Abstract
Objective: Although insomnia often compounds tinnitus, sleeping problems in people experiencing tinnitus are rarely treated. This study investigates the experiences of participants receiving Cognitive Behavioural Therapy for insomnia (CBTi) as part of a randomised controlled trial for managing tinnitus-related insomnia. The aim of this study is to gain detailed insight into participants’ perceptions and experiences of this treatment.
Design: Semi-structured interviews were conducted via phone or in-person by one of the two clinical psychologists who facilitated the CBTi sessions. Reflexive thematic analysis with semantic inductive approach was used for analysis to keep the research question theoretically flexible.
Study samples: Eight participants (three females, age range 32–69 years) were interviewed six months after CBTi completion.
Results: Three superordinate themes were identified: “Common humanity and transcending individual distress,” “Changing the things I can” and “Accepting the things I cannot change.” The group environment helped participants to normalise their experiences. Reliable tinnitus/sleep information and robust behavioural change techniques helped participants to respond and relate to their condition differently.
Conclusion: Generally, participants reported long-term benefits from CBTi to treat tinnitus-related insomnia, particularly increased confidence, and getting on with life. CBTi is multi-component, so clinicians need to respond to individual preferences and lifestyles.
Introduction
Tinnitus is a common condition, reported in all age groups and is estimated to affect about 15% to 30% of the adult population with increased incidence in older adults (Kim et al. Citation2015). Tinnitus involves the perception of a noise in the ear or head in the absence of an external source of sound (Baguley, McFerran, and Hall Citation2013). Detailed understanding of the pathophysiology of tinnitus is lacking. It seems to be related to physiological changes in the auditory system (Shore, Roberts and Langguth Citation2016) and is also closely linked to psychological well-being (Kim et al. Citation2015). At present, there is no cure for tinnitus in that there is nothing that makes the noise inaudible. Some chronic tinnitus sufferers experience the noise as extremely distressing and disabling; it can cause occupational impairment, disrupt interpersonal relationships and change emotional responses, which can lead to anxiety and depression (Baguley, McFerran, and Hall Citation2013).
Tinnitus can be more noticeable in quiet circumstances such as at bedtime, which may contribute to the findings that insomnia is one of the most common complaints of tinnitus sufferers and can further affect their well-being (Schecklmann et al. Citation2015). Insomnia is the repeated difficulty initiating or maintaining sleep or waking early with inability to return to sleep, causing worry, suffering and impairment (Riemann et al. Citation2017).
Relationships between tinnitus and insomnia
Similar precipitants and maintaining factors of tinnitus and insomnia have been identified: shared underlying physiological mechanistic pathways such as hyperarousal of the sympathetic nervous system and activation of the same brain regions regulating emotions in the conditions of distressing tinnitus and insomnia (Wallhäusser-Franke, Schredl and Delb Citation2013).
Correlation studies indicate links between self-rated tinnitus severity and insomnia (e.g. Schecklmann et al. Citation2015). This suggests that physical sensations such as loudness and consistency of the noise would predict symptoms of insomnia. The available evidence does not support this straight-forward prediction. For example, Aazh and Moore (Citation2019) observed that the relationship is mediated by factors such as depression, tinnitus annoyance and tinnitus handicap (impact of tinnitus on daily living). Crönlein et al. (Citation2016) showed that psychological and cognitive variables contribute to impaired sleeping in people with chronic tinnitus. They found that next to somatic complaints, tinnitus patient’s insomnia results from insomnia-specific concerns such as increased worrying about deficient sleep, anxiety at bedtime and catastrophizing thoughts. Such observations suggest a more complex picture of the relationship between insomnia and tinnitus, involving cognitive, emotional and somatic factors.
It is likely that relationships between tinnitus and insomnia are bidirectional (Asnis et al. Citation2018). Poor sleep may worsen the experience of tinnitus by creating an opportunity for greater awareness of tinnitus, reduced tolerance for and altered perception of tinnitus and greater distress. More intrusive tinnitus may, in turn, make it more difficult to obtain sleep by provoking greater physical and cognitive arousal. People experiencing tinnitus have reported that improving night-time sleep would be the most important factor to decrease tinnitus severity (Eysel-Gosepath and Selivanova Citation2005).
Current treatment approaches
It is apparent from current UK NICE guidelines that apart from providing amplification in the context of an accompanying hearing loss, CBT is the treatment to be considered for people with tinnitus-related distress (NICE Citation2020). CBT incorporates cognitive and behavioural interventions and is based on the theory that dysfunctional cognitive factors (thoughts and beliefs) and behavioural responses maintain psychological distress, including tinnitus-related distress (McKenna et al. Citation2014). CBT uses strategies to reduce cognitive-behavioural factors that prevent habituation to tinnitus such as thought challenging and relaxation techniques (McKenna et al. Citation2014). In a systematic review and meta-analysis of 28 RCT, Hoare et al. (Citation2011), reported low to moderate effect sizes for most CBT intervention studies.
The benefits might be limited due to the CBT interventions not being specific to insomnia. It has been argued that although sleeping problems are a significant comorbidity for tinnitus sufferers, insomnia is still rarely treated in this population (Asnis et al. Citation2018). Many CBT interventions for tinnitus include a component of insomnia, but given the amount of other components that are covered in these interventions, they are usually informational in nature rather than practical-oriented (see Greenwell et al. Citation2016). Also, some tinnitus-related insomnia sufferers do not struggle during the day, they only suffer with insomnia, making them a poor fit for standard CBT protocols. Insufficient treatment of sleeping problems can cause a vicious cycle of untreated insomnia and potentiated tinnitus noise (Eysel-Gosepath and Selivanova Citation2005). A helpful comparison for how this might work comes from experimental work with chronic pain, as there are many similarities between pain and tinnitus (Moller Citation2007). Tang, Goodchild and Salkovskis (Citation2012) looked at pain-related insomnia and exemplified the demand of a two-dimensional intervention. They proposed that chronic pain-related insomnia should be treated as a stand-alone problem, because pain management alone did not resolve sleeping problems. This is because people with pain-related insomnia share underlying characteristics with people who suffer from insomnia independent from pain, maintaining dysfunctional behavioural habits around sleep and sleep-related anxiety (Tang et al. Citation2012).
CBT-for-insomnia adapted to tinnitus
Based on the above, there is a need to offer treatment beyond standard CBT for tinnitus to achieve sleep behaviour changes for individuals with comorbid insomnia and as this group might be better served by adapting interventions to address insomnia and tinnitus simultaneously. CBTi focuses on managing insomnia specific concerns and encompasses a range of practical-focussed tools that improve sleep including stimulus control, sleep hygiene, time-in-bed-restriction, where participants restrict their time in bed to the actual time being asleep after tracking their sleep, and relaxation training (Riemann et al. Citation2017). It is a popular treatment choice for sleeping problems with medium to large effect sizes (Okajima, Komada and Inoue Citation2011).
The benefits of using CBTi for tinnitus-related insomnia are demonstrated in the literature. A recent RCT of 102 participants with tinnitus-related insomnia compared CBTi to audiology based care and a sleep support group (Marks et al. Citation2022). CBTi was significantly more effective than both other control groups, and 80% of participants in CBTi reported clinically meaningful improvements in sleep, with additional improvements in tinnitus distress, functioning and mental health. This indicates that CBTi is more effective than treatment as usual and control groups, and more effective for treating sleep than general CBT for tinnitus (Marks et al. Citation2022).
Aims
Only one RCT (Marks et al. Citation2022) has investigated CBTi for tinnitus-related insomnia, indicating effectiveness. Alongside this is the need for interventions to improve theories and to contribute to understanding how the interventions contribute to change (Skivington et al. Citation2021). This is particularly important for complex multicomponent interventions, such as CBTi when applied to chronic conditions such as tinnitus. This qualitative study aims to look at potential mechanisms underlying the change in outcomes and to contribute to our understanding about how CBTi can be of benefit to people with both tinnitus and insomnia.
This study aimed to take qualitative accounts of tinnitus sufferers who received six CBTi sessions as part of an RCT (Marks et al. Citation2022) and explore the question: How do participants experience CBTi for treating their tinnitus-related insomnia? Qualitative approaches have already been used to explore peoples’ experiences, reactions, interactions and mechanisms of action, for example, with internet-based tinnitus self-management programs (Beukes et al. Citation2018; Greenwell et al. Citation2019; Greenwell et al. Citation2021). Reflexive Thematic Analysis (TA) was used to gain detailed insight into participants’ perceptions about the treatment, how they understand the changes in their experience of tinnitus and sleep that occur during treatment, and whether/how CBTi was effective in the long-term. Qualitative methods allow deeper exploration of experiences regarding the treatment and can contribute to the development of more effective therapies for tinnitus both in routine clinical practice and future research.
Methods
Design
The study took place as part of a larger RCT (Marks et al. Citation2022), and participants who had completed CBTi within the RCT were invited to take part in an interview study six months later, to allow for deeper investigation of their perceived experiences and changes relating to treatment. As CBTi for tinnitus-related insomnia is poorly researched, a reflexive approach to TA was used for analysis to keep the research question theoretically flexible (Braun and Clarke Citation2020). The RCT was registered with ClinicalTrials.gov, NCT03386123. Ethical approval was granted for the trial by the London-Camden and Kings Cross NHS Research Ethics Committee and for the reflective study by the University of Bath Research Ethics Committee, 21-052.
Participants
Participants were screened using self-report measures for sleep, tinnitus and organic sleep disorders. Those meeting minimum thresholds then took part in an assessment with a clinical psychologist to ascertain inclusion and exclusion criteria (see Supplementary Table 1). An upper age limit was set at 70 years to avoid developmental insomnia in older adults. Full details of the assessment process are published in the full RCT (Marks et al. Citation2022).
Table 1. Participants’ characteristics (all names are pseudonyms).
Recruitment for the qualitative study took place at the follow up session after completion of CBTi. Only those eligible participants who completed CBTi and attended the follow up were invited to volunteer for the interviews. The first eight respondents were included. Gender, age, tinnitus, and insomnia duration varied; quantitative measures were taken as part of the RCT and indicated how tinnitus distress and insomnia changed following CBTi (). Names were replaced with pseudonyms to ensure confidentiality.
Braun and Clarke’s (Citation2021) reflexive TA guidance states that the sample size cannot be determined wholly in advance of analysis, but must be small enough to manage the data and large enough to provide a holistic and detailed understanding of the experience from within this participant group. As these participants were relatively homogenous in terms of experience (all report chronic tinnitus and insomnia), recruitment from one clinic setting and receipt of a standardised treatment with the same two clinicians, a total of eight participants were likely to provide sufficient data to explore their experiences. Furthermore, at the point of analysing the last two interviews, no new themes were identified, suggesting that code saturation may have been reached, but that meaning saturation may not have been achieved (discussed further in our limitations) (Braun and Clarke Citation2021).
Procedures
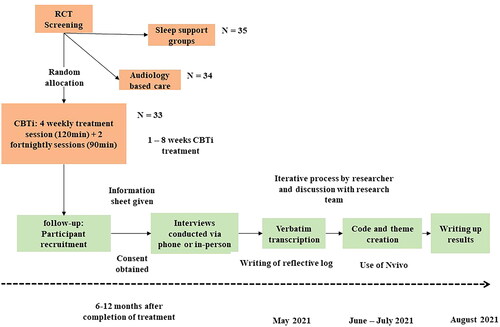
Participants who met inclusion criteria were randomly allocated to CBTi as part of the RCT. CBTi was delivered in a group setting and consisted of six sessions over eight weeks. The treatment methods were based on the UK standard treatment of insomnia, adapted to tinnitus. Participants were eligible only if they had completed the RCT and their final, six-month follow up. They were given information about this interview study, and if interested, they provided full, informed consent. All interviews were conducted by one of the trial clinicians and lasted 40–50 min. Participants were advised that the interviews were a chance to explore and reflect on therapy experiences, both positives and negatives. Interviews were conducted based on the interview schedule (see Supplementary Material) and asked participants to reflect on their experiences of CBTi including being in a group, balance between insomnia and tinnitus, barriers of treatment, changes and future implications. A chronological order of the procedural steps is illustrated in . Full explanation and detail of the treatment involved in CBTi is described in the published RCT by Marks et al. (Citation2022).
Analysis
The team adopted a critical realist epistemological perspective, trying to depict theory out of experience based on the assumption that meaning, language and experience are directly linked (Potter and Wetherell Citation1987). A semantic and inductive approach was chosen for the analysis to stay close to participants’ accounts and limit top-down approaches (Braun and Clarke Citation2020). It should be acknowledged, however, that qualitative research is a recursive process of critical reflection, and all stages of analysis were inevitably somewhat influenced by the researchers’ epistemological stance as they were active in creating the themes (Mills, Durepos and Wiebe Citation2010).
To ensure transparency, reflexive TA was used based on the guidance of Braun and Clarke (Citation2020). The first author (LC) achieved deep immersion of the data through a process of verbatim transcription, checking of accuracy, re-reading and noting down initial ideas of recurring codes/themes. LC demonstrated her reflexive engagement with theory, data and interpretation by writing a reflective log during initial data familiarisation. The log presents the researcher’s subjectivity as a “resource” which affected analysis and interpretation (Braun and Clarke Citation2020). Line-by-line codes that represent important features to answer the research question were applied by utilising the software programme NVivo. EM reviewed and checked the codes of the first interview before coding the other interviews. Codes were collated into potential themes/subthemes and a thematic map was developed. The themes were reviewed and refined which involved discussion with the research team. Each theme was described in detail and suitable extracts were chosen so that each participant’s personal story was constructed around key themes. See Supplementary Material for the thematic map (Supplementary Figure 2) and examples of how the coding was conducted on an excerpt of the material (Supplementary Table 2).
Table 2. Clinical recommendations based on results.
The research team consisted of two MSc students in Applied Clinical Psychology, and three clinical psychologists, two of whom delivered CBTi (EM & LMK). The first author who transcribed the interviews and led analysis had no personal experience with tinnitus, nor has she worked with tinnitus sufferers. Thus, analysis was less likely to be influenced by prior experience/expectations.
Results
Accounts revealed three overarching themes that were present in all interviews: “Common humanity and transcending individual distress,” “Changing the things I can” and “Accepting the things I cannot change.” Associated subthemes are summarised and described below.
Theme 1: common humanity and transcending individual distress
The group environment of this study’s treatment allowed participants to connect, collaborate and exchange with people who suffer from similar problems and put their tinnitus-related insomnia into a different, more shared perspective.
Mutual understanding, support and motivation
Most participants described that before treatment they often felt lonely and isolated, because friends and relatives did not understand the impacts of tinnitus-related insomnia. Participation in the group reduced loneliness because participants realised that other group members shared their suffering.
I used to feel alone, because I didn’t think that anybody understood these noises that you are hearing and how they affect you… then going to the course… I realised that other people have similar issues, and you are not alone. (Farah, 57 years, female)
Participants were particularly frustrated by the misconception of professionals who often underestimated the psychological impact of “severe” tinnitus and insomnia because of the high prevalence of more “mild” tinnitus in the population. Participants seemed relieved to meet other group members who had insight into their distress: “Other people have the same. Other people get it” (Bella, 32 years, female). The possibility to exchange with like-minded peers led participants to recognise the normality of their experiences. It helped them to realise that there are different degrees of tinnitus impact and to identify their condition as “medical and serious” (Bella), something that made them feel validated and important; being part of a scientific trial added to this.
I think just having the voice … having audience to help you share your experiences, it was quite powerful … it just made you part of something important really. (Ravi, 39 years, male)
Moreover, the group acted as a support system where members helped each other and explored how peers managed their tinnitus and insomnia, and “what worked for them and what didn’t" (Hannah, 57 years, female). Listening to other group members’ success stories enhanced their optimism and belief that the treatment works.
Just listening to the people that were there, they were really lovely people… I enjoyed listening that they were improving. That helped. (Oscar)
This shows that seeing other group members improve created happiness for the other, motivation to stay dedicated to the tasks and increased hope for recovery. Prevailing kindness in the group was described as another type of support next to understanding and motivation.
Because I was quite shy … people, you don’t know, it’s quite difficult to chat with, but the people in the group were really nice and kind of everybody just got on. That was nice. (Farah)
Putting tinnitus and insomnia into perspective
During the regular group sessions, some participants compared and contrasted their condition against others, causing mixed feelings. Firstly, realising that there are people who sleep less or have more intrusive tinnitus caused positive feelings: “I was grateful that I didn’t have it as bad as other people … it was comforting to know that” (Ravi). Downward comparisons seemed to affect people’s judgements about their symptom severity and made them feel fortunate for being “not as bad” (Paul, 53 years, male) when they realised there was worse suffering in the group. For some this even generated some feelings of guilt and being an “imposter” who did “not have the right” (Bella) to be part of CBTi: “I get a break from the tinnitus, whereas none of the others did … I did think I shouldn’t be here really” (Paul). In contrast, improvements reported by others could put pressure on some participants to similarly improve, creating feelings of “competitiveness” (Matthew, 46 years, male). For some this undermined motivation to continue treatment and lowered hopes for recovery.
By the third week their sleep was better, this was better, everything was better, and I couldn’t understand, because I was following everything and yet I had not improved by that stage. (Oscar)
Theme 2: changing the things I can
The rigorous behavioural CBTi components seemed to serve as structures and motivational guidance, while cognitive techniques helped to shift attitudes towards tinnitus and insomnia. Education about tinnitus and insomnia helped participants to differentiate between tinnitus as a “constant” and insomnia as a “variable … the thing they could do something with” (Hannah). This realisation motivated participants to change what they could, and accept what they could not.
Using structure and tools to support change
CBTi is a multi-component treatment, offering various techniques; a “toolbox” from which the “tools” that work best could be chosen, and different participants benefitted from different tools. Some found that a sleep diary helped them to “stick to the routine” (Declan, 52 years, male), reflect on sleep patterns, on actual hours asleep, and on daytime activities that might impact sleep. Relaxation and imagery techniques were perceived as particularly effective when struggling to sleep. Matthew said that he used relaxation techniques such as breathing not to dwell on the noise in the night; this helped him “more than anything.” Other participants used relaxation to “go back to sleep” (Declan) or “put them into the moment” (Matthew).
Some reported certain techniques being detrimental, such as the addition of sound enrichment on top of tinnitus could be perceived as “irritating” (Ravi). Bella found the breathing exercises induced anxiety if she could not regulate her breath. Furthermore, some participants experienced the thought challenging as “unhealthy” and “too deep” (Oscar) and preferred not to hold onto a negative thought but to rather “just let it go” (Matthew). Together this indicates how the multicomponent nature of CBTi may allow for individual variability and improvement with participants able to use the tools that resonated most with their needs and preferences.
All participants seemed to benefit from the realisation that the "structure around sleep" is important (Declan), which motivated engagement in lifestyle changes including increased exercise, reduced screen time before bed, reduced caffeine, and alcohol intake, and maintenance of good sleep hygiene. Time-in-bed-restriction was regarded as particularly effective in improving the ability to sleep. Bella commented that it “cured her sleep.” The start of the time-in-bed-restriction was challenging, particularly “keeping the wake-up time stable even on weekends” (Ravi) or “on a dark October morning” (Hannah). Nevertheless, all participants continued with the programme and early sleep improvements acted as an incentive to continue with the rigid routine.
From the initial beginning part of the study, I saw the improvements of getting my sleep better and better and I just continued with that trust and faith knowing that it was leading to a positive outcome. (Ravi)
The structure of CBTi in terms of fixed bedtime and wake-up times, sleep hygiene rituals and restriction helped participants to engage in changes and consequently sleep improved. Interestingly, changing sleep behaviour also seemed to be crucial for improvements in overall wellbeing and tinnitus severity.
It’s nice to know for me personally, what tinnitus is … but in increase how to manage it, which is what the sleep intervention assisted in, because I think the more sleep I’m getting, … the far, far, better the tinnitus is becoming. (Declan)
Structure and routine were not possible for everyone due to shift work or unplanned life events. Hannah underlined that due to her unusual work patterns she could not always keep the routine, because sometimes she was coming home after her bedtime, it was “hard to unwind” and go straight to bed after work.
Feeling more confident
After completing the treatment all participants mentioned that they felt more confident and less anxious about coping with tinnitus and insomnia in the future. Participants described being “set for life” (Bella) to deal with future stressors and being equipped with “knowledge and techniques to make tinnitus more manageable” (Declan).
I’ve always got the exercises to go back to if I have problems … I’m feeling happier to accept another time in the future knowing that I can handle my situation now. (Ravi)
The “toolbox” of exercises provided seemed to increase participants’ sense of self-management and internal control. Paul, for example, experienced the tinnitus noise louder after the treatment. In spite of this, he described himself as being able to “cope” with it, since learning the management techniques.
All participants described how their sleep had improved mainly due to sticking to the routine they established during the CBTi course. Everyone described the stabilising effect of time-in-bed-restriction as having a lasting success, leading to longer, and better-quality sleep. The impact included waking up feeling “energised” (Farah) and refreshed in the morning, and performing better during the day, for example with “more analytical thinking” (Bella). Improved sleep was linked to tolerating tinnitus more, underlining the importance of changes in sleep behaviour during treatment.
The benefits of getting a proper night sleep and being refreshed for the day … it’s kind of beneficial all-round … It improved my tinnitus … feeling better with myself, it’s a win-win. (Declan)
Theme 3: accepting the things I cannot change
Allowing tinnitus to be there
Some participants explained how they were frustrated by CBTi being “all about just managing it [tinnitus] rather than actually a cure” (Bella). Those who showed a strong urge to “fix” their tinnitus seemed particularly reluctant to believe in the potential benefits of the treatment at first. Nevertheless, when offered information about the process of habituation, participants gained an understanding of tinnitus and why “fighting” it can be counterproductive.
That explanation of why it feels worse when you pay more attention to it and … when you can get to a place where you don’t see it as a threat, your body will naturally habituate it and tune it out. That was really helpful … - a concrete scientifically physiological cure. (Bella)
There were two strands of changed relationships to tinnitus. One appeared to related to habituation, whereby tinnitus was perceived as less threatening, so participants felt less drawn to attend to it. The other related to acceptance, which felt more appropriate when tinnitus was not something that involves a real threat. Matthew described changing from “trying to fix” to seeing tinnitus as “a part of oneself.” Every participant described how “accepting” tinnitus helped them to shift attention away from the noise, making it less intrusive and more of a “subconscious thing” (Declan).
I learned I shouldn’t be focusing on it and I should accept it and that makes a lot of difference … Now, I know it’s there, I hear it and it doesn’t bother me the same. (Farah)
This shows that participants engaged in a process that increased psychological flexibility. Participants changed their negative thoughts and simply acknowledged the tinnitus and allowed it to be there without judgement or resistance. This change was described as a journey rather than a result.
It started to change … must be third week or the fourth week when I stopped concentrating on the noise of the tinnitus. (Oscar)
Some participants described starting to “accept” their tinnitus after treatment indicating that continued use of treatment techniques was helpful in strengthening the processes of allowance and increased flexibility.
Reliable tinnitus education was important to dispel unhelpful myths about possible cures and about anxiety-provoking information on the internet. For example, for Declan the tinnitus became “less threatening and dominating” when he realised that the noise will not make him deaf. The information seemed to help participants to allow their tinnitus to be present and feel less intimidated by it.
Getting on with life
Most participants described significant differences between before and after treatment, for example, from perceiving going to bed as “torture” (Oscar) “to looking forward to going into bed again” (Bella). This change seemed to require practice over time. Six months after completion of CBTi, participants described “getting on with it” and continuing their life without letting their tinnitus and insomnia be a burden.
I learned to accept well, I’ve got the tinnitus, let’s just crack on with it … don’t let it … let parties or anything like that off… At the end of the day, there is no cure for it … you just got to get on with it. (Paul)
Participants received information about tinnitus that highlighted the benefits of adaptation. Participants stopped being “stuck” in a vicious cycle of perceiving tinnitus as a threat and fighting it hopelessly. After treatment they seemed to be less focussed on their tinnitus and how their future might be destroyed by it; they were more focussed on living their life in the present, and how they could adapt to live alongside tinnitus. Additionally, participants learned that they could sleep “normally” even with audible tinnitus; this change reduced worries about deficient sleep and allowed more positive and relaxed responses:
Coming to this group made me look at it a bit differently … I still get the bad night sleep and stuff, but I don’t worry about it, I don’t worry about sleep in the day. It is what it is. Sleep isn’t really something that you should think about (Matthew).
Ravi described not thinking about sleep anymore and going to bed “as any normal person … not occupied thinking about tomorrow” as he concluded “even if you had a bad night you can get through that.”
Discussion
The present study sought to explore the experiences of chronic tinnitus sufferers who had received CBTi. Three overarching themes were identified: “Common humanity and transcending individual distress,” “Changing the things I can” and “Accepting the things I cannot change.” Findings indicate that participants experienced CBTi as a treatment that helped them to improve sleep and reduce tinnitus distress. This is in line with clinical evidence showing that tinnitus distress and insomnia improve after CBTi (Marks et al. Citation2022), and extends our understanding of the ways in which such changes may occur. The group setting of CBTi embraced common humanity and transcended individual suffering, associated with increased kindness to self and others, and motivation to engage with more challenging aspects of treatment. Reliable tinnitus and sleep information helped participants to understand the possibility of effective action, enabling them to focus their efforts on the most helpful approaches to change and expend less effort on less helpful behaviours (e.g. “fighting it”). Structured behavioural approaches including time-in-bed-restriction, sleep hygiene and relaxation were seen to have had important impacts on sleep, to have improved tinnitus tolerance, and increased feelings of self-efficacy when facing current and future stressors. Cognitive techniques supported a shift in perspective, where tinnitus was “allowed” and accepted, rather than being something to escape or remove. Together these changes seemed to create confidence within the participants, enabling them to live their lives more fully, with less worry about the future. These findings offer important insight into the aspects of CBTi that may be of particular benefit to this population.
The benefits of a group-based therapy for tinnitus aligns with other findings in this area. Participants recognised the value of seeing other people in the same situation, sharing and understanding their suffering. Identification with other group members can normalise challenging experiences; this process was echoed in the current participants’ experiences of tinnitus-related distress and insomnia. Similarly, Thompson, Pryce and Refaie (Citation2011), observed that that group and peer interaction led to greater validation of feelings and reduced isolation, compared to individual therapy. Thompson, Pryce and Refaie (Citation2011) also noted that group participants focussed more on downward comparisons (“mine is not that bad”) than upward ones (“I could be like that”) than did people in individual therapy; a similar process is reported here. Furthermore, the group offered another type of support, that of kindness and motivation. This allowed upward comparisons to be helpful. Seeing other group members improve created a sense of warmth and happiness for the other, and confidence that the individual would be able to engage in a similar task and benefit from it. This fits with evidence that seeing the success of others positively reinforces behaviours (Morrison Citation2001).
However, there was some variability in how comparisons were made, and there were some potential pitfalls relating to group dynamics, where more difficult feelings arose in relation to others. This included guilt or self-blame from downward social comparisons, one’s tinnitus is less intrusive than another’s. Upward social comparisons caused additional pressure, for example if individuals perceived their own progress as slower than their peers, engendering difficult feelings such as hopelessness and self-critical thoughts or unrealistic expectations, which in turn could increase the self-applied pressure on sleep. Such findings indicate potential internal barriers (negative views, self-doubts) to recovery that might be exacerbated by the group, and also affect the wellbeing of participants and the cohesion of the wider group. Group therapy should therefore proceed with care, and facilitators must be aware of the different responses of participants to group dynamics and social comparisons, and address this as part of the group, to minimise unhelpful social comparisons, normalise a range of responses and build strong relationships between group members when possible (see ).
The second theme highlighted how important skills training was in helping participants to feel more in control and resilient. In line with other research it was, however, apparent that preferences for different techniques varied across participants (Greenwell et al. Citation2019; Pryce et al. Citation2018). For example, Pryce et al. (Citation2018) found that identifying a preference was part of patients developing coping strategies and control, whether via physical devices or cognitive strategies. This points to the importance of multicomponent treatments for mixed groups, and the ability to offer an intervention than can enhance a sense of control. Increasing control can reduce worry which, in turn, may improve tinnitus tolerance and resilience.
Few participants described techniques as “irritating” (sound enrichment), anxiety inducing (breathing exercise) or “unhealthy” (thought challenging technique). Those findings give valuable information about possible detrimental effects of the treatment, meaning the programme could have potential to increase depressive or anxious thoughts and feelings, and that careful facilitation and follow up is important.
The theme of “Accepting the things I cannot change” is found across the treatment literature in tinnitus, where acceptance is correlated with improved quality of life in tinnitus sufferers (Riedl et al. Citation2015). Acceptance describes a shift from focussing on “curing” tinnitus and trying to fight it, to understanding how to allow and accept tinnitus as part of life, which, in turn, enables the individual to move forwards. This finding is interesting as CBTi is not ostensibly an acceptance-based approach, yet the thread of acceptance ran throughout different themes and arose alongside specific cognitive and behavioural aspects of the intervention. This included reliable information and peer discussion that helped participants to perceive tinnitus as less scary and more part of oneself. Strategies such as time-in-bed-restriction and relaxation led to improved sleep which appeared to make thinking less catastrophic and reduce the need to change things, so creating space for a new, more accepting response to tinnitus. Acceptance has been identified as a significant process and outcome in other acceptance-based psychological treatments for tinnitus. This includes Mindfulness-Based-Cognitive-Therapy for tinnitus (MBCT-t) where people shift from “fighting” to “allowing” tinnitus (Marks, Smith, and McKenna Citation2020) and Acceptance-and-Commitment-Therapy (ACT), where improvements in distress have been found to be mediated by changes in tinnitus acceptance (Westin et al. Citation2011). CBTi appears to involve a similar experience of adjustment and acceptance, whilst also leading to significant reductions in sleep disturbances.
Strengths and limitations
This novel study is the first to explore how people with tinnitus-related insomnia experience CBTi and offers unique insight into potential processes of change. The TA approach offers meaningful insight into how tinnitus sufferers experience CBTi, leading to clinical recommendations (). Although not all participants receiving CBTi were interviewed, results were based on a sample that was representative of those taking part in the RCT, as the trial data indicates that almost all participants receiving CBTi were well engaged in treatment (only 2 of 33 CBTi participants − 6% - did not complete treatment) and 80% reported improved insomnia at the end of treatment (Marks et al. Citation2022). Even so, those participants who took part in the interview study had all completed therapy so were likely to be motivated and positive. More diverse results and valuable insight into the contextual factors affecting outcome and experience could have been provided by purposefully sampling to include non-completers. Interviews were lengthy and conducted by one of the facilitators of CBTi which encouraged participants to disclose rich and detailed information. The interviewer was, however, a therapist in the trial, which could have led to some positive response bias, so the interviewer encouraged participants to be honest about the negative experiences as well as the positive ones. Participants reflected a range of ages and genders, although all participants were Caucasian, and the majority reported having received a tertiary education. Furthermore the study was performed at one clinical setting. These issues limit the transferability of findings to a more diverse sample and other settings, and future research should attempt broader recruitment strategies to improve diversity. This is particularly relevant for education as CBTi does include an educational component which could exacerbate health inequalities if not appropriately delivered. To avoid the risk of developmental insomnia contributing to sleep disorder in the participants, an upper age limit of 70 years was set as an inclusion criteria, but this does limit the applicability of the findings to adults in later life. Interviews were conducted more than six months after treatment completion, which allowed assessment of longer-term impacts, embedding of skills, reflection upon learning and identification of changes since finishing therapy. This, however, could also affect accuracy of memory recall especially of effects that may not have been so long-lasting. Although eight participants were interviewed and very similar themes were found across participants, indicating code saturation, a larger sample size could have led to further insights and development of further meaning.
Future research should aim to develop larger scale trials that allow for the assessment of potential causal pathways and mediators of change. Findings here indicate that key elements of CBTi for tinnitus include both therapy-specific elements (psychoeducation, relaxation, sleep restriction, stimulus control) and group-specific elements (social support, awareness of others suffering), and dismantling trials and measurement of mediators such as “belongingness” to the group could be used within future trials to develop logic models which could then be used to refine and improve interventions.
Conclusion
This is the first study to offer direct insight into tinnitus sufferers’ experiences of receiving CBTi to treat tinnitus-related insomnia. Qualitative findings indicate benefits of group therapy including mutual understanding, support and motivation, although care must be taken to manage potential pitfalls from group therapy, including unhelpful social comparisons. Cognitive and behavioural approaches of CBTi allowed focus on both insomnia and tinnitus, which enabled participants to feel more accepting of tinnitus, which appeared to reduced distress. Learning practical sleep tools was an effective way of improving sleep and increasing confidence and activity. Individual lifestyles, preferences and needs needed to be considered to tailor the treatment to each participant. Future research could explore if such benefits arise in a more diverse sample of tinnitus sufferers receiving CBTi, particularly those who did not complete all treatment sessions.
Ethical approval
Ethical approval was granted for the trial by the London-Camden and Kings Cross NHS Research Ethics Committee and for the reflective study by the University of Bath Research Ethics Committee, 21-052.
Informed consent
Informed written consent to take part in the qualitative study has been obtained by all eight participants prior to the interviews.
Author contributions
EM led and designed the study, collected the data and contributed to analysis and write up. LC supported the study design, transcribed and analysed the data and contributed to write up. FV and LM contributed to data analysis and write up.
Supplemental Material
Download MS Word (18.3 KB)Acknowledgements
We thank the patients who took part in the study. The trial was conducted as a collaboration between the Royal National Ear, Nose and Throat and Eastman Dental Hospital, University College London Hospitals, London, UK and the University of Bath, UK.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. Clinical Trial registration: NCT03386123.
Additional information
Funding
References
- Aazh, H., and B. Moore. 2019. “Tinnitus Loudness and the Severity of Insomnia: A Mediation Analysis.” International Journal of Audiology 58 (4):208–212. doi:10.1080/14992027.2018.1537524.
- Asnis, G. M., K. Majeed, M. A. Henderson, C. Sylvester, M. Thomas, and R. D. La Garza. 2018. “An Examination of the Relationship between Insomnia and Tinnitus: A Review and Recommendations.” Clinical Medicine Insights: Psychiatry 9:117955731878107. doi:10.1177/1179557318781078.
- Baguley, D., D. McFerran, and D. Hall. 2013. “Tinnitus.” Lancet 382 (9904):1600–1607. doi:10.1016/S0140-6736(13)60142-7.
- Beukes, E. W., V. Manchaiah, A. S. A. Davies, P. M. Allen, D. M. Baguley, and G. Andersson. 2018. “Participants’ Experiences of an Internet-based Cognitive Behavioural Therapy Intervention for Tinnitus.” International Journal of Audiology 57 (12):947–954. doi:10.1080/14992027.2018.1514538.
- Braun, V., and V. Clarke. 2020. “One Size Fits All? What Counts as Quality Practice in (Reflexive) Thematic Analysis?” Qualitative Research in Psychology 18 (3):328–352.
- Braun, V., and V. Clarke. 2021. “To Saturate or Not to Saturate? Questioning Data Saturation as a Useful Concept for Thematic Analysis and Sample-size Rationales.” Qualitative Research in Sport, Exercise and Health 13 (2):201–216. doi:10.1080/2159676X.2019.1704846.
- Crönlein, T., B. Langguth, M. Pregler, P. M. Kreuzer, T. C. Wetter, and M. Schecklmann. 2016. “Insomnia in Patients with Chronic Tinnitus: Cognitive and Emotional Distress as Moderator Variables.” Journal of Psychosomatic Research 83:65–68. doi:10.1016/j.jpsychores.2016.03.001.
- Eysel-Gosepath, K., and O. Selivanova. 2005. “Charakteristik der Schlafstörungen bei Patienten mit Tinnitus [Characterization of Sleep Disturbance in Patients with Tinnitus].” Laryngo- Rhino- Otologie 84 (5):323–327. doi:10.1055/s-2005-861020.
- Greenwell, K., M. Sereda, N. Coulson, A. El Refaie, and D. J. Hoare. 2016. “A Systematic Review of Techniques and Effects of Self-help Interventions for Tinnitus: Application of Taxonomies from Health Psychology.” International Journal of Audiology 55 (sup3):S79–S89. doi:10.3109/14992027.2015.1137363.
- Greenwell, K., M. Sereda, N. S. Coulson, A. W. A. Geraghty, K. Bradbury, and D. J. Hoare. 2021. “That’s Just How I Am”: A Qualitative Interview Study to Identify Factors Influencing Engagement with a Digital Intervention for Tinnitus Self Management.” British Journal of Health Psychology 26 (3):727–747. doi:10.1111/bjhp.12486.
- Greenwell, K., M. Sereda, N. S. Coulson, and D. J. Hoare. 2019. “Understanding User Reactions and Interactions With an Internet-based Intervention for Tinnitus Self-management: Mixed-methods Evaluation.” American Journal of Audiology 28 (3):697–713. doi:10.1044/2019_AJA-18-0171.
- Hoare, D. J., V. L. Kowalkowski, S. Kang, and D. A. Hall. 2011. “Systematic Review and Meta-analyses of Randomized Controlled Trials Examining Tinnitus Management.” The Laryngoscope 121 (7):1555–1564. doi:10.1002/lary.21825.
- Kim, H. J., H. J. Lee, S. Y. An, S. Sim, B. Park, S. W. Kim, J. S. Lee, S. K. Hong, and H. G. Choi. 2015. “Analysis of the Prevalence and Associated Risk Factors of Tinnitus in Adults.” PLoS One 10 (5):e0127578. doi:10.1371/journal.pone.0127578.
- Marks, E., C. Hallsworth, F. Vogt, H. Klein, and L. McKenna. 2022. “Cognitive Behavioural Therapy for Insomnia (CBTi) as a Treatment for Tinnitus-related Insomnia: A Randomised Controlled Trial.” Cognitive Behaviour Therapy. doi:10.1080/16506073.2022.2084155.
- Marks, E., P. Smith, and L. McKenna. 2020. “I Wasn’t at War with the Noise: How Mindfulness Based Cognitive Therapy Changes Patients’ Experiences of Tinnitus.” Frontiers in Psychology 11:483. doi:10.3389/fpsyg.2020.00483.
- McKenna, L., L. Handscomb, D. J. Hoare, and D. A. Hall. 2014. “A Scientific Cognitive- behavioral Model of Tinnitus: Novel Conceptualizations of Tinnitus Distress.” Frontiers in Neurology 5:196. doi:10.3389/fneur.2014.00196.
- Mills, A., G. Durepos, and E. Wiebe. 2010. “Reflexivity.” In Encyclopedia of Case Study Research, edited by D. Begoray and E. Banister, 789–790. California: Sage.
- Moller, A. R. 2007. “Tinnitus and Pain.” Progress in Brain Research 166:47–53. doi:10.1016/S0079-6123(07)66004-X.
- Morrison, N. 2001. “Group Cognitive Therapy: Treatment of Choice or Sub-optimal Option?” Behavioural and Cognitive Psychotherapy 29 (3):311–332. doi:10.1017/S1352465801003058.
- NICE (National Institute for Health and Care Excellence) 2020. Tinnitus: Assessment and Management. March 11. https://www.nice.org.uk/guidance/ng155/chapter/Recommendations#management-of-tinnitus
- Okajima, I., Y. Komada, and Y. Inoue. 2011. “A Meta-analysis on the Treatment Effectiveness of Cognitive Behavioral Therapy for Primary Insomnia.” Sleep and Biological Rhythms 9 (1):24–34. doi:10.1111/j.1479-8425.2010.00481.x.
- Potter, J., and M. Wetherell. 1987. Discourse and Social Psychology: Beyond Attitudes and Behaviour. Sage Publications, Inc.
- Pryce, H., A. Hall, R. Shaw, B. A. Culhane, S. Swift, J. Straus, and B. Claesen. 2018. “Patient Preferences in Tinnitus Outcomes and Treatments: A Qualitative Study.” International Journal of Audiology 57 (10):784–790. doi:10.1080/14992027.2018.1484184.
- Riedl, D., G. Rumpold, A. Schmidt, P. G. Zorowka, H. R. Bliem, and R. Moschen. 2015. “The Influence of Tinnitus Acceptance on the Quality of Life and Psychological Distress in Patients with Chronic Tinnitus.” Noise & Health 17 (78):374–381. doi:10.4103/1463-1741.165068.
- Riemann, D., C. Baglioni, C. Bassetti, B. Bjorvatn, L. Dolenc Groselj, J. G. Ellis, C. A. Espie, et al. 2017. “European Guideline for the Diagnosis and Treatment of Insomnia.” Journal of Sleep Research 26 (6):675–700. doi:10.1111/jsr.12594.
- Schecklmann, M., M. Pregler, P. M. Kreuzer, T. B. Poeppl, A. Lehner, T. Crönlein, T. C. Wetter, E. Frank, M. Landgrebe, and B. Langguth. 2015. “Psychophysiological Associations between Chronic Tinnitus and Sleep: A Cross Validation of Tinnitus and Insomnia Questionnaires.” BioMed Research International 2015:461090. doi:10.1155/2015/461090.
- Shore, S. E., L. E. Roberts, and B. Langguth. 2016. “Maladaptive Plasticity in Tinnitus Triggers, Mechanisms and Treatment.” Nature Reviews. Neurology 12 (3):150–160. doi:10.1038/nrneurol.2016.12.
- Skivington, K., L. Matthews, S. A. Simpson, P. Craig, J. Baird, J. M. Blazeby, K. A. Boyd, et al. 2021. “A New Framework for Developing and Evaluating Complex Interventions: Update of Medical Research Council Guidance.” BMJ (Clinical Research Ed.) 374:n2061. doi:10.1136/bmj.n2061
- Tang, N. K., C. E. Goodchild, J. Hester, and P. M. Salkovskis. 2012. “Pain-related Insomnia versus Primary Insomnia: A Comparison Study of Sleep Pattern, Psychological Characteristics, and Cognitive-behavioral Processes.” The Clinical Journal of Pain 28 (5):428–436. doi:10.1097/AJP.0b013e31823711bc.
- Tang, N. K., C. E. Goodchild, and P. M. Salkovskis. 2012. “Hybrid Cognitive-behaviour Therapy for Individuals with Insomnia and Chronic Pain: A Pilot Randomised Controlled Trial.” Behaviour Research and Therapy 50 (12):814–821. doi:10.1016/j.brat.2012.08.006.
- Thompson, P., H. Pryce, and E. Refaie. 2011. “Group or Individual Tinnitus Therapy: What Matters to Participants?” Audiological Medicine 9 (3):110–116. doi:10.3109/1651386X.2011.604470.
- Wallhäusser-Franke, E., M. Schredl, and W. Delb. 2013. “Tinnitus and Insomnia: Is Hyperarousal the Common Denominator?” Sleep Medicine Reviews 17 (1):65–74. doi:10.1016/j.smrv.2012.04.003.
- Westin, V. Z., M. Schulin, H. Hesser, M. Karlsson, R. Z. Noe, U. Olofsson, M. Stalby, G. Wisung, and G. Andersson. 2011. “Acceptance and Commitment Therapy versus Tinnitus Retraining Therapy in the Treatment of Tinnitus: A Randomised Controlled Trial.” Behaviour Research and Therapy 49 (11):737–747. doi:10.1016/j.brat.2011.08.001.