Abstract
Objective: It is unknown how adults communicate about their experienced listening difficulties with their audiologist. This scoping review aims to explore how adults self-describe the listening difficulties that they experience, and how they communicate about them. Design: A scoping review was conducted between December 2020 and September 2022 to identify published journal articles in which adults described and communicated about their listening difficulties. Study sample: Database searches yielded 10,224 articles initially. After abstract screening and full text review, 55 articles were included for analysis. Results: The listening difficulties that adults described were varied, highlighting the fact that each person has individual experiences. Adults discussed reasons for their listening difficulties, impacts of their listening difficulties, and behavioural responses they adopted to cope with their listening difficulties. Conclusions: This review shows the broad impacts of listening difficulties, and the varied ways in which adults discuss their listening difficulties. There is no available literature reporting how adults communicate about their listening difficulties in a clinical context.
Introduction
Hearing loss is an important and growing public health concern and is the third most common chronic health condition in Australia (Hartley et al. Citation2010). Untreated hearing loss leads to listening difficulties, which can adversely affect both the individual (e.g. fatigue, social isolation) and their social networks (e.g. relationship strain) (Heffernan et al. Citation2019; Vas, Akeroyd, and Hall Citation2017). Hearing aids are often the recommended treatment option for adults with hearing loss (Weinstein Citation1996). Hearing aids can improve access to sound, and may reduce the negative impacts of listening difficulties (Chisolm et al. Citation2007; Weinstein Citation1996). The number of people who own hearing aids, relative to the number of people with hearing loss, is low despite advances in hearing aid technology (NIDCD Citation2021). For example, a population-based survey of older Australian adults found that only 33% of those with bilateral hearing loss owned hearing aids (Chia et al. Citation2007).
One approach to improving hearing aid uptake is ensuring that hearing care is patient-centred (Poost-Foroosh et al. Citation2011). In patient-centred care, the patient’s needs and desired outcomes are at the centre of all healthcare decisions, and decision-making is shared between the patient and the clinician. Importantly, treatment is not only provided based on audiological need, but with the psychological, social and financial needs of patients in mind (Grenness et al. Citation2014b). Previous research in audiology has shown that hearing aid uptake rates are negatively affected by patient-centred care (Laplante-Lévesque et al. Citation2013; Poost-Foroosh et al. Citation2011). Increased hearing aid uptake rates are achieved when patients feel that their audiologist has understood their needs (Poost-Foroosh et al. Citation2011). However, qualitative interviews with audiology patients show that this is not the experience that all patients report (Grenness et al. Citation2014a).
Some patients have reported feeling as if their audiologist does not understand their listening difficulties and does not address their psychosocial concerns (Ekberg, Grenness, and Hickson Citation2014; Glass and Elliot Citation1992; Grenness et al. Citation2014a). Further, a literature review found that audiologists tended not to respond appropriately to the concerns that patients expressed (Manchaiah et al. Citation2019). Thus, the audiologist’s response to concerns that are raised during appointments may contribute to adults reporting that they do not feel understood. One participant in a qualitative interview described their experience thus: “When I leave (I feel) an element of frustration, that I am not being fully listened to, that I’m listened to up to a point, and then there’s an inconvenience, or a difficulty in really following through what she’s saying and a sense of ‘Oh, she’s being very fussy, pedantic, nit picking’. But it’s my hearing and I need to be able to be comfortable that whatever I’ve got, it’s the best that can be done for me at my level of finance, that I’m getting the best outcome that I can get” (Grenness et al. Citation2014a). Research has explored a number of aspects of communication during audiology appointments such as interaction styles, communication patterns and how results are communicated to patients (Grenness et al. Citation2015; Meyer et al. Citation2017; Parmar et al. Citation2022). Most suggestions about how to improve clinical communication are in relation to audiologists’ communication style. Further research is needed to explore how patients currently communicate their listening difficulties, in order to identify how patients could be better supported to communicate more effectively about their experiences. Improving patients’ ability to effectively communicate their experiences may have a positive impact on their perception of audiologists’ understanding of their listening difficulties (Poost-Foroosh et al. Citation2011).
In current audiological practice, audiologists generally assess patients’ experience of listening difficulties using self-report questionnaires or history-taking interviews. These methods of assessment depend on patients’ recollection of their experience, which may result in descriptions lacking detail, or omitting some listening difficulties. Additionally, these methods may lack ecological validity as the domains of enquiry are often pre-determined by the questionnaire or interviewer, and thus may not adequately capture the real-world listening difficulties experienced by patients. To address these limitations, ecologically valid assessment methods, such as ecological momentary assessment (EMA), have been proposed as a feasible method of assessing listening difficulties (Timmer, Hickson, and Launer Citation2017). EMA involves patients documenting and describing their listening difficulties whilst in the listening environment and offers a personalised approach that has the potential to capture the individual nature of listening experiences. Audiologists could assess listening difficulties using EMA, which could be incorporated as part of a digital tool that patients use before their audiology appointments, or as an ongoing way to monitor their own listening difficulties. A tool which supports patients to document their listening difficulties may improve patients’ perceptions of their audiologists’ understanding of their listening experiences, leading to improvements in the quality of patient-centred care. In order to develop a clinical tool which uses EMA, it is essential to have a better understanding of how patients choose to describe their listening difficulties.
Listening difficulties, and the impacts of listening difficulties, have been explored by synthesising reported hearing difficulties from people with hearing loss and classifying them into the following domains: auditory, social and self (Vas, Akeroyd, and Hall Citation2017). Whilst this research has improved the understanding about the impacts of hearing loss, it is unknown whether adults would describe the same listening difficulties with their audiologist. A meta-synthesis of qualitative studies examining the psychosocial experiences of hearing loss indicated that listening difficulties had impacts such as reduced participation or enjoyment of activities, social impacts and emotional impacts (Barker, Leighton, and Ferguson Citation2017). Examples of the social and emotional impacts include effects on relationships between the person with hearing loss and those close to them, being isolated due to reduced social interaction, and negative effects on mood due to the experienced listening difficulties. Barker, Leighton, and Ferguson (Citation2017) also found that people adopted different coping strategies and responded to their listening difficulties in different ways such as withdrawal from their social activities, denial about their hearing loss and use of communication strategies. This meta-synthesis has contributed to understanding about the impacts of hearing loss, although it did not explore how adults communicate about their listening difficulties with their audiologist.
A qualitative synthesis of how adults communicate about their listening difficulties has not been completed to our knowledge. There also appears to be a lack of research exploring how adults choose to communicate about their listening difficulties with their audiologist. A necessary precursor to future work that aims to improve adults’ experiences of communication during audiology appointments, is an improved understanding of adults’ listening difficulties and their preferences for communicating about them. Accordingly, the aim of this review was to explore research literature regarding how adults describe the listening difficulties that they experience, and how they communicate about these difficulties. It was of particular interest to explore how adults describe and communicate about their listening difficulties during clinical encounters, should such research exist.
Methods
A preliminary search of the literature was completed in October 2020 with the assistance of a research librarian. This revealed a lack of literature addressing this topic specifically, and therefore a scoping review was chosen as being the most appropriate review type. Scoping reviews are exploratory, more appropriate for answering broad questions and for highlighting evidence gaps.
A scoping review protocol was followed as described by Peters et al. (Citation2020).
Eligibility criteria
Studies were included for analysis if they met the following criteria:
The study included adults who were experiencing, or had previously experienced, listening difficulties
The participants identified and/or described listening difficulties that they experienced, and/or the impacts of experienced listening difficulties
The study was published in English
Studies were excluded if:
The article type was an opinion piece, editorial, commentary piece, conference abstract or review
Only closed-set response options were offered to the participants, such that they did not self-identify their listening difficulties
The study was published (or data was collected) prior to 1945
Search strategy
Four databases were searched (Medline, EMBASE, CINAHL complete and Web of Science) using the following search terms and Booleans: ((information or history or report* or descri* or perce* or problem* or issue* or difficult*) adj2 (listen* or hearing)) AND (self or adult or client or patient) not child*). The base search was adapted to each database. The search was initially run on 2–3 December 2020. Reference lists of the extracted studies were hand searched for any additional relevant studies. The search was re-run on 2 September 2022 to ensure inclusion of recent publications.
Study selection and data extraction
Search results were uploaded to the Covidence systematic review software (Citation2021). This is a web-based software which streamlines the production of systematic and other literature reviews. Duplicates were removed and the titles and abstracts were screened independently by two authors. Irrelevant studies were excluded. In cases where the screening authors disagreed about the relevance of a study, a third author cast a deciding vote. Included studies were then assessed for eligibility based on the full text of the article. Two authors (ZM and GN) read each full-text article and voted for its inclusion or exclusion. When there was disagreement on the decision to include a study, or on the reason for its exclusion, authors ZM and GN discussed their reasoning in order to reach a consensus. All title and abstract screening from the September 2022 literature search was completed by ZM. Included studies were then assessed for eligibility by two authors (ZM and KG) based on the full text article.
A data extraction form was developed by ZM and agreed upon by all authors. It was then piloted with the first five articles. Minor changes were made such that the final form captured the following information from each study: year published, country in which the study was conducted, aim(s), research question(s), study design, sample size, key demographic details (age, gender, hearing levels), inclusion criteria, recruitment setting, prompt(s) used to elicit information about listening difficulties and/or their impacts, and study findings, including supporting quotes from participants. Author ZM completed the data extraction process and met weekly with authors KG, BT and DT during the process to ensure that all relevant data was being extracted and to reflect on the accumulating results. A critical appraisal of article quality was not performed in line with current scoping review methodological recommendations (Peters et al. Citation2020).
Data synthesis
A thematic approach was determined as the most appropriate to synthesise the data collated in this review. The general method adopted is described in Braun and Clarke (Citation2006), however the authors also referred to Thomas and Harden (Citation2008), who describe a method of analysis which is specific to undertaking reviews. Thomas and Harden (Citation2008), discuss how they adopted methods commonly used in thematic analysis of primary research and used the term thematic synthesis to describe the application of thematic analysis in reviews.
Thematic synthesis occurred in three stages. In the first stage, extracted study findings and direct quotes were imported into the qualitative analysis software, QSR NVivo. Line-by-line coding of the resulting text was completed according to meaning and content. Codes were grouped into categories and reviewed by the authors in order to check the accuracy and consistency of interpretation. Most sentences had at least one code applied, and many were categorised using multiple codes. The second stage of synthesis was to create new codes which captured the meaning of groups of the initial codes. These new codes were termed descriptive themes. A summary of each theme was written by author ZM, which contained a summary of the study findings contributing to the theme, with supporting quotes extracted from the articles. The third stage of synthesis involved creation of analytical themes. Themes were developed based on the research question, as well as on the judgement and insights of those conducting the research (Thomas and Harden Citation2008). The descriptive themes were discussed by all the authors together. This resulted in the development of the final key themes.
Results
Literature search
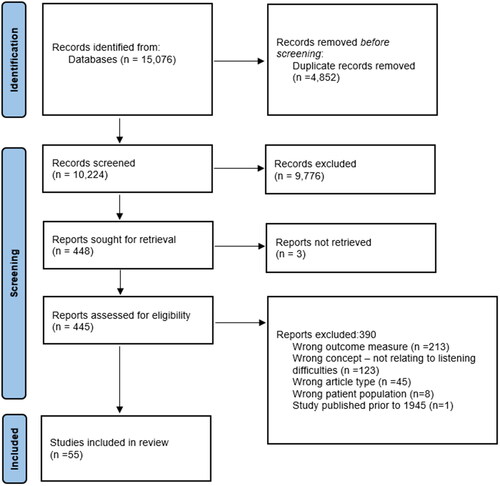
Literature searches were completed in September 2022. Search results were uploaded to the Covidence software for screening. Duplicates were removed, leaving 10,224 studies to be screened. After screening titles and abstracts, 9,776 studies were removed. This left 448 studies to be assessed for eligibility based on the full-text article, however 3 full-text articles were unable to be retrieved. Therefore, 445 full-text articles were assessed by the authors. There were 383 studies excluded for not meeting the inclusion criteria, and 62 studies were included for data extraction and analysis. However, a further 7 studies were excluded during this phase as they did not meet the inclusion criteria, meaning that 390 studies were excluded at the full text stage, and 55 studies were included for the final analysis. For summary details of the study search and selection, see .
Characteristics of included studies
Study characteristics are presented in . The aims and references for the included studies are presented in supplemental Appendices A and B respectively within the supplemental material. All data included in the analysis was qualitative. Interviews (structured or semi-structured), focus groups, questionnaires and case histories were the methods of data collection used. Studies with questionnaires were only included if they consisted of at least some open-ended questions. Sample sizes in the included studies ranged from 1 to 4,266. The age of participants was varied, however all were adults. Across the included studies, all participants experienced listening difficulties, and had hearing loss of varying degrees, ranging from normal hearing to profound hearing loss. Participant groups were comprised of both hearing device users and non-hearing device users. The location of the study was varied, with 21 studies from the United Kingdom, 11 from the United States, 7 from Canada, 5 from Australia, 2 from multiple countries, 2 from Sweden, 2 from Denmark, and 1 each from Spain, New Zealand, Netherlands, China and Italy. Three key themes and their sub-categories are shown in .
Figure 2. Map representing how adults describe their listening difficulties, and what they communicate about them.
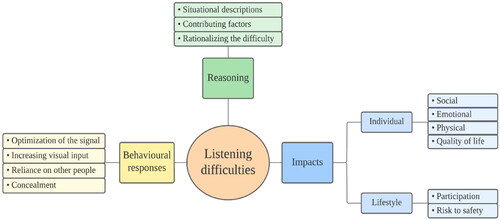
Table 1. Summary of included studies showing methodological characteristics and participant details.
Reasoning and explanations for listening difficulties
Adults provided descriptions of situations or contexts in which they experienced listening difficulties. They reported difficulty understanding amplified speech, such as through television, radio, or telephone. They also reported experiencing listening difficulties in background noise, group conversations, at church, in the workplace, during medical encounters, or when listening to music. Adults also described difficulty when taking part in quiet or confidential conversations.
I am a trial lawyer and I had to apply for disability retirement last fall because it got to a point where in good conscience, I didn’t feel like I was being fair to my clients because of all the nuances involved with examining a witness. Not only in hearing a witness, but in hearing the manner in which a witness is responding.” (Tye-Murray, Spry, and Mauzé Citation2009)
Some adults discussed difficulty with hearing environmental sounds, some of which were designed to be warning sounds. Examples in this category included doorbells, telephone rings, equipment or machinery sounds, or car indicators.
A lot of times you’ll just be in the area by yourself and if you can’t hear that little whistling noise, something that’s a little bit out of the ordinary, it could be very dangerous. (Morata et al. Citation2005)
The reasoning for adults’ listening difficulties often included discussion of the factors that contributed to making listening difficult. Adults discussed physical characteristics such as reverberant environments or rooms with hard surfaces. They also discussed speaker characteristics and behaviours which contributed to listening difficulty. Examples of these contributing factors were certain voice pitches, unfamiliar voices, fast speech, mumbling, situations in which the speaker’s voice trailed off at the end of sentences, or when adults were unable to view the speaker’s face.
People are mumbling and do not move their lips or articulate adequately…you can’t even lip-read what they are saying. (Hallberg and Barrenäs Citation1995)
I couldn’t hear what he [specialist doctor] was saying at all. I told him but he maintained his original tone. I was pushed out of the door very quickly. He could have spoken louder. He could have looked at me. He could have spoken more slowly. (Skøt et al. Citation2017)
The emotional state of adults could also contribute to their experienced listening difficulties.
I suspect the times I hear better are the times when I’m calmer. (Pryce Citation2003)
Adults provided reasons for the difficulties experienced. In some cases, they attempted to rationalise the difficulty by providing alternative explanations for communication breakdowns, which sometimes suggested a lack of awareness of their own listening difficulties.
People were trying to convince me that I had hearing loss but I kept convincing myself that people just didn’t speak loud enough or they weren’t clear enough. (Pike et al. Citation2022)
Behavioural responses to listening difficulties
Adults described actions they would take in response to listening difficulties, or perceived future listening difficulties. A common response to listening difficulties was to optimise the signal, which was most often a speech signal. They described increasing the volume of the television or radio for example, reducing background noise whilst communicating, or preparing for listening situations by positioning themselves in the optimal location for listening. As one participant described: “I would always go down before and review the room. I would always try to be early so that I could sit right at the front…” (Tye-Murray, Spry, and Mauzé Citation2009).
Another behavioural response to listening difficulties was initiating a change, for example adults changed their own positioning, in order to make use of visual cues.
I’ve got to concentrate and look at people more. Now, when people speak to me, I look at their face. Before, you could have talked to me and if I was writing something then I wouldn’t bother looking at them. Now, I have to look at people when they talk to me. (Holman et al. Citation2019)
They also discussed their preference to use written communication or gesture where possible. An example of this was their preference to communicate via email. Adults spoke about writing notes rather than lipreading “because you don’t want to miss anything. Many words look the same on the mouth,” (Iezzoni et al. Citation2004).
Reliance on others for communication assistance was a strategy used by adults, where they could ask others for repeats in the case of communication breakdown.
Two participants spoke of finding someone with receptive body language to sit by in airports so that they could ask the person to repeat public address system announcements. (Tye-Murray, Spry, and Mauzé Citation2009)
The final type of behavioural response was concealment of listening difficulties. Adults reported pretending to hear, in an effort to cover up that they were missing parts of the conversation, or to avoid disrupting the conversation.
I’d pretend that I understand the subject matter and I keep saying yes, yes, but at the same time I’m trying to figure out what he’s saying and, any, all the time it would become a disaster…. (Bain, Scott, and Steinberg Citation2004)
Some adults reported that they avoided disclosing their experienced listening difficulties for a variety of reasons including embarrassment, discomfort or because it was easier to conceal than explaining them to others. One participant described a situation of pretending to hear and how this affected their participation in conversations. “I get the thread of the conversation when it starts, and then other people put their five pennies in and then I just don’t get it and I just go blank and just smile a lot,” (Dixon et al. Citation2020).
Impacts of listening difficulties
The impact of listening difficulties could be classified as impacts on the individual and their wellbeing or impacts on their lifestyle. Listening difficulties had the potential to affect the individual’s quality of life through their broad effect on individual wellbeing. The social, physical and emotional impacts of listening difficulties also affected individual wellbeing.
Social impacts of listening difficulties involved reduced participation in social settings as a result of their difficulties. Sometimes, adults’ responses to their listening difficulties contributed to the social impacts that they experienced. For example, adults may avoid attending a social setting in the first place or remove themselves from a challenging social setting.
If I can get out of going to an event I do, because I wouldn’t be able to enjoy the conversation…I wouldn’t be able to hear properly. (Lucas, Katiri, and Kitterick Citation2018)
At other times, adults would remain in the situation, however, would be unable to fully engage or participate. One participant described how this occurs: “The noise level goes up and up and up and if I’m talking to you, I can’t hear you clearly and I’d miss out on every third word you say. Then I get frustrated and start switching off,” (Holman et al. Citation2019).
Listening difficulties led to social isolation and reduced value or enjoyment of social situations. Listening difficulties could also affect social relationships. Sometimes this was due to listening difficulties affecting their ability to develop and maintain social relationships. In some cases, it was the impact of the listening difficulties on communication partners that led to frustration and tension.
My son gets annoyed with me because when he phones me up and I give him all the wrong answers. (Holman et al. Citation2019)
Some additional aspects of listening difficulties which affected adults socially were difficulty following humour, interpreting social cues or participating in intimate or confidential conversations.
You miss the punch line, you start laughing after everybody is finished laughing. (Bain, Scott, and Steinberg Citation2004)
Impacts on physical wellbeing related to the increased stress and fatigue experienced by adults. They commonly discussed the need for increased listening effort in an attempt to overcome their listening difficulties.
I do find it tiring [hearing impairment] because I feel that I’ve got to put additionally an extra focus on when people are speaking… by the end of a working day for me or any day in general I feel quite tired with it because I feel I’m having to focus more, lip read more, or you know face people more that sort of thing and I would say it adds a certain amount of stress to you. (Holman et al. Citation2019)
Adults discussed emotions they experienced resulting from their listening difficulties. These were feelings of sadness, loss, anxiety, worry, fear, irritation, embarrassment, or discomfort.
As a musician and conductor, the discernment of sound quality, pitch and balance are crucial. As a result of the deficit I have become frustrated and depressed. (Greasley, Crook, and Fulford Citation2020)
I frequently had to ask somebody to repeat instructions about something I hadn’t done before. And it’s embarrassing for you. If somebody is saying something very simple, not anything intense or deep, and you haven’t understood it. (Tye-Murray, Spry, and Mauzé Citation2009)
They also reported that they felt as if they were dependent on others, or burdensome, due to their listening difficulties. Another aspect of the emotional impact of listening difficulties related to adults’ perceptions of themselves. Adults discussed their own self image as a person with listening difficulties, but also reported how they felt they were perceived by others. One participant described how their behavioural response and coping strategy for listening difficulties may have caused others to form a perception about them. “I actually made an effort not to talk to people…So when I would be around people I would probably have my head stuck in a book. So I probably came across as quite ignorant and unapproachable. After I got my hearing aids somebody did actually say to me that they had been worried because I had been so quiet…and they thought…I was a loner,” (Heffernan et al. Citation2016).
The lifestyle impacts of listening difficulties related to participation and risks to safety. Participation across a broad range of situations was discussed. Situations reported were similar to those described in the reasoning theme, however the impact of these was demonstrated by describing how participation was affected. As an example, this description shows the impact of listening difficulties within a workplace: “I’m a pharmacist. I couldn’t take phone calls. I couldn’t speak to doctors on the phone. I really couldn’t interact with staff,” (Dixon et al. Citation2020).
The risk to safety was relevant when warning sounds were not heard and was described in relation to traffic or workplace machinery.
Now particularly where I am very vulnerable, and I’ve already been knocked down is out on the road. They expect people to move. Well, if you don’t hear them, you can’t move. (Gallagher and Woodside Citation2018)
Discussion
This review of the literature has contributed to the current understanding of adults’ listening difficulties by providing a comprehensive synthesis of adults’ qualitative descriptions of their listening difficulties. Findings show that adults communicate about their listening difficulties by explaining contextual details and factors which contribute to their listening difficulties, by describing their own behavioural responses to their listening difficulties, and by discussing the impacts of their listening difficulties. The range of descriptions within the themes were broad, for example, there were many different locations in which listening difficulties were experienced. From this, we can infer that listening difficulties are individualised. This is consistent with studies which showed that perceived communication and psychosocial impacts resulting from listening difficulties are individualised and cannot be predicted by audiometric results alone (John, Kreisman, and Pallett Citation2012; Newman et al. Citation1997). Adults have emphasised the importance of being able to tell their own story to their clinician both within the field of audiology (Laplante-Lévesque, Hickson, and Worrall Citation2010), and within other areas of healthcare, such as for people with diabetes (Entwistle et al. Citation2008). Adults reported that having the opportunity to describe their experiences was linked to improved perceptions of their involvement in decision-making with their audiologist (Laplante-Lévesque, Hickson, and Worrall Citation2010). Importantly, no study included in this review asked participants to describe their listening difficulties in their own words, nor did any study explore how participants choose to describe and communicate about their listening difficulties.
Some of the studies included in this review limited their focus to listening difficulties in a specific context or to exploring a particular aspect of listening difficulties. For example, Vaisberg et al. (Citation2019) explored challenges related to music listening for instrumentalists. Supplemental Appendix A, in the supplemental material, contains a summary of the aim of each included study highlighting that the range of contexts, in which listening difficulties were investigated, was broad. By including all studies containing qualitative descriptions of listening difficulties, even those in which the focus was limited, this review contributes to an improved understanding of listening difficulties within multiple contexts. This was considered a strength, as this review contains detailed descriptions of listening difficulties that may have been lost if studies with a limited focus had been excluded. It is not clear whether adults would provide detailed descriptions of their listening difficulties if the focus was not limited, and questions were asked in a more general way. Participant characteristics provided in the included studies generally reflects diversity among the participants. It is important to note that in some cases, information about participant characteristics was missing. Specifically, 27 out of the 55 included studies, did not report the hearing levels of their participants. This makes the generalisability of findings difficult to determine.
Another limitation of the studies included in this review is that the setting in which adults described their listening difficulties was not always clear. In the absence of explicit descriptions of who participants were describing their listening difficulties to, and through examination of study methodologies, it could only be assumed that most studies involved participants describing their listening difficulties to the researcher. Patients with chronic health conditions may share different information about their health with their providers, compared to other people, for example, family members (Lim et al. Citation2016). This review did not uncover literature exploring how adults describe their listening difficulties to their audiologist in a clinical setting, thus it is unknown whether the descriptions of listening difficulties found in this review, are consistent with those that adults describe in clinical settings.
For adults, successfully communicating about their listening difficulties with their audiologist is an important component of patient-centred care (Grenness et al. Citation2014a). Lim et al. (Citation2016) explored how patients with multiple chronic health conditions choose to communicate with their healthcare providers, however, adults’ preferences for how they communicate their concerns with their audiologist remains unknown. There is a need to further explore what adults choose to communicate about with their audiologist, as well as what they feel they are not successfully communicating to them. A digital tool that incorporates EMA may address the challenges faced by adults when describing their listening difficulties (Galvin et al. Citation2022; Galvin et al. Citation2023). By allowing adults to record their listening difficulties in real-time, such a tool could minimise the negative impacts of relying on long-term memory recall (Bradburn, Rips, and Shevell Citation1987; Shiffman and Stone Citation1998). While the tool could be implemented using traditional pen and paper mediums, research indicates that smartphones offer improved compliance and accuracy of data collection (Galvez et al. Citation2012; Timmer, Hickson, and Launer Citation2017). Clinician focus groups, and unpublished data from consumer focus groups, supported the use of a digital tool in this way (Galvin et al. Citation2022; Galvin et al. Citation2023). Providing a means for adults to accurately document their own listening experiences, may support them to be able to communicate about their listening difficulties in a way that they perceive to be successful.
Conclusion
This scoping review found that when adults describe their listening difficulties, they often describe details about the situation and context, and provide reasoning for their experienced difficulty. Additionally, they often communicate about their own behavioural responses to their listening difficulties, and the impacts of their listening difficulties. This review did not uncover any literature exploring what adults are not successfully communicating about their listening difficulties. It also did not uncover any literature regarding what adults would choose to communicate about their listening difficulties in a clinical setting. This is significant as adults report feeling that their audiologist does not understand their listening difficulties. However, it is unclear what adults would choose to tell their audiologist in order to facilitate their audiologist’s ability to understand and address the adult’s listening difficulties. Future research could explore what adults feel they are not successfully communicating to their audiologist, and the development of a clinical tool which allows adults to document their listening difficulties to facilitate individualised communication with their audiologist.
Supplemental Material
Download MS Word (36.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [NIDCD] National Institute on Deafness and Other Communication Disorders. 2021. Statistics and Epidemiology: Hearing, Ear Infections and Deafness. https://www.nidcd.nih.gov/health/statistics
- Bain, L., S. Scott, and A. G. Steinberg. 2004. “Socialization Experiences and Coping Strategies of Adults Raised Using Spoken Language.” Journal of Deaf Studies and Deaf Education 9 (1):120–128. https://doi.org/10.1093/deafed/enh001
- Barker, A. B., P. Leighton, and M. A. Ferguson. 2017. “Coping Together with Hearing Loss: A Qualitative Meta-Synthesis of the Psychosocial Experiences of People with Hearing Loss and Their Communication Partners.” International Journal of Audiology 56 (5):297–305. https://doi.org/10.1080/14992027.2017.1286695
- Bradburn, N. M., L. J. Rips, and S. K. Shevell. 1987. “Answering Autobiographical Questions: The Impact of Memory and Inference on Surveys.” Science (New York, N.Y.) 236 (4798):157–161. https://doi.org/10.1126/science.3563494
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2):77–101. https://doi.org/10.1191/1478088706qp063oa
- Chia, E. ‑M., J. J. Wang, E. Rochtchina, R. R. Cumming, P. Newall, and P. Mitchell. 2007. “Hearing Impairment and Health-Related Quality of Life: The Blue Mountains Hearing Study.” Ear and Hearing 28 (2):187–195. https://doi.org/10.1097/AUD.0b013e31803126b6
- Chisolm, T. H., C. E. Johnson, J. L. Danhauer, L. J. P. Portz, H. B. Abrams, S. Lesner, P. A. McCarthy, and C. W. Newman. 2007. “A Systematic Review of Health-Related Quality of Life and Hearing Aids: Final Report of the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults.” Journal of the American Academy of Audiology 18 (2):151–183. https://doi.org/10.3766/jaaa.18.2.7
- Covidence systematic review software [Computer software]. 2021. Veritas Health Innovation. Melbourne, Australia. www.covidence.org
- Dixon, P. R., D. Feeny, G. Tomlinson, S. Cushing, J. M. Chen, and M. D. Krahn. 2020. “Health-Related Quality of Life Changes Associated with Hearing Loss.” JAMA Otolaryngology- Head & Neck Surgery 146 (7):630–638. https://doi.org/10.1001/jamaoto.2020.0674
- Ekberg, K., C. Grenness, and L. Hickson. 2014. “Addressing Patients’ Psychosocial Concerns Regarding Hearing Aids Within Audiology Appointments for Older Adults.” American Journal of Audiology 23 (3):337–350. https://doi.org/10.1044/2014_AJA-14-0011
- Entwistle, V., M. Prior, Z. C. Skea, and J. J. Francis. 2008. “Involvement in Treatment Decision-Making: Its Meaning to People with Diabetes and Implications for Conceptualisation.” Social Science & Medicine (1982) 66 (2):362–375. https://doi.org/10.1016/j.socscimed.2007.09.001
- Gallagher, N. E., and J. V. Woodside. 2018. “Factors Affecting Hearing Aid Adoption and Use: A Qualitative Study.” Journal of the American Academy of Audiology 29 (4):300–312. https://doi.org/10.3766/jaaa.16148
- Galvez, G., M. B. Turbin, E. J. Thielman, J. A. Istvan, J. A. Andrews, and J. A. Henry. 2012. “Feasibility of Ecological Momentary Assessment of Hearing Difficulties Encountered by Hearing Aid Users.” Ear and Hearing 33 (4):497–507. https://doi.org/10.1097/AUD.0b013e3182498c41
- Galvin, K., B. H. B. Timmer, D. Tomlin, and Z. Cleaver. 2022. “Designing a Hearing Health Care Smartphone App With Ecological Momentary Assessment: A Qualitative Study of Audiologists’ Perspectives.” American Journal of Audiology 31 (4):1247–1259. https://doi.org/10.1044/2022_AJA-22-00054
- Galvin, K., D. Tomlin, B. H. Timmer, Z. McNeice, N. Mount, K. Gray, and C. Short. 2023. “Designing a Mobile App to Assess Real-World Listening Difficulties: A Qualitative Study of Consumer Perspectives.” [Manuscript submitted for publication]. https://preprints.jmir.org/preprint/47578
- Glass, L. E., and H. H. Elliot. 1992. “The Professionals Told Me What it Was, But That’s Not Enough.” SHHH Journal 13 (1):26–28.
- Greasley, A., H. Crook, and R. Fulford. 2020. “Music Listening and Hearing Aids: Perspectives from Audiologists and their Patients.” International Journal of Audiology 59 (9):694–706. https://doi.org/10.1080/14992027.2020.1762126
- Grenness, C., L. Hickson, A. Laplante-Lévesque, C. Meyer, and B. Davidson. 2015. “Communication Patterns in Audiologic Rehabilitation History-Taking.” Ear and Hearing 36 (2):191–204. https://doi.org/10.1097/AUD.0000000000000100
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014a. “Patient-Centred Audiological Rehabilitation: Perspectives of Older Adults Who Own Hearing Aids.” International Journal of Audiology 53 Suppl 1 (1):S68–S75. https://doi.org/10.3109/14992027.2013.866280
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014b. “Patient-Centred Care: A Review for Rehabilitative Audiologists.” International Journal of Audiology 53 Suppl 1Suppl (1):S60–S67. https://doi.org/10.3109/14992027.2013.847286
- Hallberg, L. R., and M. L. Barrenäs. 1995. “Coping With Noise-Induced Hearing Loss: Experiences from the Perspective of Middle-Aged Male Victims.” British Journal of Audiology 29 (4):219–230. https://doi.org/10.3109/03005369509086600
- Hartley, D., E. Rochtchina, P. Newall, M. Golding, and P. Mitchell. 2010. “Use of Hearing Aids and Assistive Listening Devices in an Older Australian Population.” Journal of the American Academy of Audiology 21 (10):642–653. https://doi.org/10.3766/jaaa.21.10.4
- Heffernan, E., N. S. Coulson, H. Henshaw, J. G. Barry, and M. A. Ferguson. 2016. “Understanding the Psychosocial Experiences of Adults with Mild-Moderate Hearing Loss: An Application of Leventhal’s Self-Regulatory Model.” International Journal of Audiology 55 Suppl 3 (Suppl 3):S3–S12. https://doi.org/10.3109/14992027.2015.1117663
- Heffernan, E., D. W. Maidment, J. G. Barry, and M. A. Ferguson. 2019. “Refinement and Validation of the Social Participation Restrictions Questionnaire: An Application of Rasch Analysis and Traditional Psychometric Analysis Techniques.” Ear and Hearing 40 (2):328–339. https://doi.org/10.1097/AUD.0000000000000618
- Holman, J. A., A. Drummond, S. E. Hughes, and G. Naylor. 2019. “Hearing Impairment and Daily-Life Fatigue: A Qualitative Study.” International Journal of Audiology 58 (7):408–416. https://doi.org/10.1080/14992027.2019.1597284
- Iezzoni, L. I., B. L. O’Day, M. Killeen, and H. Harker. 2004. “Communicating About Health Care: Observations from Persons Who Are Deaf or Hard of Hearing.” Annals of Internal Medicine 140 (5):356–362. https://doi.org/10.7326/0003-4819-140-5-200403020-00011
- John, A. B., B. M. Kreisman, and S. Pallett. 2012. “Validity of Hearing Impairment Calculation Methods for Prediction of Self-Reported Hearing Handicap.” Noise & Health 14 (56):13–20. https://doi.org/10.4103/1463-1741.93321
- Laplante-Lévesque, A., L. Dons Jensen, P. Dawes, and C. Nielsen. 2013. “Optimal Hearing Aid Use: Focus Groups with Hearing Aid Clients and Audiologists.” Ear and Hearing 34 (2):193–202. https://doi.org/10.1097/AUD.0b013e31826a8ecd
- Laplante-Lévesque, A., L. Hickson, and L. Worrall. 2010. “A Qualitative Study of Shared Decision Making in Rehabilitative Audiology.” Journal of the Academy of Rehabilitative Audiology 43:27–43.
- Lim, C., A. B. L. Berry, T. Hirsch, A. L. Hartzler, E. H. Wagner, E. Ludman, and J. D. Ralston. 2016. “It just seems outside my health”: How Patients with Chronic Conditions Perceive Communication Boundaries with Providers.” DIS ’16: Proceedings of the 2016 ACM Conference on Designing Interactive Systems, Brisbane, Australia, 4-8 June, 2016, 1172–1184. https://doi.org/10.1145/2901790.2901866
- Lucas, L., R. Katiri, and P. T. Kitterick. 2018. “The Psychological and Social Consequences of Single-Sided Deafness in Adulthood.” International Journal of Audiology 57 (1):21–30. https://doi.org/10.1080/14992027.2017.1398420
- Manchaiah, V., M. L. Bellon-Harn, A. L. Dockens, J. H. Azios, and W. E. Harn. 2019. “Communication Between Audiologist, Patient, and Patient’s Family Members During Initial Audiology Consultation and Rehabilitation Planning Sessions: A Descriptive Review.” Journal of the American Academy of Audiology 30 (9):810–819. https://doi.org/10.3766/jaaa.18032
- Meyer, C., C. Barr, A. Khan, and L. Hickson. 2017. “Audiologist-Patient Communication Profiles in Hearing Rehabilitation Appointments.” Patient Education and Counseling 100 (8):1490–1498. https://doi.org/10.1016/j.pec.2017.03.022
- Morata, T. C., C. L. Themann, R. F. Randolph, B. L. Verbsky, D. C. Byrne, and E. R. Reeves. 2005. “Working in Noise with a Hearing Loss: Perceptions from Workers, Supervisors, and Hearing Conservation Program Managers.” Ear and Hearing 26 (6):529–545. https://doi.org/10.1097/01.aud.0000188148.97046.b8
- Newman, C. W., G. A. Hug, G. P. Jacobson, and S. A. Sandridge. 1997. “Perceived Hearing Handicap of Patients with Unilateral or Mild Hearing Loss.” The Annals of Otology, Rhinology, and Laryngology 106 (3):210–214. https://doi.org/10.1177/000348949710600305
- Parmar, B., K. Mehta, D. Vickers, and J. K. Bizley. 2022. “Experienced Hearing Aid Users’ Perspectives of Assessment and Communication Within Audiology: A Qualitative Study Using Digital Methods.” International Journal of Audiology 61 (11):956–964. https://doi.org/10.1101/2021.09.08.21263074
- Peters, M. D. J., C. Marnie, A. C. Tricco, D. Pollock, Z. Munn, L. Alexander, P. McInerney, C. M. Godfrey, and H. Khalil. 2020. “Updated Methodological Guidance for the Conduct of Scoping Reviews.” JBI Evidence Synthesis 18 (10):2119–2126. https://doi.org/10.11124/JBIES-20-00167
- Pike, A., S. Moodie, K. Parsons, A. Griffin, J. Smith-Young, T. ‑L. Young, L. Mills, M. Barrett, L. Rowe, M. Parsons, et al. 2022. “‘Something is Just Not Right with My Hearing’: Early Experiences of Adults Living with Hearing Loss.” International Journal of Audiology 61 (9):787–797. https://doi.org/10.1080/14992027.2021.1983656
- Poost-Foroosh, L., M. B. Jennings, L. Shaw, C. N. Meston, and M. F. Cheesman. 2011. “Factors in Client-Clinician Interaction that Influence Hearing Aid Adoption.” Trends in Amplification 15 (3):127–139. https://doi.org/10.1177/1084713811430217l
- Pryce, H. 2003. “Emotional Responses to King‐Kopetzky Syndrome: A Qualitative Study.” Audiological Medicine 1 (4):247–254. https://doi.org/10.1080/16513860310022381
- Shiffman, S., and A. A. Stone. 1998. “Introduction to the Special Section: Ecological Momentary Assessment in Health Psychology.” Health Psychology 17 (1):3–5. https://doi.org/10.1037/h0092706
- Skøt, L., T. Jeppesen, A. I. Mellentin, and A. Elklit. 2017. “Accessibility of Medical and Psychosocial Services Following Disasters and Other Traumatic Events: Experiences of Deaf and Hard-of-Hearing Individuals in Denmark.” Disability and Rehabilitation 39 (24):2468–2476. https://doi.org/10.1080/09638288.2016.1236154
- Thomas, J., and A. Harden. 2008. “Methods for the Thematic Synthesis of Qualitative Research in Systematic Reviews.” BMC Medical Research Methodology 8 (45):45. https://doi.org/10.1186/1471-2288-8-45
- Timmer, B. H. B., L. Hickson, and S. Launer. 2017. “Ecological Momentary Assessment: Feasibility, Construct Validity, and Future Applications.” American Journal of Audiology 26 (3S):436–442. https://doi.org/10.1044/2017_AJA-16-0126
- Tye-Murray, N., J. L. Spry, and E. Mauzé. 2009. “Professionals with Hearing Loss: Maintaining that Competitive Edge.” Ear and Hearing 30 (4):475–484. https://doi.org/10.1097/AUD.0b013e3181a61f16
- Vaisberg, J. M., A. T. Martindale, P. Folkeard, and C. Benedict. 2019. “A Qualitative Study of the Effects of Hearing Loss and Hearing Aid Use on Music Perception in Performing Musicians.” Journal of the American Academy of Audiology 30 (10):856–870. https://doi.org/10.3766/jaaa.17019
- Vas, V., M. A. Akeroyd, and D. A. Hall. 2017. “A Data-Driven Synthesis of Research Evidence for Domains of Hearing Loss, as Reported by Adults with Hearing Loss and their Communication Partners.” Trends in Hearing 21:2331216517734088. https://doi.org/10.1177/2331216517734088
- Weinstein, B. E. 1996. “Treatment Efficacy: Hearing Aids in the Management of Hearing Loss in Adults.” Journal of Speech, Language, and Hearing Research 39 (5):S37–S45. https://doi.org/10.1044/jshr.3905.s37