Abstract
Reduced physical activity (PA) is an independent risk factor for lung function decline, hospitalization and mortality in chronic obstructive pulmonary disease (COPD) and affects a large proportion of patients from Europe and the United States. However, little is known of the level of PA of COPD patients in Latin America. The aim of this study was to provide information of the level of PA and its determinants in COPD patients in Latin America. This is an observational, cross-sectional study on patients with COPD in seven Latin American countries. PA level was evaluated with the short version of the International Physical Activity Questionnaire (IPAQ) and the association between PA and other variables was investigated. Complete information of PA level was obtained in 734 COPD patients consecutively recruited from specialized outpatient clinics; 448 (61%) were men, with a mean age of 69.6 years (standard deviation [SD] = 8.7) and a mean FEV1 (% predicted) = 49.1% (17.5%). In 37.9% the level of PA was low, and the average sitting time was 36.1 h per week. Patients with low levels of PA were older, with higher levels of dyspnea and higher CAT scores. Additionally, we found that patients with low level of PA presented more symptoms during the day. Low levels of PA have been observed in a large proportion of COPD patients of Latin America, which is higher in women and older patients and it is related with worse functional and clinical characteristics.
Keywords:
Introduction
Physical activity (PA) is defined as any bodily movement produced by skeletal muscles that results in an energy expenditure, and it is a clinical parameter of increasingly relevance for many chronic conditions [Citation1]. Specifically, in chronic obstructive pulmonary disease (COPD) a reduction in the level of PA is an independent risk factor for accelerated lung function decline, hospitalization and mortality [Citation2–4].
Two of the main symptoms in COPD are a progressive exertional dyspnea and a gradual intolerance to exercise, leading to inactivity and disability as a natural progression of the disease [Citation5]. Furthermore, inactivity by itself induces a higher physical deterioration creating a vicious circle that leads to isolation and increased mortality [Citation2].
A high prevalence of physical inactivity in COPD patients from Europe and United States of America has been described, and this inactivity is more prevalent in COPD than in other chronic conditions such as diabetes mellitus or rheumatoid arthritis [Citation1,Citation6–8]. Additionally, there is evidence showing that physical inactivity affects COPD patients from earlier stages of the disease [Citation9].
Currently, little is known about the level of PA in Latin American patients with COPD [Citation10]. Therefore, it is relevant to have information regarding the PA level in COPD patients in this area and its determinants in order to design effective interventions with the aim to increase the PA level of COPD patients. In this context, we have analyzed the data collected in a large multicenter, international study conducted in Latin America with the objective to determine the level of PA of COPD patients and the determinant factors associated with low levels of PA.
Methods
The Latin American Study of 24-hour SYmptoms in Chronic Obstructive Pulmonary Disease (LASSYC) was an observational, multicenter, multinational, cross-sectional, non-interventional study (Clinical Trial Number NCT02789540) which primary objective was to describe the prevalence, severity and characteristics of respiratory symptoms in COPD patients from seven Latin American countries: Argentina, Chile, Colombia, Costa Rica, Guatemala, Mexico, and Uruguay [Citation11, Citation12]. In the current manuscript we present the results of an analysis of the PA and its determinants in the whole population.
The protocol of the study has been previously described in detail [Citation11]. Inclusion criteria were male and female outpatients, aged from 40 years old, diagnosed of COPD at least for 1 year, at least one spirometry with a COPD diagnosis using the post-bronchodilator forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) <0.70 criteria in the previous 12 months and current or ex-smokers (10 pack-years). Patients were classified according to the GOLD 2013 spirometric stages I to IV and groups A to D [Citation13]. Exclusion criteria were diagnosis of sleep apnea or any other chronic respiratory disease and any acute or chronic condition that would limit the patient’s ability to participate in the study.
Patients were consecutively recruited from specialized outpatient clinics and there was only one scheduled study visit in stable state which selected patients were asked to provide data on disease-related symptomatology assessed during a 24-hour day, health-related quality of life (HRQoL) and PA. The following data were collected: social demographics, health insurance system, lifestyle, smoking history, comorbidities, level of dyspnea, disease severity, prescribed COPD treatments, exacerbation history and healthcare resource utilization during the last 12 months. The study was performed in line with the Declaration of Helsinki and was approved by board and local ethics committee of all participating centers and all patients provided written informed consent.
PA level was evaluated with the short version of the International Physical Activity Questionnaire (IPAQ) which consists in 4 generics items for self-administered use [Citation14]. IPAQ short version was designed primarily for adults (range of 15-69 years) and there are validated versions available in more than 10 languages [Citation15]. The IPAQ short form asks about three specific types of activity (walking, moderate-intensity activities and vigorous-intensity activities). It provides separate scores for time (minutes) and frequency (days) in each type of activity, also includes a sitting question as an additional indicator of sedentarism. The IPAQ short form identifies the total minutes over the last seven days spent in each type of PA, responses are converted to metabolic equivalent task (MET) according to the IPAQ scoring protocol (8.0 MET for each minute of vigorous activity, 4 MET for each minute of moderate activity and 3.3 MET for each minute of walking). Afterwards, a sum of MET is obtained, allowing to categorize subjects in: High level of PA for subjects spending in one week at least 1500 MET in vigorous activities or who spend 3000 MET in a week of moderate plus vigorous PA; moderate level of PA applies for each of the following 3 criteria: 3 or more days of vigorous activity of at least 20 min per day, 5 or more days of moderate-intensity activity and/or walking of at least 30 min per day, 5 or more days of any combination of walking, moderate-intensity or vigorous-intensity activities achieving a minimum of at least 600 MET at week; finally, low level of PA is for activity under moderate level of PA [Citation15].
Level of dyspnea was quantified with the modified Medical Research Council (mMRC) dyspnea scale [Citation16]. As a measure of COPD prognosis, we used the Body Mass Index (BMI), Airflow Obstruction, Dyspnea and Exacerbations (BODEx) index, HRQoL was evaluated with the COPD Assessment Test (CAT) questionnaire and comorbidity was evaluated with the COPD comorbidity index (COPD specific comorbidity test [COTE]) [Citation17–19].
The Evaluating Respiratory Symptoms (E-RS) in COPD questionnaire was used to evaluate daytime symptoms (E-RS™: COPD; formerly EXAcerbations of Chronic pulmonary disease Tool [EXACT™] – Respiratory Symptoms) [Citation20]. The EXACT and E-RS are owned by Evidera, permission to use these instruments was obtained from Evidera [[email protected]].
Morning symptoms were assessed with the Early Morning Symptoms of COPD Instrument (EMSCI), which assesses symptoms that occur during the time from when patients get out of bed to start their daily living activities through the moment that they are ready for activities of the day at study visit [Citation21]. The nighttime symptoms were assessed with the Nighttime Symptoms of COPD Instrument (NiSCI). The NiSCI assesses symptoms that occur from the time from when patients go to bed the previous night until they wake up and get out of bed to start their daily living activities of the day of study visit [Citation22].
Statistical analysis
Descriptive statistics included the absolute and relative frequencies for categorical variables and mean and standard deviation (SD) for numerical ones.
In order to test associations of the level of PA with other characteristics we classified patients into tertiles, according with their level of PA. We also tested association between sitting time and other variables using two different methods: Firstly, we divided the population into tertiles according to sitting time with the highest tertile (more time sitting a day) as the reference; secondly, patients who spent 6 or more hours a day sitting were compared with the remaining patients. To analyze the relationship between PA and sitting time with symptoms at different times during the 24-hours day we classified patients in a dichotomic way, as daytime, early morning and nighttime symptomatic versus not symptomatic as in the previous publication [Citation11].
Analyses are presented as unadjusted and adjusted analysis by age, BMI, smoking status, COTE index, mMRC scale, FEV1% predicted, CAT score, BODEx index and number of ambulatory exacerbations. For these analyses, we dichotomize the PA tertiles in low and moderate/high levels, being the last category used as the reference one. The adjusted analysis was performed through a stepwise model, with only variables with p-values <0.2 included in the model, and those with a p-value lower than 5% were considered as statistically significant and were kept in the model. Collinearity and multicollinearity were evaluated. For collinearity between variables, we conducted a Pearson correlation and consider a value below −0.85 and higher than 0.85 as suggestive of the presence of collinearity. In the adjusted analysis, we evaluated the variance inflation factor and consider a mean value of 8.0 suggestive of the presence of multicollinearity in the model. As there is a well-known difference of PA levels by sex, we opted to stratify the analysis. All analyses were performed using Stata 13.1 (StatCorp LP, 2013. Stata Statistical Software: Release 13, College Station. TX. USA).
Results
A total of 795 patients were included, among them 734 (92.3%) COPD patients had complete information of PA level and they constitute the population of the current study. Of them, 448 (61%) were men, with a mean age of 69.6 years (SD = 8.7) and a mean FEV1 (% predicted) = 49.1% (17.5%) ().
Table 1. Patient’s characteristics according with the level of physical activity.
Levels of physical activity and associated factors
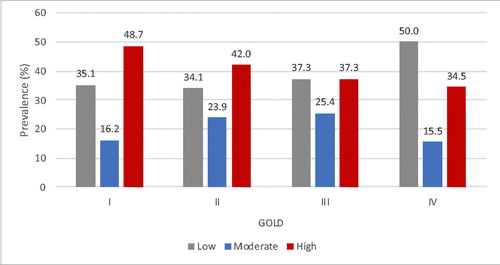
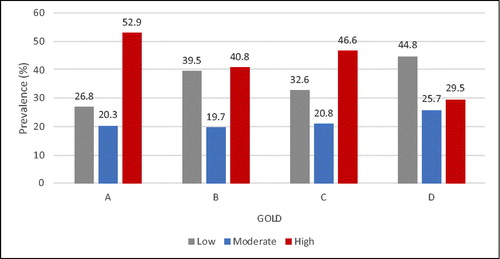
The levels of PA according to the scores of the IPAQ questionnaire are shown in . Patients reporting low level of PA included a higher proportion of women, were older, had lower FEV1 (%) and FEV1/FVC, were more symptomatic (higher score of mMRC scale and CAT), reported higher frequency of ambulatory exacerbations, presented a higher score of BODEx and higher frequency of symptoms during the day (global ERS score and specifically the breathlessness domain) (). In a multilevel model, being level 1 the country and level 2 the individuals, we found that intraclass correlation was lower than 6% indicating there is no role of the country on the proposed results (data not shown). In an adjusted analysis, for the whole population, low levels of PA (third tertile of the IPAQ questionnaire scores) were significantly associated with older age, higher levels of dyspnea and higher CAT scores, with small differences between both sexes. In females the significant association was observed with age and mMRC and in males with mMRC and CAT scores (). No evidence of collinearity or multicollinearity in the models was found.
Figure 1. Distribution of patients according with the level of physical activity.
High: Percentage with high physical activity, Moderate: Percentage with moderate physical activity, Low: percentage with low physical activity.
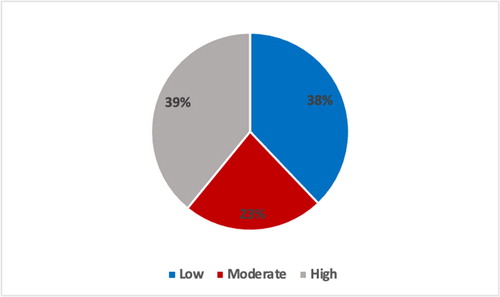
Table 2. Unadjusted and adjusted association between patients’ characteristics with low levels of physical activity. (lower tertile).
The distribution of levels of PA according to the GOLD severity stages I to IV or GOLD groups A to D are shown in and .
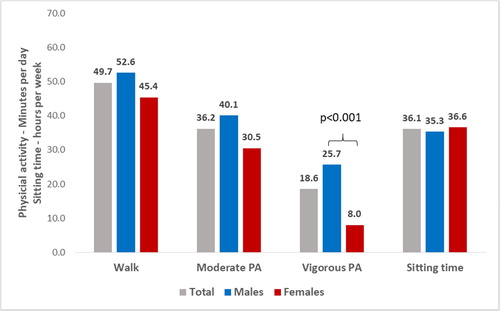
Time spent in different types of physical activity
Patients spent a mean of 49.7 min per day walking, 36.2 min doing moderate and 18.6 min doing vigorous PA, while mean sitting time was 36.1 h per week (5.1 h per day). A significant difference between sexes was observed in vigorous PA, with men being more active than women (mean of 25.7 versus 8.0 min per day, p < 0.001, ).
Association of symptoms during early morning, daytime and nighttime with levels of physical activity
The analysis of association between respiratory symptoms during the whole day and low level of PA only showed a significant association of daytime symptoms and low levels of PA in men in unadjusted analysis (OR= 1.61; 95% CI= 1.02 to 2.53; p = 0.041), but no significant associations were observed in the adjusted analysis (). No evidence of collinearity or multicollinearity was found.
Table 3. Unadjusted and adjusted association between symptoms during early morning. night and daytime with low levels of physical activity. (lower tertile).
Association of symptoms during early morning, daytime and nighttime with sitting time
In the unadjusted analysis, the risk to spend 6 or more hours a day sitting was higher in patients who presented daytime symptoms (OR = 1.52, p = 0.015); however, this association disappeared after adjustment for age, BMI, smoking status, COTE index, mMRC scale, FEV1 (%), CAT score, BODEx index and number of ambulatory exacerbations in the previous year.
The relationship between sitting time using the higher tertile as reference and symptoms during early morning, daytime and nighttime was also not significant neither consistent.
Discussion
Our results showed that near 40% of patients with COPD in Latin America presented low levels of PA and spent approximately 36 h per week (more than 5 h a day) sitting. Patients with low levels of PA were older, presented worse lung function, were more symptomatic, presented more frequency of exacerbations and were more frequently women. Additionally, we found that patients with low level of PA presented more symptoms during the day; however, patients with low level of PA or who spend more time sitting did not present any particular pattern of symptoms during the day (early morning, nighttime or during day symptoms).
Low levels of PA in COPD have been previously demonstrated in patients mainly from United States and Europe [Citation1,Citation6–8,Citation23]. Moreover, it has been clearly demonstrated that low levels of PA have an impact on mortality, exacerbations requiring hospitalization, and HRQoL [Citation1–4]. To the best of our knowledge, the current study is the first to characterize the level of PA in different patients with COPD in Latin America; it included patients from seven countries and allowed us to analyze relationships between levels of PA and other variables such as respiratory symptoms and HRQoL.
Patients with COPD present reduced levels of PA irrespective of the method for measurement used, although the proportion of inactive patients may vary between questionnaires and objective measurements [Citation24]. Studies using questionnaires have shown similar results to ours; for example, Garcia-Aymerich et al. [Citation2] reported that 21% of COPD patients had low or very low levels of PA, and Parada et al. [Citation10] using the IPAQ questionnaire, described that 38% of 112 COPD patients presented low levels of PA, almost identical to the 37.9% observed in our population. However, studies using objective methods, such as accelerometers, have found a higher proportion of patients with low level of PA compared with our results, for instance, Pitta et al. [Citation25] using an activity monitor, reported that COPD patients spend only 44 min per day walking. It has been well documented that questionnaires may be affected by recall bias, with a tendency to report higher levels than those observed using objective measurements [Citation24].
Several studies observed that the clinical characteristics of COPD are only weakly related to levels of PA and do not completely explain the level of PA [Citation1, Citation6, Citation10], the most frequently identified factors associated with reduced PA were older age, increased dyspnea, poor HRQoL, depression and more impaired lung function [Citation1, Citation6, Citation8, Citation10]. We have extended these results by identifying other factors significantly associated with low levels of PA in our population of Latin American patients with COPD; among them, the female sex, the higher frequency of exacerbations in the previous year and, in particular, the higher frequency and intensity of respiratory symptoms measured by the CAT questionnaire. These results suggest the presence of at least two possible vicious circles in patients with COPD [Citation26]: the first refers to the low levels of PA associated to depression and symptoms measured by the CAT scores. This relationship between depression and low PA may be bidirectional, inactive patients may be more depressed and depressed patients may be more inactive. In addition, depression influences the CAT scores [Citation27], and a worse CAT score may reflect both, increased symptoms and depression, both of them with a negative impact in PA [Citation1, Citation7]. On the other hand, the second vicious circle includes exacerbations and low PA; frequent and severe exacerbations may be a cause of low PA [Citation28], but also prospective studies suggest that exacerbations are more frequent in patients with low PA [Citation1]. These findings indicate that, in addition to direct strategies to increase PA levels, active screening and treatment of depression and effective treatments to prevent exacerbations may result in improvements of PA [Citation29]. Interestingly, low levels of PA were already observed in early or milder stages of COPD (GOLD I-II and GOLD A-B), which is consistent with previous studies [Citation9, Citation30].
Walking is by far the most frequent type of PA for patients with COPD. It is interesting to see how social, cultural, economic or climatic factors may influence the mean walking time of COPD patients in different countries [Citation31]. A Canadian study on patients with mainly mild COPD observed a mean walking time of only 3.9 h/week (33 min/day) [Citation3], which is significantly lower that the activity observed in patients from other countries with different socioeconomic and climatic conditions. In Spain, a study using objective measurements observed a mean of 86 min/day [Citation4]; however, a large study on +4,000 patients with moderate to severe COPD (mean FEV1 [%] 50% predicted) reported a mean self-declared walking of 66 min/day [Citation23], higher than the 49.7 min observed in our study and very similar to the 64 min observed in a recent study in Australia [Citation32]. Intensity of PA is also an important variable, and our patients spent a mean of 54.8 min a day on moderate to vigorous activity. These levels of activity are inferior to those observed in a recent study on 111 patients in Croatia who spent a mean of 87 min/day [Citation33], and to the 105 min/day on moderate or vigorous activity reported for a group of Spanish COPD patients, although they had milder airflow obstruction (FEV1 [%] of 56%) and lower level of symptoms compared with our population (mean CAT score of 12) [Citation4].
The reduced PA in Latin American COPD patients is even more pronounced in women. Both the time walking and the time in moderate and vigorous activities were significantly reduced in women compared to men. These differences are probably due to the socioeconomic and cultural characteristics of the area, where less women are professionally active and they are used to staying home caring for the households and the family members.
Sedentarism is a real health problem, in particular in COPD patients; a recent study reported up to a mean of 643 min per day of sedentary behavior in patients with COPD, which represents 71% of the waking time [Citation31]. However, our results suggest that COPD patients in Latin America spend less time sitting than in Europe: 309 min/day versus 374 min/day reported by Pitta et al. [Citation9] in COPD patients in Belgium, although this last study used an objective measurement of PA, which may account in part for the differences observed. In a systematic review, Hunt et al. [Citation34] reported a mean of 359 min/day of sitting time in COPD patients, but again, most of the patients were from European countries. Interestingly, Pitta et al. [Citation25] observed a significantly lower sitting time in Brazilian compared to Austrian COPD patients (296 versus 388 min/day). The lower sitting time in COPD patients from Latin America could be related to socioeconomics and cultural factors, for example in Latin America subjects use to having larger families and do more daily activities at home, such as cooking and cleaning, and there is less leisure time at home, being less frequent the “coach potato” behavior pattern than in Europe or the United States [Citation35].
We could not define a clear pattern of association between symptoms during different parts of the day and sedentary behavior. In the unadjusted analysis it appeared that patients presenting symptoms during daytime were more likely to spend more than 6 h a day sitting; however, this association was no longer significant in the adjusted analysis. Similarly, we could not identify any significant association between symptoms during different parts of the day and low levels of PA. Previous reports have suggested a relationship between morning symptoms and reduced PA in patients with COPD [Citation36, Citation37], but most of these studies did not consider symptoms in other parts of the day as well. Patients consecutively recruited from specialized outpatient clinics and therefore, results may not be extrapolated to milder patients attended in primary care. Patients with COPD associated to other exposures different from tobacco smoking were not included due to difficulties in standardizing the measurement of exposure across centers in different countries. The main limitation of our study is the use of a questionnaire to obtain information of PA instead of using an objective measure; however, we used a validated questionnaire that has demonstrated to be reliable for the quantification of PA in COPD patients. Another limitation is the cross-sectional design, which prevents any conclusion about causality. In contrast, the strength of the study is the large international sample of patients with different degrees of severity from seven Latin American countries.
Conclusions
In conclusion, the current study demonstrates for the first time that physical inactivity affects a big proportion of COPD patients in Latin America. Low levels of PA are particularly important in women and older patients and it is related with worse functional and clinical factors. Some strategies to incentive PA in Latin American COPD patients should be implemented, in particular strategies that have demonstrated their efficacy with a reduced cost, such as the use of pedometers or the urban circuits [Citation38–40].
Declaration of interest
Laura Mendoza has received speaker fees from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Grifols and Novartis and consulting fees from GlaxoSmithKline. Ana Menezes has been paid for her work as a statistician for the LASSYC study by AstraZeneca. Filip Surmont is an Employee of AstraZeneca. Marc Miravitlles has received speaker fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Menarini, Rovi, Bial, Zambon, CSL Behring, Grifols and Novartis and consulting fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Bial, Gebro Pharma, CSL Behring, Laboratorios Esteve, Ferrer, Mereo Biopharma, Verona Pharma, TEVA., pH Pharma. Novartis and Grifols and research grants from Grifols. The remaining authors have no conflicts of interest to disclosure.
Additional information
Funding
References
- Watz H, Waschki B, Meyer T, et al. Physical activity in patients with COPD. Eur Respir J. 2009;33:262–272. DOI:10.1183/09031936.00024608
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population-based cohort study. Thorax. 2006;61:772–778. DOI:10.1136/thx.2006.060145
- Dogra S, Good J, Buman MP, et al. Physical activity and sedentary time are related to clinically relevant health outcomes among adults with obstructive lung disease. BMC Pulm Med. 2018;18(1):98. DOI:10.1186/s12890-018-0659-8
- Arbillaga-Etxarri A, Gimeno-Santos E, Barberan-Garcia A, et al. Socio-environmental correlates of physical activity in patients with chronic obstructive pulmonary disease (COPD). Thorax. 2017;72(9):796–802. DOI:10.1136/thoraxjnl-2016-209209
- Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res. 2017;18:67. DOI:10.1186/s12931-017-0548-3
- Moy ML, Danilack VA, Weston NA, et al. Daily step counts in a US cohort with COPD. Respir Med. 2012;106:962–969. DOI:10.1016/j.rmed.2012.03.016
- Gimeno-Santos E, Frei A, Steurer-Stey C, et al. Determinants and outcomes of physical activity in patients with COPD: a systematic review. Thorax. 2014;69(8):731–739. DOI:10.1136/thoraxjnl-2013-204763
- Miravitlles M, Cantoni J, Naberan K. Factors associated with low level of physical activity in patients with chronic obstructive pulmonary disease. Lung. 2014;192(2):259–265. DOI:10.1007/s00408-014-9557-x
- Pitta F, Troosters T, Spruit MA, et al. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(9):972–977. DOI:10.1164/rccm.200407-855OC
- Parada A, Klaassen J, Lisboa C, et al. Reducción de la actividad física en pacientes con enfermedad pulmonar obstructiva crónica. Rev Med Chil. 2011;139:1562–1572.
- Miravitlles M, Menezes A, Lopez Varela MV, et al. Prevalence and impact of respiratory symptoms in a population of patients with COPD in Latin America: the LASSYC observational study. Respir Med. 2018;134:62–69. DOI:10.1016/j.rmed.2017.11.018
- Casas A, Montes de Oca M, Menezes AMB, et al. Respiratory medication used in COPD patients from seven Latin American countries: the LASSYC Study. Int J Chron Obstruct Pulm Dis. 2018;13:1545–1556. DOI:10.2147/COPD.S154097
- Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(4):347–365. DOI:10.1164/rccm.201204-0596PP
- Hallal PC, Victora CG. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med Sci Sports Exerc. 2004;36:556. DOI:10.1249/01.mss.0000117161.66394.07
- Lee PH, Macfarlane DJ, Lam TH, et al. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. DOI:10.1186/1479-5868-8-115
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–586. DOI:10.1136/thx.54.7.581
- Soler-Cataluña JJ, Martínez-García MA, Sánchez LS, et al. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med. 2009;103:692–699. DOI:10.1016/j.rmed.2008.12.005
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. DOI:10.1183/09031936.00102509
- Divo M, Cote C, de Torres JP, Casanova C, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. DOI:10.1164/rccm.201201-0034OC
- Leidy NK, Murray LT, Monz BU, et al. Measuring respiratory symptoms of COPD: performance of the EXACT-Respiratory Symptoms Tool (E-RS) in three clinical trials. Respir Res. 2014;15(1):124. DOI:10.1186/s12931-014-0124-z
- Eremenco S, Albuquerque P, Arnold BJ, et al. Translation and linguistic validation of two COPD symptom diaries (NiCSI and EMSCI) for use in 14 countries. Value Health. 2014;17:A600. DOI:10.1016/j.jval.2014.08.2079
- Hareendran A, Palsgrove AC, Mocarski M, et al. The development of a patient-reported outcome measure for assessing nighttime symptoms of chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2013;11:104. DOI:10.1186/1477-7525-11-104
- Ramon MA, Esquinas C, Barrecheguren M, et al. Self-reported daily walking time in COPD: relationship with relevant clinical and functional characteristics. Int J Chron Obstruct Pulm Dis. 2017;12:1173–1181. DOI:10.2147/COPD.S128234
- O’Neill B, McDonough SM, Wilson JJ, et al. Comparing accelerometer, pedometer and a questionnaire for measuring physical activity in bronchiectasis: a validity and feasibility study?Respir Res. 2017;18:16. DOI:10.1186/s12931-016-0497-2
- Pitta F, Breyer MK, Hernandes NA, et al. Comparison of daily physical activity between COPD patients from Central Europe and South America. Respir Med. 2009;103:421–426. DOI:10.1016/j.rmed.2008.09.019
- Ramon MA, Ter Riet G, Carsin AE, et al. The dyspnoea-inactivity vicious circle in COPD: development and external validation of a conceptual model. Eur Respir J. 2018;52(3):1800079. DOI:10.1183/13993003.00079-2018
- Miravitlles M, Molina J, Quintano JA, et al. Depressive status explains a significant amount of the variance in COPD assessment test (CAT) scores. COPD. 2018;13:823–831. DOI:10.2147/COPD.S154791
- Demeyer H, Costilla-Frias M, Louvaris Z, et al. Both moderate and severe exacerbations accelerate physical activity decline in COPD patients. Eur Respir J. 2018;51(1):1702110. DOI:10.1183/13993003.02110-2017
- Miravitlles M, Troosters T, Janssens W, et al. Multidisciplinary perspectives on the importance of physical activity in COPD. Arch Bronconeumol. 2019;55:551–552. DOI:10.1016/j.arbres.2019.03.010
- Decramer M, Rennard S, Troosters T, et al. COPD as a lung disease with systemic consequences–clinical impact, mechanisms, and potential for early intervention. Int J Chron Obstruct Pulm Dis. 2008;5:235–256. DOI:10.1080/15412550802237531
- Boutou AK, Raste Y, Demeyer H, et al. Progression of physical inactivity in COPD patients: the effect of time and climate conditions - a multicenter prospective cohort study. COPD. 2019;14:1979–1992. DOI:10.2147/COPD.S208826
- Cheng SWM, Alison JA, Stamatakis E, et al. Patterns and correlates of sedentary behaviour accumulation and physical activity in people with chronic obstructive pulmonary disease: a cross-sectional study. COPD. 2020;17(2):156–164. DOI:10.1080/15412555.2020.1740189
- Matkovic Z, Tudoric N, Cvetko D, et al. Easy to perform physical performance tests to identify COPD patients with low physical activity in clinical practice. Int J Chron Obstruct Pulm Dis. 2020;15:921–929. DOI:10.2147/COPD.S246571
- Hunt T, Madigan S, Williams MT, et al. Use of time in people with chronic obstructive pulmonary disease–a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:1377–1388.
- Tekerlek H, Cakmak A, Calik-Kutukcu E, et al. Exercise capacity and activities of daily living are related in patients with chronic obstructive pulmonary disease. Arch Bronconeumol. 2020;56:208–213. DOI:10.1016/j.arbres.2019.06.015
- van Buul AR, Kasteleyn MJ, Chavannes NH, et al. Association between morning symptoms and physical activity in COPD: a systematic review. Eur Respir Rev. 2017;26(143):160033. DOI:10.1183/16000617.0033-2016
- Nuñez A, Esquinas C, Barrecheguren M, et al. Evaluating the impact of morning symptoms in chronic obstructive pulmonary disease (COPD) using the Capacity of Daily Living during the Morning questionnaire (CDLM). Int J Chron Obstruct Pulm Dis. 2018;13:3837–3844. DOI:10.2147/COPD.S179402
- Mendoza L, Horta P, Espinoza J, et al. Pedometers to enhance physical activity in COPD: a randomised controlled trial. Eur Respir J. 2015;45(2):347–354. DOI:10.1183/09031936.00084514
- Pleguezuelos E, Pérez ME, Guirao L, et al. Improving physical activity in patients with COPD with urban walking circuits. Respir Med. 2013;107(12):1948–1956. DOI:10.1016/j.rmed.2013.07.008
- Arbillaga-Etxarri A, Gimeno-Santos E, Barberan-Garcia A, et al. Long-term efficacy and effectiveness of a behavioural and community-based exercise intervention (Urban Training) to increase physical activity in patients with COPD: a randomised controlled trial. Eur Respir J. 2018;52(4):1800063. DOI:10.1183/13993003.00063-2018