time to get right”; “Important to know situations and lifestyle of each patient”; “I would tailor the fitting strategy based on the patients reports of the type of music listening they do, their concerns and desires”. Many also reflected in the comments about the importance of regular follow-up appointments to check if adjustments are needed.
A range of other strategies reported included using the manufacturer’s predefined “music” settings (e.g. “Use manufacturers’ pre-set programs for music”, “normally provide hearing-aid provider’s programme for music”). Some noted they would alter Maximum Power Output (MPO), and again there was a variety of approaches adopted but a lack of detail in sufficiently describing these changes (e.g. “raise MPO levels marginally”, “MPO increase”, “lowering MPO”). Only four audiologists noted that they would ask patients to bring music or their instrument to the clinic:
Very, very occasionally I’ll ask patients who are really struggling to either sing or bring their instrument to see if its possible to ask the right questions and get them to listen to the sound and see if they can pinpoint what’s resonating too much for them, or drowning out particular sounds
Music-specific training and resources for audiologists
Just over a third (37%) of audiologists had received some form of training on the subject of music listening and 63% had not. Of those that had received some form of training, the majority had received this at a conference or Continuing Professional Development (CPD) event, with only a small number of audiologists reporting that it had been part of their curriculum training. Thematic coding of open-ended responses () revealed a cluster around manufacturer-led and academic conference events (e.g. “manufacturer held two specific events with invited speakers from the music industry”; “Various conferences nationally (British Society of Audiology, British Academy of Audiology) and internationally (American Academy of Audiology)”) and some in-curriculm training (e.g. “Info about the attack and release time, noise management of aid, directionality”), though curriculum training included courses outside of audiology such as sound engineering and music technology.
Figure 12. What kind of training relating to music listening did you receive? Thematically coded responses (n = 35, percentages sum >100% as participants contributed to >1 theme).

A number of associations revealed the positive impact of any kind of training received. Those who had received training were more likely to report feeling confident providing advice about music listening (χ2 (2) = 11.652, p = 0.003), to have more years’ experience in programming hearing aids for music (χ2 (2) = 11.214, p = 0.004), and to be programming hearing aids for music for a greater number of patients (χ2 (1) = 6.035, p = 0.014).
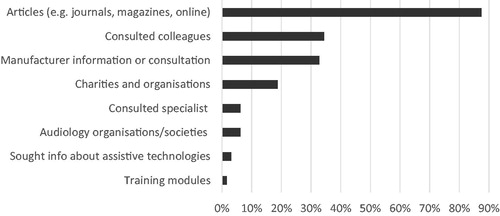
74% (69 out of 93) of audiologists said they had sought information on music listening solutions. highlights themes found in the free-fill responses completed by 65 of the audiologists, showing that the most frequent sources of information were journals, magazines or online resources, consultation with colleagues, and manufacturer information.
Figure 13. Information sought about music listening for patients. Thematically coded responses (n = 35, percentages sum >100% as participants contributed to >1 theme).
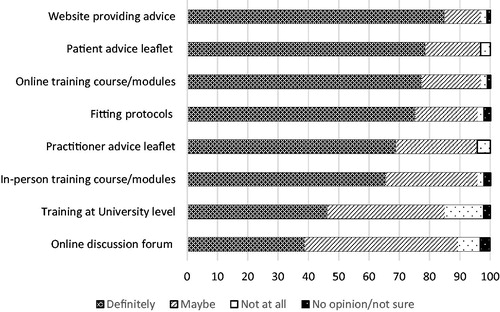
When asked what resources they would find useful, the highest rated were “website providing guidance” (85% would definitely use), “a patient advice leaflet” (79%), “online training course/modules” (77%), fitting protocols (75%), and “a practitioner advice leaflet” (69%) (). Finally, when asked whether they would use/give out a patient information leaflet on the subject of music listening if it was provided, 41% reported “Yes, all the time”, 38% “Probably”, 17% “If needed”, and only 4% reported that it was unlikely that they would hand a leaflet out.
Discussion
The present results reflect the existing understanding that whilst hearing aids can be helpful for music listening, many listeners experience problems. Issues identified here include poor sound quality, difficulties hearing words in songs, distortion, and feedback, and difficulties in live contexts and these have been identified in previous research (e.g. Leek et al. Citation2008; Looi, Rutledge, and Prvan Citation2019; Madsen and Moore Citation2014; Vaisberg et al. Citation2019). Audiologists corroborated this, the majority reporting that hearing aids were “sometimes useful, sometimes not”.
Relatively few discussions about music were found to be taking place in the clinic. 58% of hearing-aid users had never had a discussion about music listening, 50% of audiologists reported that they ask 1 in 5 (or fewer) patients about music, and a larger majority (72%) said that fewer than 1 in 5 patients ask them about music. This is most likely due to the context that the primary purpose of audiological practice and hearing-aid technology is to facilitate aural, verbal communication, not music perception. Hearing-aid users’ quantitative data suggest that discussions about music listening rarely lead to positive outcomes, yet qualitative data revealed a high sense of satisfaction with their audiologists, indicating that in spite of challenges with outcomes with regard to music listening, audiology patients are receiving good overall experiences in clinic.
The range of fitting strategies reported by audiologists appears to be congruent with advice in the literature. Audiologists frequently reported disabling various automatic functions for music perception. In musical contexts, it is likely that this over-arching strategy may prevent sustained-tone stimuli (e.g. organ, flute) being mistakenly analyzed as feedback and suppressed, and similarly disabling noise/wind management may reduce musical stimuli being interpreted as unwanted sound (Chasin and Hockley Citation2012, Citation2014). Reports around other adaptive functions were varied. Selecting a fixed microphone directionality may allow a better focus on music in live settings but in other music listening situations, omni-directionality may be advantageous. Likewise, reports from hearing-aid users in this study were mixed, indeed some reported that feedback cancellation was helpful in musical settings. The data supports the idea that there is no “one-size-fits-all” approach, and that the adjustment of automatic functions should be driven by consideration of users’ individual needs.
While 30% of audiologists reported providing volume control, far fewer (4%) volunteered that they make adjustments to volume as part of a programming strategy for music listening. Nonetheless, providing volume control to patients is likely to be beneficial. Another common adjustment reported was altering gain and compression. Many hearing-aid users reported problems with volume/dynamics, in particular, issues hearing high frequencies, and so it is perhaps unsurprising that audiologists were adjusting gain frequently. Research has shown that slow-acting WDRC or linear amplification is preferred by some hearing-aid users for music listening (Croghan, Arehart, and Kates Citation2014; Madsen et al. Citation2015; Moore and Sęk Citation2016), perhaps because it does not flatten the dynamic range and avoids modulation of foreground sound.
Given the frequency with which audiologists reported applying these strategies, these are likely to be tried and tested, though systematic research is needed. The lack of technical detail provided by audiologists in this study about the specific nature of changes made means that it is not possible to provide more technical interpretation of the effects of combined acoustic changes. The limited range of terminology used may have reflected the range of experience of audiologists (a third of the sample had only been practising for a few years). Furthermore, some of the commercially available software for fitting does not allow audiologists to know exactly how changes to programming are applied within a given algorithm, so caution is needed in generalizing about their impact. Changes to gain for different input levels will inherently affect compression but this was typically reported by audiologists simply as “gain changes”. This again highlights the need for in-depth laboratory and field-based research to support an evidence base for programming changes for music, linking adaptations in acoustic parameters to measurable improvements in outcome, whether independently or within strategies in line with speech perception prescriptive tools.
Research into practice: the case for audiologist training
Despite there being relatively few discussions about music in the clinic, there was evidence of good confidence among clinical practitioners about music listening issues. Roughly 60% reported at least some degree of confidence in providing advice about music listening and in fitting a music programme, and 57% reported at least some confidence in programming hearing-aids for music. However, nearly half were “not sure” or reluctant to provide advice or programme a hearing-aid for music, and most (60%) reported that they programme a hearing-aid for music for fewer than 1 in 10 patients. This suggests that there is room to increase clinical audiology activity around music listening and training may have a key role to play in increasing confidence in doing so.
Training on music for audiologists was found to include both formal and informal channels, in particular attendance at conferences, and was related to increased confidence in providing advice about music listening and in programming hearing aids for music. While causal links cannot be inferred, it is likely that relevant, topic-specific training is a precursor to confidence in discussing, advising and fitting for music in the clinic, supporting the relationship between training and years’ experience programming hearing aids for music. These data present a strong case for more formalized methods of training, benefiting larger numbers of audiologists, especially given the appetite for such training: 74% had already sought information, and more than two-thirds would “definitely” use resources such as fitting proposals or patient/practitioner advice leaflets. It is essential that the development of evidence-based, validated guidelines to support training is underpinned by empirical research into fitting strategies and, crucially, their relationship to beneficial outcomes for users.
Training in fitting cannot address the inherent limitations of hearing-aid technology with respect to the amplification of music but can provide strategies to maximize its potential. There is evidence from the literature on musical aural rehabilitation with cochlear implant users that despite limitations of cochlear implant technology for music perception such as poor pitch and melodic discrimination (Limb and Roy Citation2014; Looi and She Citation2010; Drennan et al. Citation2015) there are beneficial effects of training on musical appreciation (Looi, Wong, and Loo Citation2016; van Besouw et al. Citation2014). Recently, Looi (Citation2018) provides recommendations for cochlear implant users and audiologists to improve outcomes for music, and the current study suggests similar guidance is needed for hearing-aid technology. Music often carries higher emotional significance for listeners than speech stimuli, and so aural rehabilitation journeys may be longer, and more emotionally traumatic (Einhorn Citation2012). Hearing-aid users in the present study reflect this, including negative psychosocial consequences such as anxiety, depression, and social isolation and exclusion as a direct result of disengaging with music.
Limitations and further research
There were a number of limitations to the present surveys. To maximize responses, Study 1 was designed to be completed in the clinic in under 5 minutes which limited the depth and scope of the inquiry. Patients were not asked about the purpose of their visit (e.g. whether a new or repeat visit or for a particular issue) or about various more detailed aspects of their hearing-aid use (e.g. whether they wear one/two, how long they have worn aids for, what style, fitting experiences). Patients’ audiometric profiles were not obtained which limited the ability to associate problems experienced with the level and type of hearing impairment.
The current results do not tell us which strategies and adjustments in the clinic lead to improved music listening experiences, and programming strategies reported by audiologists were not sufficiently well defined to provide in-depth analyses. Further research is needed that systematically explores associations between reported problems and hearing loss level and configuration and/or hearing-aid technology. This includes the implementation of manufacturer music programmes and impartial evaluation of their efficacy in different listening settings.
Systematically linking clinical interventions with patient outcomes will enable researchers to test and evaluate the effectiveness of different strategies. In turn, this knowledge can inform the creation of practioner training and guidelines which will likely increase confidence and the prevalence of discussions about music (alongside speech) in the clinic. A clinical outcome measure for music listening could be developed and validated, taking into account hearing-aid users’ various perceptual needs and facilitating the mapping of problems experienced and improvements over time. Supported by new technologies and data collection methods, longitudinal studies could track new hearing-aid users, mapping their experiences, real-time adjustments made, and subsequent outcomes. Improvements to music-listening outcomes may help address the low- or non-use of hearing aids by people who have been fitted with them (currently estimated to be between 5 and 24%, McCormack and Fortnum Citation2013) and even influence non-user adoption for the 3 out of 4 individuals who would benefit from a hearing-aid but do not adopt them (Kochkin Citation2007). Developing advice leaflets that help hearing-aid users adapt to music listening with hearing aids and provide audiologists with counselling and fitting tools, could improve patient awareness of the potential for hearing aids to support music listening, and audiologists’ confidence in raising these issues in the clinic.
Conclusions
Results indicate that the prevalence of conversations about music in the clinic remains low and attempts to programme hearing aids for music are currently mixed. The results indicate that even a small amount of training and knowledge, such as a one-off CPD event or conference, is associated with positive impacts in the clinic, increasing clinician confidence in programming hearing aids for music and the prevalence of their attempts to do so. There is a significant opportunity, therefore, to increase the evidence base relating clinical strategies with patient outcomes that would enable discussions in the clinic to be more effective. Such further research would also support the development of practitioner training.
The results also show that hearing aids can be problematic for music for two-thirds of hearing-aids users. As hearing aids are not expressly designed to amplify music, the diverse range of experiences reported is perhaps to be expected. Reports that problems with music listening negatively affected the quality of life or even led to disengagement with music listening or participation were found alongside reports that hearing aids are indispensable. Nonetheless, there remains a clear scope for improving hearing-aid amplification of music. It is likely that emerging technologies will revolutionize both patient and practitioner outcomes, and the use of personalized data may alter the role of the clinician into the future.
Acknowledgements
The authors thank Harley Street Hearing, the British Academy of Audiology (BAA) for assistance with recruitment, Matthew Frost for his research on the taught content of audiology courses, and Amy Beeston for helpful comments and discussion.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Note
Additional information
Funding
Notes
1 We adopt the convention that ‘deaf’ refers to the physical condition of deafness and ‘Deaf’ refers to those who identify with the Deaf community and culture.
References
- Action on Hearing Loss. 2015. “Hearing Matters.” AHL. https://www.actiononhearingloss.org.uk/-/media/ahl/documents/research-and-policy/reports/hearing-matters-report.pdf. Accessed 05/05/2020
- Beck, D. L. 2014. “Issues and Considerations regarding Musicians, Music, Hearing and Listening.” Hearing Review 21 (8): 14–16.
- Beck, D. L. 2016. “Music, Sound Quality, and Hearing Aids: An Interview with Brian Moore and Richard Einhorn.” Hearing Review 23 (7): 38.
- Cai, Y., F. Zhao, and Y. Zheng. 2013. “Mechanisms of Music Perception and Its Changes in Hearing Impaired People.” Hearing, Balance and Communication 11 (4): 168–175. doi:10.3109/21695717.2013.839356.
- Chasin, M. 2010. “Six Ways to Improve Listening to Music through Hearing Aids.” Hearing Journal 63 (9): 27–30. doi:10.1097/01.HJ.0000388537.27405.77.
- Chasin, M. 2012. “Hearing Aids and Music.” Audiology Practices 4 (2): 8–13.
- Chasin, M. 2018. “Using Audiology to Extend a Musician’s Career.” Hearing Review 25 (10): 10.
- Chasin, M., and Hockley, N. S. 2012. “Special Issue on Music and Hearing Loss: Preventative and Rehabilitative Options.” Trends in Amplification 16 (3), 135–182. doi:10.1177/1084713812464910.
- Chasin, M., and N. S. Hockley. 2014. “Some Characteristics of Amplified Music through Hearing Aids.” Hearing Research 308: 2–12. doi:10.1016/j.heares.2013.07.003.
- Chasin, M., and F. A. Russo. 2004. “Hearing Aids and Music.” Trends in Amplification 8 (2): 35–47. doi:10.1177/108471380400800202.
- Croghan, N. B. H., K. H. Arehart, and J. M. Kates. 2014. “Music Preferences with Hearing Aids: Effects of Signal Properties, Compression Settings, and Listener Characteristics.” Ear & Hearing 35: 170–184.
- Drennan, W. R., J. J. Oleson, K. Gfeller, J. Crosson, V. D. Driscoll, J. H. Won, E. S. Anderson, and J. T. Rubinstein. 2015. “Clinical Evaluation of Music Perception, Appraisal and Experience in Cochlear Implant Users.” International Journal of Audiology 54 (2): 114–123. doi:10.3109/14992027.2014.948219.
- Einhorn, R. 2012. “Observations from a Musician with Hearing Loss.” Trends in Amplification 16 (3): 179–182. doi:10.1177/1084713812468513.
- Fulford, R., J. Ginsborg, and J. Goldbart. 2011. “Learning Not to Listen: The Experiences of Musicians with Hearing Impairments.” Music Education Research 13 (4): 447–446. doi:10.1080/14613808.2011.632086.
- Fulford, R., J. Ginsborg, and A. Greasley. 2015. “Hearing Aids and Music: The Experiences of D/Deaf Musicians.” Paper presented at the Ninth Triennial Conference of the European Society for the Cognitive Sciences of Music, Manchester, UK, August 17–22.
- Kirchberger, M. J., and F. A. Russo. 2015. “Development of the Adaptive Music Perception Test.” Ear and Hearing 36 (2): 217–228. doi:10.1097/AUD.0000000000000112
- Kochkin, S. 2007. “MarkeTrak VII: Obstacles to Adult Non-User Adoption of Hearing Aids.” Hearing Journal 60 (4): 24–51. doi:10.1097/01.HJ.0000285745.08599.7f.
- Lamont, A., A. E. Greasley, and J. A. Sloboda. 2016. “Choosing to Hear Music: Motivation, Process and Effect.” In Oxford Handbook of Music Psychology. 2nd edition, edited by S. Hallam, I. Cross, and M. Thaut, 711–724. Oxford, UK: Oxford University Press.
- Leek, M. R., M. R. Molis, L. R. Kubli, and J. B. Tufts. 2008. “Enjoyment of Music by Elderly Hearing-Impaired Listeners.” Journal of the American Academy of Audiology 19 (6): 519–526. doi:10.3766/jaaa.19.6.7.
- Limb, C. J., and A. T. Roy. 2014. “Technological, Biological, and Acoustical Constraints to Music Perception in Cochlear Implant Users.” Hearing Research 308: 13–26. doi:10.1016/j.heares.2013.04.009.
- Looi, V. 2018. “The Sound of Music for Adult Cochlear Implant Recipients.” ENT & Audiology News 25 (4): 80–84.
- Looi, V., and J. She. 2010. “Music Perception of Cochlear Implant Users: A Questionnaire, and Its Implications for a Music Training Program.” International Journal of Audiology 49 (2): 116–128. doi:10.3109/14992020903405987.
- Looi, V., K. Gfeller, and V. Driscoll. 2012. “Music Appreciation and Training for Cochlear Implant Recipients: A Review.” Seminars in Hearing 33 (4): 307–334. doi:10.1055/s-0032-1329222.
- Looi, V., Y. Wong, and J. H. Y. Loo. 2016. “The Effects of Training on Music Perception and Appreciation for Cochlear Implant Recipients.” Advances in Otolaryngology 2016: 1–12. doi:10.1155/2016/6286514.
- Looi, V., K. Rutledge, and T. Prvan. 2019. “Music Appreciation of Adult Hearing Aid Users and the Impact of Different Levels of Hearing Loss.” Ear and Hearing 40 (3): 529–544. doi:10.1097/AUD.0000000000000632.
- McCormack, A., and H. Fortnum. 2013. “Why Do People Fitted with Hearing Aids Not Wear Them?” International Journal of Audiology 52 (5): 360–368. doi:10.3109/14992027.2013.769066.
- Madsen, S. M., and B. C. Moore. 2014. “Music and Hearing Aids.” Trends in Hearing 18: doi:10.1177/2331216514558271.
- Madsen, S. M., M. A. Stone, M. F. McKinney, K. Fitz, and B. C. Moore. 2015. “Effects of Wide Dynamic-Range Compression on the Perceived Clarity of Individual Musical Instruments.” Journal of Acoustical Society of America 137 (4): 1867–1876. doi:10.1121/1.4914988.
- Moore, B. C. J. 2016. “Effects of Sound-Induced Hearing Loss and Hearing Aids on the Perception of Music.” Journal of the Audio Engineering Society 64 (3): 112–123. doi:10.17743/jaes.2015.0081.
- Moore, B. C., and A. Sęk. 2016. “Preferred Compression Speed for Speech and Music and Its Relationship to Sensitivity to Temporal Fine Structure.” Trends in Hearing 20: doi:10.1177/2331216516640486.
- Revit, L. J. 2009. “What’s so Special about Music?” Hearing Review 16 (2): 12–19.
- Tozer, C., and H. Crook. 2012. “Music Listening With Hearing Aids: A Review of the Literature.” Poster presented at the Music Mind Machine in Sheffield Launch Event, Sheffield, UK, November 27.
- Schäfer, T., P. Sedlmeier, C. Städtler, and D. Huron. 2013. “The Psychological Functions of Music Listening.” Frontiers in Psychology 4: 1–33. doi:10.3389/fpsyg.2013.00511.
- Uys, M., and C. van Dijk. 2011. “Development of a Music Perception Test for Adult Hearing-Aid Users.” South African Journal of Communication Disorders 58 (1): 19–47. doi:10.4102/sajcd.v58i1.38.
- Vaisberg, J. M., A. T. Martindale, P. Folkeard, and C. Benedict. 2019. “A Qualitative Study of the Effects of Hearing Loss and Hearing Aid Use on Music Perception in Performing Musicians.” Journal of the American Academy of Audiology 30 (10): 856–870. doi:10.3766/jaaa.17019.
- van Besouw, R. M., D. R. Nicholls, B. R. Oliver, S. M. Hodkinson, and M. L. Grasmeder. 2014. “Auditory Rehabilitation through Music Workshops for Cochlear Implant Users.” Journal of the American Academy of Audiology 25 (4): 311–323. doi:10.3766/jaaa.25.4.3.


![Figure 10. Years’ experience in programming hearing aids for music (a [n = 79]), and percentage of patients that practitioners programme a music programme for (b [n = 80]).](/cms/asset/329d85e8-3a72-40bc-a86c-b9f63f563b4d/iija_a_1762126_f0010_b.jpg)