Abstract
Objective
Although the availability of mobile device applications (apps) to support people with hearing impairment is rapidly increasing, there are few reports of the use of such apps by the target population. The aim of this paper is to describe research that has applied apps at various stages of the adult rehabilitation journey.
Design
A summary of studies utilising apps to investigate (1) the hearing difficulties and acoustic environments of adults with mild hearing impairment, (2) hearing aid benefit in this population and (3) useability of an app to guide hearing aid handling tasks.
Study sample
Older adults with no previous experience with hearing aids, who owned a smartphone or tablet and were confident in using apps. Participant samples ranged from 10 (hearing aid benefit pilot study, mean age = 70 years) to 30 participants (app useability study, mean age = 69 years).
Results
All studies showed that smartphone apps can provide real-world insights during the early stages of the patient journey and hearing aid management support during the latter stages. App useability was rated positively by participants.
Conclusion
Smartphone apps may be used as a feasible complement to face-to-face interaction in audiology practice.
Introduction
Age-related hearing impairment is among the most common chronic conditions of aging (Simpson, Simpson, and Dubno Citation2015). Contemporary approaches in the management of chronic health conditions including hearing impairment promote the concept of person-centred care (e.g. Grenness et al. Citation2014a), where individuals with chronic conditions work in partnership with health professionals, encouraging shared decision-making and the patient’s self‐management of the condition. Self‐management refers to the ability of the person with the health condition to manage symptoms, treatment, lifestyle and psychosocial changes related to the care of an ongoing medical condition (Barlow et al. Citation2002).
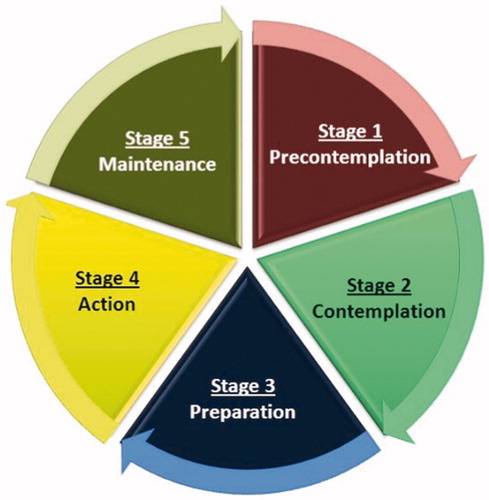
In reviewing the processes involved in self-management, Lorig and Holman (Citation2003) suggested self-management encompassed several stages: problem solving, decision making, utilising resources, partnering with healthcare providers, taking action, and improving self-efficacy. These processes are strongly aligned with the phases associated with the so-called “patient journey” in audiologic rehabilitation, which has been defined in several ways. For example, Stephens and Kramer (Citation2009) suggest a patient journey of enablement with several stages; evaluation, integration and decision making, short-term remediation, ongoing remediation and outcome assessment (134). Several studies have applied a transtheoretical model of behaviour change (Prochaska, Johnson, and Lee Citation2009) and identified a journey with stages-of-change of pre-contemplation, contemplation, preparation, action, and maintenance (Laplante-Lévesque, Hickson, and Worrall Citation2013; Ekberg, Grenness, and Hickson Citation2016). In creating a framework and tool to facilitate audiologic rehabilitation, Gregory (Citation2012) identified a patient journey incorporating seven phases: pre-awareness, awareness, movement, diagnostics, rehabilitation, and postclinical. Given that the provision of hearing aids is the most common intervention for acquired, or adult-onset, hearing impairment (Chisolm, Abrams, and McArdle Citation2004; Timmer, Hickson, and Launer Citation2015; Ferguson et al. Citation2017), others have simplified the patient journey to the more device-centric path of pre-fitting, fitting and post-fitting (e.g. Manchaiah et al. Citation2013; Paglialonga et al. Citation2018). Although the stage descriptors in the various models differ, all approaches to describing the patient journey incorporate different phases and processes which are supported by person-centred, collaborative care between clinicians and patients and aim to foster self-management.
In the context of hearing care, self-management has been shown to result in improved collaboration and decision-making between the individual and the clinician (Taylor Citation2020) and improved outcomes such as greater hearing aid benefit and satisfaction (Convery et al. Citation2019). Aside from counselling and instruction delivered by clinicians face-to-face in a clinical setting and printed materials such as hearing aid user guides, the use of multimedia resources such as videos and illustrations may also support self-management during the patient journey. For example, a recent randomised controlled trial by Gomez and Ferguson (Citation2020) with 56 first-time hearing aid users showed greater improvement in hearing aid management and knowledge for participants who viewed DVD-based or online educational hearing aids management content compared to participants who received a printed booklet on hearing aids. Such multimedia educational content can also be embedded in other sources, such as mobile device applications (apps), to support self-management (Paglialonga, Tognola, and Pinciroli Citation2015). Of course, apps are only of benefit for those who own mobile devices such as smartphones. Evidence shows that smartphone ownership is increasing worldwide, in particular for older adults. For example, smartphones are owned by 73% of people in the U.S. between the ages of 50 and 64 years and 46% of people aged 65 years and over (Pew Research Center Citation2018). In Australia, the statistics are higher; 90% of people between the ages of 65 and 74 years, and 84% people of 75 years of age and over, owned a smartphone as of July 2019 (Statista Citation2020). App usage is also rising and demographic usage statistics show that adults over the age of 65 years spend about 1 h 43 min a day on apps (Iqbal Citation2020).
As with smartphone ownership, the availability of mobile device apps designed for older adults with hearing impairment is rapidly increasing. Paglialonga, Tognola, and Pinciroli (Citation2015) identified 203 apps targeting hearing care professionals and/or individuals with hearing impairment covering various aspects of the patient journey: hearing impairment screening and assessment, intervention and rehabilitation, education and information, and assistive tools. The study concluded that apps may be a viable means of meeting the needs of some individuals with hearing impairment but further research is needed to assess the viability and effectiveness of such apps. In a follow-up study reviewing 120 apps related to hearing and hearing impairment, Paglialonga, Pinciroli, and Tognola (Citation2017) suggested that developers should take into account the particular useability needs of older adults in setting-up and using apps.
Reviews and useability studies of general apps for older adults have suggested that the take-up is low because the apps are not designed with the older adult in mind (Fisk et al. Citation2009; Plaza et al. Citation2011; Wildenbos, Peute, and Jaspers Citation2018). Paglialonga et al. (Citation2018) agreed with this and highlighted the dearth of literature evidencing the use and benefit of mobile apps to support the hearing rehabilitation journey. Both Bright and Pallawela (Citation2016) and (Swanepoel et al. Citation2019) agree that further validation of apps as suitable for clinical purposes is required. This paper aims to highlight some of the authors’ research which included the use and validation of apps with older adults and how such apps could support the patient journey using the stages-of-change (Ekberg, Grenness, and Hickson Citation2016) of contemplation and preparation, action, and maintenance ().
Supporting contemplation and preparation
The early stage in the patient journey involves processes such as awareness of a hearing impairment, contemplation about what might be done about the hearing impairment, and preparation for, and decision-making about, which intervention/s to try (Stephens & Kramer, Citation2009; Ekberg, Grenness, and Hickson Citation2016). As Oh and Lee (Citation2016) suggest, clinicians can support patients on this journey by means of assessing hearing status, functional difficulties, and intervention candidacy and by selecting appropriate intervention options. Although individuals can access and download smartphone apps that provide self-tests with accurate hearing screening (Barczik and Serpanos Citation2018; Margolis et al. Citation2018), it is recognised that objective hearing tests and audiometric thresholds do not motivate help-seeking as much as subjective or self-reported functional hearing ability (Meyer and Hickson Citation2012; Alicea and Doherty Citation2017).
We have previously published studies describing the use of smartphone apps to explore the functional hearing difficulties of older adults. Using an Ecological Momentary Assessment (EMA) app, 29 adults (mean age = 69 years) with mild hearing impairment reported their experiences in common real-world listening events (Timmer, Hickson, and Launer Citation2017). EMA is a methodology that uses surveys to document current experiences in real time and at multiple times per day. While paper-and-pencil EMA surveys and daily diaries were used in the past, the surveys are nowadays often incorporated in apps installed on smartphones, as this approach increases participant compliance by means of reminders and pre-defined survey-initiation triggers (Stone et al. Citation2002). Over a 2 week period, Timmer, Hickson, and Launer (Citation2017) asked participants who were non-hearing aid users to describe listening activities they were in and characteristics of the sound environment, and rate their speech understanding and listening effort in those situations. The results showed the participants’ most common listening situations were in the home, either in conversation with three or fewer familiar speakers or listening to TV or radio. Participants reported high levels of subjective speech understanding and in 91% of the 962 speech-listening event surveys collected in the study, they rated their percentage understanding of speech as either 75% or 100%. However, in two-thirds of these speech-listening situations, the participants indicated that listening effectively required some degree of effort (Timmer, Hickson, and Launer Citation2018). Other researchers have also highlighted the detrimental effects of hearing impairment for listening effort (e.g. Picou, Ricketts, and Hornsby Citation2013; Ohlenforst et al. Citation2017) but this is typically for adults with more severe degrees of hearing impairment than those in this study.
While the use of EMA can provide rich data for research purposes, it may also provide relevant insight for clinical practice. The data from the EMA app described in Timmer, Hickson, and Launer (Citation2017) showed the variability in individuals’ listening situations, and their hearing ability in those situations. Using EMA with individual patients could serve to raise awareness of hearing difficulties in everyday life and this insight into functional hearing ability may be the driver or motivator required to take the next step in the rehabilitation journey. Furthermore, the information gleaned from the app may facilitate shared decision-making with the clinician as both can discuss these experiences and consider solutions together. People with hearing impairment report that receiving such “individualized” care is a fundamental aspect of person-centred care (Grenness et al. Citation2014a).
EMA data can also indicate if the patient is a candidate for hearing aids or other hearing impairment intervention options. For example, knowing that the individual reports reduced speech understanding and considerable listening effort during a listening situation common and important to them, allows the clinician insight into if (and to what degree) hearing aids could address that specific listening situation. It also provides a base for goal-setting beyond improved speech understanding, and targeting benefits such as reduced listening effort. Additional information, such as the familiarity and number of speakers in the individual’s typical listening situations may point towards the need for additional communication strategy education. Beyond these early stages of awareness raising and decision making, our next question was whether or not smartphone EMA apps could be used to assess the outcome of hearing aid provision and communication strategies during the action or intervention stage of the patient journey?
Supporting the action stage
Hearing aids are the most common intervention for acquired, or adult-onset, hearing impairment (Chisolm, Abrams, and McArdle Citation2004; Timmer, Hickson, and Launer Citation2015; Ferguson et al. Citation2017). Successful self-management for adults with hearing impairment therefore often entails the ability to use and manage hearing aids and measuring hearing aid outcomes. Research indicates however that hearing aid outcomes are not easy to assess due to the complexity of what hearing aid success entails and the divergence of outcome measures (Saunders, Chisolm, and Abrams Citation2005; Humes Citation2006). As Poost-Foroosh et al. (Citation2011) and Grenness et al. (Citation2014b) have summarised, the use of a person-centred approach to manage chronic conditions such as hearing impairment leads to successful outcomes as the approach fosters greater involvement, decision-making and empowerment in individuals and better self-management of their condition. A person-centred approach in hearing rehabilitation would suggest a process of setting individualised goals and relevant outcomes to define success.
As a follow up to the EMA study described in the previous section, Timmer et al. (Citation2018) reported a pilot study using the smartphone app to measure real-world listening experiences for adults before and after hearing aid fitting. The ten participants with mild hearing impairment (mean age = 70 years) and no previous amplification experience answered survey questions on an app detailing their listening experiences over a 4-week period (1 week without hearing aids, followed by 2 weeks with hearing aids, and then 1 week without hearing aids). Results from the 860 surveys collected showed that participants reported hearing aid benefit during the 2-week trial but there was significant individual variation in the nature of the benefits. Three participants showed a large degree of benefit from wearing hearing aids in terms of reduced listening effort but only medium or small degrees of benefit for improved speech understanding. The same three participants had reported needing to expend listening effort to communicate effectively without hearing aids and therefore reduced listening effort would have been an appropriate individual rehabilitation goal. It is important to note that a reduction in listening effort would be unlikely to be elicited as a goal using traditional self-report goal-setting measures such as the Client Oriented Scale of Improvement (COSI; Dillon, James, and Ginis Citation1997). One participant in the study showed no benefit and some deterioration across all hearing dimensions with hearing aids. For clinical practice, this insight from the app could highlight the need for further questioning and possibly finetuning of the hearing aids to validate if real-world benefit could be achieved for this participant.
As the review by Paglialonga et al. (Citation2018) highlighted, hearing aid fitting and fine-tuning can also be conducted using teleaudiology apps and this functionality is now supported by all major hearing aid manufacturers. In a recent study to evaluate the feasibility and perceived benefits of providing teleaudiology hearing aid follow-up appointments, Angley, Schnittker, and Tharpe (Citation2017) found over 80% of the 50 participants (mean age = 65 years) reported preferring teleaudiology follow-up appointments, rather than face-to-face, and over 90% would recommend teleaudiology hearing aids appointments to others.
Supporting the maintenance stage
As stated earlier, success with hearing aids requires the ability to manage them. Research indicates, however, that many adults, including experienced hearing aid users, have difficulty with aspects of aid management. These hearing aids management difficulties can lead to low use and reduced ratings of satisfaction (Mulrow, Tuley, and Aguilar Citation1992; Kumar, Hickey, and Shaw Citation2000; Bertoli et al. Citation2009). A study by Bennett et al. (Citation2018) identified an array of device management difficulties related to the use, care and handling of the hearing aids and suggested these problems have significant impact on overall hearing aid success in the long term. Their findings highlighted that hearing aids management information and instruction should receive greater emphasis from clinicians to better support individuals’ rehabilitation journey. The provision of such information by means of interactive, educational content delivered on mobile technology platforms such as smartphones has been shown to lead to better hearing aids self-efficacy and knowledge (Maidment et al. Citation2020).
To add to the emerging research evidence investigating if apps could support hearing aid management, we utilised a prototype app developed by Sonova AG (Staefa, Switzerland) designed to support hearing aid wearers in daily use and management. The primary research questions were: (1) Could adults over the age of 60 years with no previous hearing aid experience use the app to perform everyday hearing aid management tasks? and (2) What factors affected the ability of participants to use the app? The participant inclusion criteria were age 60 years or older, living in the community, comfortable speaking and reading English, and no experience using or managing hearing aids including assisting a significant other. Adults were eligible to participate regardless of whether or not they had a hearing impairment. In addition, participants had to own, and self-report to be confident using apps on a smartphone or tablet. Participants were recruited through The University of Queensland research registries, the university invigilators group, local retirement villages, and word-of-mouth. Ethical approval was provided by The University of Queensland Behavioural and Social Sciences Ethical Review Committee. All participants were reimbursed with an AUD25 (approximately USD20) gift voucher for their participation.
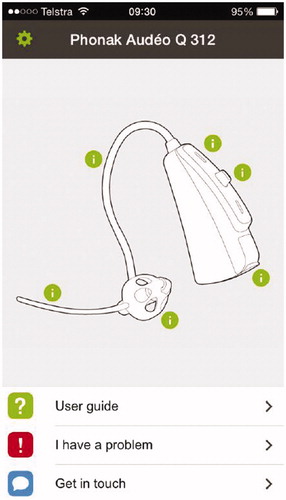
Two identical Phonak (Sonova AG, Staefa, Switzerland) mini behind-the-ear hearing aids, with a thin tube, dome earpiece, and a pushbutton configured to change volume, were used for the study. The hearing aids were set up with the default alerts (beeps) to indicate program or volume change, but were programmed to provide no amplification. The app was installed by the researchers on iPod Touch devices manufactured by Apple Inc (Cupertino, US) and was a beta version of a hearing aid management app intended for release to the public at a future date for both iOS and Android platforms. The iPod Touch devices had a 4-inch or 10.2 cm (diagonal) widescreen display and all display settings (such as brightness, etc) were left at default settings.
During the data collection appointment, all participants completed a demographic questionnaire to obtain characteristics such as age and sex and information related to length of smartphones ownership, confidence in ability to use apps, and frequency of app use to gain insight into the participants’ previous use of apps. Although hearing status was not an exclusion criteria, pure-tone air-conduction thresholds were obtained for both ears at 0.5, 1, 2, and 4 kHz to ensure participants were able to hear the researchers’ instructions. To assess a number of factors which may impact on an individual’s ability to effectively use the app to complete the hearing aid management tasks, a number of standardised measures were also administered using paper-and-pencil with the researcher present. These included the Measure of Audiologic Rehabilitation Self-Efficacy for Hearing Aids (MARS-HA; West and Smith Citation2007) to assess hearing aid self-efficacy, the Short Test of Functional Health Literacy in Adults (Baker et al. Citation1999) to assess health literacy, the Grooved Pegboard Test (Bornstein Citation1985) to assess finger dexterity and the Montreal Cognitive Assessment test (MoCA; Nasreddine et al. Citation2005) to detect cognitive impairment.
Each participant was then shown the hearing aid and its components were described by the researcher using the same terminology used in the apps (such as volume button, dome, etc). The participants were then given one minute to become familiar with the app. The app opens to a “home screen” () showing the hearing aid model used in this study. The “home screen” has three main sections: user guide, troubleshooting (“I have a problem”), and feedback (“Get in touch”). The user guide section included instructions on common hearing aid management tasks using text, diagrams and videos.
Participants were asked to complete a number of common hearing aid management tasks and were assessed by means of a test modified from the Practical Hearing Aid Skills Test (PHAST) devised by Desjardins and Doherty (Citation2009). The test was modified to reflect the particular hearing aids being used in the study and that the handling skills would be guided by means of an app. For example, the PHAST separates changing volume and changing program tasks into two tasks, whereas this task could be completed using the same (one) physical control on the hearing aids in this study. The resulting modified test required the participant to perform six hearing aid management tasks with guidance from an app, on their own or with prompts. The tasks were: (1) change the battery, (2) turn the hearing aid on and off, (3) insert the hearing aid in the ear on the dominant side (e.g. right ear if the person was right handed), (4) turn up the volume on both hearing aids, (5) remove the hearing aids and turn them off, and (6) clean the dome. Following task 3, the second device was placed by the researcher on the non-dominant side ear after the participant had inserted the hearing aid on their dominant side, to allow completion of tasks 4–6 using both hearing aids.
After providing some time for the participants to become familiar with the app, they were asked to perform the first task (change the battery). The app was opened by the researcher on the home screen (see ) as the starting point for each task. If the participant made errors or was unable to complete the task within 2 min, the researcher proceeded to provide a series of prompts in hierarchical order. These were: (a) opening the app to the correct section (if they were unable to find it), (b) playing the video (if they had found the correct section but not seen the video), and (c) providing a second chance (only for those who had found the correct section and watched the video). The participant was moved through the prompts until they had completed the task correctly or had reached the last prompt. Final task performance and the time taken to complete the task were recorded. For each task a score of 2 indicated correct performance with no prompts, a score of 1 indicated correct performance with 1 prompt, and a score of 0 indicated the need for more than 1 prompt and/or inability to perform the task correctly. The possible total score for completing all six common hearing aid management tasks ranged from 0 to a maximum score of 12.
The study included 30 participants (17 females, 13 males) with a mean age of 69.2 years, ranging from 62 to 91 years. The median length of smartphone ownership was 24 months and 60% of participants reported being somewhat or quite a bit confident in using apps with 37% reporting they felt extremely confident. The participants had a varied amount of app experience with the number of apps installed by participants ranging from 0 to 221. On average, over half (56%) of the participants reported using apps once a day or more, whilst 17% reported using them once a week or less. A median score of 87% on the MARS-HA indicated high self-efficacy for hearing aid handling skills. The Grooved Peg Board results (mean = 86.7 s) was similar to the normative data for adults between 65 and 74 years (Ashendorf, Vanderslice-Barr, and McCaffrey Citation2009), however, although all participants passed a cognitive screener, 20% scored less than 26 and therefore returned a rating of “abnormal” on the MoCA.
The results from the hearing aid management test showed that of the 30 participants, 22 scored 10 points or more out of a maximum of 12 points, indicating that a substantial number were able to correctly complete all or a majority of the tasks assessed. Almost all participants (90% or greater) were able to perform each of the following tasks correctly without the need for any prompts: turn hearing aids on and off, increase volume on both hearing aids, remove both hearing aids and turn them off, and clean the dome. Almost three-quarters of participants (73%) were able to change the battery, however, only 17% were able to insert the hearing aid in their ear on their dominant side, with the biggest issue being the inability to distinguish between the right and left device. Although red and blue indicator colour codes were placed on the hearing aids’ external receivers, participants reported that these were difficult to see, making the corresponding instructions on the app difficult to interpret.
In analysing which personal factors were related to the participants’ hearing aid task test scores, results of the Spearman’s rank-order correlation indicated that there was a moderate positive association between MoCA scores and task scores, (rs(28) = .457, p = .006), suggesting greater cognitive ability was related to the ability to successfully complete hearing aid management tasks. Participant variables such as age, sex, hearing, attitude to hearing aids, self-efficacy, health literacy and finger dexterity were not significantly associated with the individual’s ability to complete the six tasks.
After completing the test, participants were shown the printed user guide for the same hearing aids and asked whether they would prefer this or the hearing aid management app. The majority said they would like both but when pushed to make a decision, 19 participants (63%) preferred the app. A total of 35 responses were made by participants as to why they preferred the app with 17% of comments relating to the inclusion of high quality videos. Other reasons cited by participants were ease of use (20%), clear instructions (14%), less text than a printed user guide (14%), and portability (9%). A total of 24 comments were made by participants who preferred a printed user guide with over half of these relating to the participant’s confidence and familiarity with printed materials. Three quarters of the participants who expressed a preference for the printed user guide believed that it contained more information and detail on the hearing aids. Preference for either the app or the printed user guide was not related to participant characteristics such as age, however, as participant inclusion criteria for this study included self-reported confidence in using apps, individuals who do not have such confidence may show a higher preference for a printed user guide.
In relation to the first aim of this study, it was clear that the majority of older adults who were confident with smartphones and apps could use an app to support hearing aid management. The ability to use interactive elements such as step-by-step instructions, diagrams and videos helped in explaining and visualising the steps involved in completing hearing aid tasks. This finding was also a conclusion from a study by Ferguson et al. (Citation2016) which showed that particularly first-time hearing aids users can be significantly supported in hearing aid self-management with the use of multimedia elements. In clinical practice, the use of a hearing aid management app could be beneficial as a complement to clinician instruction, particularly during the early stages of use, when the wearer is still familiarising with the everyday tasks required for hearing aid success.
In relation to the second aim of the study to identify factors associated with the ability to use the app, it was found that poorer cognitive ability was associated with less successful use of the app. This relationship between cognitive ability and the ability to perform hearing aid management tasks has also been found in other studies (e.g. Convery et al. Citation2013; Convey et al. Citation2015) and highlights the fact that some older adults will need ongoing support to learn how to effectively manage their hearing aids.
Conclusion and future directions
This paper highlights evidence about the use of smartphone apps to support the hearing rehabilitation patient journey by: raising awareness of hearing difficulties in everyday life, understanding the complex individualised nature of those difficulties, developing shared plans and goals for rehabilitation, measuring the outcomes of device fitting and supporting device management.
The research cited in this review suggests that smartphone apps can be beneficial, particularly when under the direction of a researcher or clinician. However, there is little knowledge about the most effective behaviour change models to be implemented using mobile health apps or how these could support long-term behaviour change (Helbostad et al. Citation2017). There is some modest evidence that suggests that diet and physical activity can be improved with the use of app-based interventions (Schoeppe et al. Citation2016) however, further research is required to investigate if the behaviour change involved in hearing rehabilitation can be supported with the use of smartphone apps. As indicated earlier, an individual’s self-assessment of their hearing difficulties are a strong driver for change and smartphone apps may provide the insight required to drive motivation for help-seeking. Some of these questions may be answered by the research being conducted by Pronk and her colleagues (Pronk et al. Citation2020) which aims to develop and assess an individualised app to improve the self-management of hearing impairment in adults over the age of 50 years as an alternative or precursor to hearing aids rehabilitation.
Further research could also be directed at the use of smartphone apps to monitor changes in the hearing situations the individuals may encounter following an intervention. As the adoption of hearing aids may lead to a change in auditory lifestyle, new hearing rehabilitation goals may emerge in the maintenance phase of the patient journey. There is evidence to show that hearing goals are often not re-visited during the patient journey, potentially resulting in audiology services not meeting the patient’s changing needs (Hickson Citation2010). In future, smartphone apps may facilitate the assessment of a change in auditory lifestyle, and advise clinicians and patients of new hearing needs.
People with hearing impairment live with this chronic health condition every day, and they and their families should become the experts on how to manage the condition. Visits to hearing clinics occur only occasionally and, in the meantime, apps on a smartphone can provide the insight, support and assistance required to successfully navigate the patient journey.
Acknowledgements
The authors would like to thank Dr Andrea Caposecco for assistance with the hearing aid management app study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Alicea, C. C. M., and K. A. Doherty. 2017. “Motivation to Address Self-Reported Hearing Problems in Adults with Normal Hearing Thresholds.” Journal of Speech, Language, and Hearing Research: JSLHR 60 (12): 3642–3655. doi:10.1044/2017_JSLHR-H-17-0110.
- Angley, G. P., J. A. Schnittker, and A. M. Tharpe. 2017. “Remote Hearing Aid Support: The Next Frontier.” Journal of the American Academy of Audiology 28 (10): 893–900. doi:10.3766/jaaa.16093.
- Ashendorf, L., J. L. Vanderslice-Barr, and R. J. McCaffrey. 2009. “Motor Tests and Cognition in Healthy Older Adults.” Applied Neuropsychology 16 (3): 171–176. doi:10.1080/09084280903098562.
- Baker, D. W., M. V. Williams, R. M. Parker, J. A. Gazmararian, and J. Nurss. 1999. “Development of a Brief Test to Measure Functional Health Literacy.” Patient Education and Counseling 38 (1): 33–42. doi:10.1016/s0738-3991(98)00116-5.
- Barczik, J., and Y. C. Serpanos. 2018. “Accuracy of Smartphone Self-Hearing Test Applications across Frequencies and Earphone Styles in Adults.” American Journal of Audiology 27 (4): 570–580. doi:10.1044/2018_AJA-17-0070.
- Barlow, J., C. Wright, J. Sheasby, A. Turner, and J. Hainsworth. 2002. “Self-Management Approaches for People with Chronic Conditions: A Review.” Patient Education and Counseling 48 (2): 177–187. doi:10.1016/s0738-3991(02)00032-0.
- Bennett, J. R., J. A. Laplante-Lévesque, H. C. Meyer, and H. R. Eikelboom. 2018. “Exploring Hearing Aid Problems: Perspectives of Hearing Aid Owners and Clinicians.” Ear and Hearing 39 (1): 172–187. doi:10.1097/AUD.0000000000000477.
- Bertoli, Sibylle, Katharina Staehelin, Elisabeth Zemp, Christian Schindler, Daniel Bodmer, and Rudolf Probst. 2009. “Survey on Hearing Aid Use and Satisfaction in Switzerland and Their Determinants.” International Journal of Audiology 48 (4): 183–195. doi:10.1080/14992020802572627.
- Bornstein, R. A. 1985. “Normative Data on Selected Neuropsychological Measures from a Nonclinical Sample.” Journal of Clinical Psychology 41 (5): 651–659. doi:10.1002/1097-4679(198509)41:5<651::AID-JCLP2270410511>3.0.CO;2-C.
- Bright, T., and D. Pallawela. 2016. “Validated Smartphone-Based Apps for Ear and Hearing Assessments: A Review.” JMIR Rehabilitation and Assistive Technologies 3 (2): e13–e13. doi:10.2196/rehab.6074.
- Chisolm, T. H., H. B. Abrams, and R. McArdle. 2004. “Short- and Long-Term Outcomes of Adult Audiological Rehabilitation.” Ear and Hearing 25: 464–477. doi:10.1097/01.aud.0000145114.24651.4e
- Convery, Elizabeth, Gitte Keidser, Andrea Caposecco, De Wet Swanepoel, Lena L. N. Wong, and Eed Shen. 2013. “Hearing-Aid Assembly Management among Adults from Culturally and Linguistically Diverse Backgrounds: Toward the Feasibility of Self-Fitting Hearing Aids.” International Journal of Audiology 52 (6): 385–393. doi:10.3109/14992027.2013.773407.
- Convery, E., G. Keidser, L. Hickson, and C. Meyer. 2019. “The Relationship Between Hearing Loss Self-Management and Hearing Aid Benefit and Satisfaction.” American Journal of Audiology 28 (2): 274–284. doi:10.1044/2018_AJA-18-0130.
- Convey, E., G. Keidser, M. Seeto, I. Yeend, and K. Freeston. 2015. “Factors Affecting Reliability and Validity of Self-Directed Automatic in Situ Audiometry: Implications for Self-Fitting Hearing Aids.” The Journal of the American Academy of Audiology 26: 5–18.
- Desjardins, J. L., and K. A. Doherty. 2009. “Do Experienced Hearing Aid Users Know How to Use Their Hearing AIDS Correctly??” American Journal of Audiology 18 (1): 69–76. doi:10.1044/1059-0889(2009/08-0022).
- Dillon, H., A. James, and J. Ginis. 1997. “The Client Oriented Scale of Improvement (COSI) and Its Relationship to Several Other Measures of Benefit and Satisfaction Provided by Hearing Aids.” Journal of the American Academy of Audiology 8 (1): 27–43.
- Ekberg, K., C. Grenness, and L. Hickson. 2016. “Application of the Transtheoretical Model of Behaviour Change for Identifying Older Clients’ Readiness for Hearing Rehabilitation During History-Taking in Audiology Appointments.” International Journal of Audiology 55 (sup3): S42–S51. doi:10.3109/14992027.2015.1136080.
- Ferguson, M., M. Brandreth, W. Brassington, P. Leighton, and H. Wharrad. 2016. “A Randomized Controlled Trial to Evaluate the Benefits of a Multimedia Educational Program for First-Time Hearing Aid Users.” Ear and Hearing 37 (2): 123–136. doi:10.1097/AUD.0000000000000237.
- Ferguson, M. A., P. T. Kitterick, L. Y. Chong, M. Edmondson-Jones, F. Barker, and D. J. Hoare. 2017. “Hearing Aids for Mild to Moderate Hearing Loss in Adults.” Cochrane Database of Systematic Reviews, 9: CD012023.
- Fisk, A. D., W. A. Rogers, N. Charness, S. J. Czaja, and J. Sharit. 2009. Designing for Older Adults: Principles and Creative Human Factors Approaches. Boca Raton: CRC Press.
- Gomez, R., and M. Ferguson. 2020. “Improving Self-Efficacy for Hearing Aid Self-Management: The Early Delivery of a Multimedia-Based Education Programme in First-Time Hearing Aid Users.” International Journal of Audiology 59 (4): 272–281. doi:10.1080/14992027.2019.1677953.
- Gregory, M. 2012. “A Possible Patient Journey: A Tool to Facilitate Patient-Centered Care.” Seminars in Hearing 33: 9–15.
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014a. “Patient-Centred Audiological Rehabilitation: Perspectives of Older Adults Who Own Hearing Aids.” International Journal of Audiology 53 (sup1): S68–S75. doi:10.3109/14992027.2013.866280.
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014b. “Patient-Centred Care: A Review for Rehabilitative Audiologists.” International Journal of Audiology 53 (sup1): S60–S67. doi:10.3109/14992027.2013.847286.
- Helbostad, Jorunn, Beatrix Vereijken, Clemens Becker, Chris Todd, Kristin Taraldsen, Mirjam Pijnappels, Kamiar Aminian, et al. 2017. “Mobile Health Applications to Promote Active and Healthy Ageing.” Sensors (Basel) 17 (3): 622. doi:10.3390/s17030622.
- Hickson, L. 2010. “Longitudinal Change in Enablement Needs of Older People with Hearing Impairment.” In Living with Hearing Difficulties: The Process of Enablement, edited by D. Stephens and S. E. Kramer. Chicester, UK: Wiley & Sons.
- Humes, L. E. 2006. “Hearing Aid Outcome Measures in Older Adults.” In Hearing Care for Adults, edited by C. A. Palmer and R. C. Seewald, 265–276. Chicago, IL: Phonak AG.
- Iqbal, M. 2020. “App Download and Usage Statistics Business of Apps.” Staines-Upon-Thames, UK: Simform.
- Kumar, M., S. Hickey, and S. Shaw. 2000. “Manual Dexterity and Successful Hearing Aid Use.” The Journal of Laryngology and Otology 114 (8): 593–597. doi:10.1258/0022215001906480.
- Laplante-Lévesque, A., L. Hickson, and L. Worrall. 2013. “Stages of Change in Adults with Acquired Hearing Impairment Seeking Help for the First Time: Application of the Transtheoretical Model in Audiologic Rehabilitation.” Ear Hear 34:447–457. doi:10.1097/AUD.0b013e3182772c49
- Lorig, K. R., and H. R. Holman. 2003. “Self-Management Education: History, Definition, Outcomes, and Mechanisms.” Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine 26 (1): 1–7. doi:10.1207/S15324796ABM2601_01.
- Maidment, David W., Rachel Heyes, Rachel Gomez, Neil S. Coulson, Heather Wharrad, and Melanie A. Ferguson. 2020. “Evaluating a Theoretically Informed and Cocreated Mobile Health Educational Intervention for First-Time Hearing Aid Users: Qualitative Interview Study.” JMIR mHealth and uHealth 8 (8): e17193. doi:10.2196/17193.
- Manchaiah, V. K. C., D. Stephens, G. Andersson, J. Rönnberg, and T. Lunner. 2013. “Use of the ‘Patient Journey’ Model in the Internet-Based Pre-Fitting Counseling of a Person With Hearing Disability: Study Protocol for a Randomized Controlled Trial.” Trials 14: 25. doi:10.1186/1745-6215-14-25.
- Margolis, R. H., G. Bratt, M. P. Feeney, M. C. Killion, and G. L. Saly. 2018. “Home Hearing Test: Within-Subjects Threshold Variability.” Ear Hear 39 (5): 906–909. doi:10.1097/AUD.0000000000000551.
- Meyer, C., and L. Hickson. 2012. “What Factors Influence Help-Seeking for Hearing Impairment and Hearing Aid Adoption in Older Adults?” International Journal of Audiology 51 (2): 66–74. doi:10.3109/14992027.2011.611178.
- Mulrow, C. D., M. R. Tuley, and C. Aguilar. 1992. “Correlates of Successful Hearing Aid Use in Older Adults.” Ear and Hearing 13 (2): 108–113. doi:10.1097/00003446-199204000-00007.
- Nasreddine, Ziad S., Natalie A. Phillips, Valérie Bédirian, Simon Charbonneau, Victor Whitehead, Isabelle Collin, Jeffrey L. Cummings, et al. 2005. “The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment.” Journal of the American Geriatrics Society 53 (4): 695–699. doi:10.1111/j.1532-5415.2005.53221.x.
- Oh, S. H., and J. Lee. 2016. “General Framework of Hearing Aid Fitting Management.” Journal of Audiology & Otology 20 (1): 1–7. doi:10.7874/jao.2016.20.1.1.
- Ohlenforst, Barbara, Adriana A. Zekveld, Thomas Lunner, Dorothea Wendt, Graham Naylor, Yang Wang, Niek J. Versfeld, et al. 2017. “Impact of Stimulus-Related Factors and Hearing Impairment on Listening Effort as Indicated by Pupil Dilation.” Hearing Research 351: 68–79. doi:10.1016/j.heares.2017.05.012.
- Paglialonga, A., A. Cleveland Nielsen, E. Ingo, C. Barr, and A. Laplante-Lévesque. 2018. “eHealth and the Hearing Aid Adult Patient Journey: A State-of-the-Art Review.” Biomedical Engineering Online 17 (1): 101. doi:10.1186/s12938-018-0531-3.
- Paglialonga, A., F. Pinciroli, and G. Tognola. 2017. “The ALFA4Hearing Model (At-a-Glance Labeling for Features of Apps for Hearing Health Care) to Characterize Mobile Apps for Hearing Health Care.” American Journal of Audiology 26 (3S): 408–425. doi:10.1044/2017_AJA-16-0132.
- Paglialonga, A., G. Tognola, and F. Pinciroli. 2015. “Apps for Hearing Science and Care.” American Journal of Audiology 24 (3): 293–298. doi:10.1044/2015_AJA-14-0093.
- Pew Research Center 2018. Mobile Fact Sheet: Mobile Phone Ownership. http://www.pewinternet.org/fact-sheet/mobile/.
- Picou, E. M., T. A. Ricketts, and B. W. Hornsby. 2013. “How Hearing Aids, Background Noise, and Visual Cues Influence Objective Listening Effort.” Ear and Hearing 34 (5): e52–e64. doi:10.1097/AUD.0b013e31827f0431.
- Plaza, I., L. Martín, S. Martin, and C. Medrano. 2011. “Mobile Applications in an Aging Society: Status and Trends.” The Journal of Systems & Software 84: 1977–1988. doi:10.1016/j.jss.2011.05.035
- Poost-Foroosh, L., M. B. Jennings, L. Shaw, C. N. Meston, and M. F. Cheesman. 2011. “Factors in Client-Clinician Interaction That Influence Hearing Aid Adoption.” Trends in Amplification 15 (3): 127–139. doi:10.1177/1084713811430217.
- Prochaska, J. O., S. Johnson, and P. Lee. 2009. “The Transtheoretical Model of Behavior Change.” In The Handbook of Health Behavior Change, 3rd ed, edited by S. A. Shumaker, J. K. Ockene, and K. A. Riekert, 59–83. New York, NY: Springer Publishing Company.
- Pronk, Marieke, Jana Besser, Cas Smits, Vanessa Feenstra-Kikken, Hans van Beek, Conny Polleunis, Sophia E. Kramer, et al. 2020. “Rationale, Theoretical Underpinnings, and Design of HEAR-Aware: Providing Adults with Hearing Loss with Tailored Support to Self-Manage Their Hearing Problems via a Smartphone App, as an Alternative to Hearing Aids.” American Journal of Audiology 29 (3S): 648–660. doi:10.1044/2020_AJA-19-00079.
- Saunders, G. H., T. H. Chisolm, and H. B. Abrams. 2005. “Measuring Hearing Aid Outcomes - Not as Easy as It Seems.” The Journal of Rehabilitation Research and Development 42 (4s): 157–168. doi:10.1682/JRRD.2005.01.0001.
- Schoeppe, Stephanie, Stephanie Alley, Wendy Van Lippevelde, Nicola A. Bray, Susan L. Williams, Mitch J. Duncan, Corneel Vandelanotte, et al. 2016. “Efficacy of Interventions That Use Apps to Improve Diet, Physical Activity and Sedentary Behaviour: A Systematic Review.” The International Journal of Behavioral Nutrition and Physical Activity 13 (1): 127–127. doi:10.1186/s12966-016-0454-y.
- Simpson, A. N., K. N. Simpson, and J. R. Dubno. 2015. “Health-Related Quality of Life in Older Adults: Effects of Hearing Loss and Common Chronic Conditions.” Healthy Aging Research 4: 4.
- Statista 2020. Smartphone Ownership in Australia as of July 2019, by Age. https://www.statista.com/statistics/730101/australia-smartphone-ownership-by-age/
- Stephens, D., and S. E. Kramer, eds. 2009. Living with Hearing Difficulties: The Process of Enablement. New York, United States: John Wiley & Sons.
- Stone, A. A., S. Shiffman, J. E. Schwartz, J. E. Broderick, and M. R. Hufford. 2002. “Patient Noncompliance with Paper Diaries.” BMJ (Clinical Research ed.) 324 (7347): 1193–1195. doi:10.1136/bmj.324.7347.1193.
- Swanepoel, D. W., K. C. De Sousa, C. Smits, and D. R. Moore. 2019. “Mobile Applications to Detect Hearing Impairment: Opportunities and Challenges.” Bulletin of the World Health Organization 97 (10): 717–718. doi:10.2471/BLT.18.227728.
- Taylor, B. 2020. “Audiology’s Third Pillar: Comprehensive Follow-Up Care and Counseling for Those Who Choose to Self-Direct Their Care.” In Advances in Rehabilitation of Hearing Loss, edited by D. Zanetti and F. D. Berardino. London: IntechOpen.
- Timmer, B. H. B., L. Hickson, and S. Launer. 2015. “Adults with Mild Hearing Impairment: Are we Meeting the Challenge?” International Journal of Audiology 54 (11): 786–795. doi:10.3109/14992027.2015.1046504.
- Timmer, B. H. B., L. Hickson, and S. Launer. 2017. “Ecological Momentary Assessment: Feasibility, Construct Validity, and Future Applications.” American Journal of Audiology 26 (3S): 436–442. doi:10.1044/2017_AJA-16-0126.
- Timmer, B., L. Hickson, and S. Launer. 2018. “Do Hearing Aids Address Real-World Hearing Difficulties for Adults with Mild Hearing Impairment? Results from a Pilot Study Using Ecological Momentary Assessment.” Trends in Hearing : 22: 2331216518783608. doi:10.1177/2331216518783608.
- Timmer, B. H. B., L. Hickson, and S. Launer. 2018. “The Use of Ecological Momentary Assessment in Hearing Research and Future Clinical Applications.” Hearing Research 369: 24–28. doi:10.1016/j.heares.2018.06.012.
- West, R. L., and S. L. Smith. 2007. “Development of a Hearing Aid Self-Efficacy Questionnaire.” International Journal of Audiology 46 (12): 759–771. doi:10.1080/14992020701545898.
- Wildenbos, G. A., L. Peute, and M. Jaspers. 2018. “Aging Barriers Influencing Mobile Health Usability for Older Adults: A Literature Based Framework (MOLD-US).” International Journal of Medical Informatics 114: 66–75. doi:10.1016/j.ijmedinf.2018.03.012.