Abstract
We report a poisoning death from inhalational exposure to the gas fumigants chloropicrin and sulfuryl fluoride. The patient displayed both local irritant effects of chloropicrin and systemic effects of sulfuryl fluoride. The clinical course, marked by initial hypocalcemia, delayed onset of ventricular dysrhythmias, and death, is consistent with fluoride being the predominant mechanism of toxicity with sulfuryl fluoride.
Keywords:
Introduction
Sulfuryl fluoride (SO2F2), manufactured under the trade name Vikane®, is a colorless, odorless gas used extensively as a structural fumigant against wood-boring insects (Citation1,Citation2). Strict practice patterns exist for use of this agent, including pre-instillation of the warning agent chloropicrin, and allowing re-entry only after measurement of acceptable sulfuryl fluoride levels (Citation2–4). Despite rigorous safety measures, significant intentional and inadvertent exposures have occasionally been described, often resulting in death (Citation1,Citation3,Citation4).
Systemic effects of fluoride ions have been the proposed mechanism responsible for many of the clinical manifestations of sulfuryl fluoride toxicity (Citation2). Such effects, well described in non-inhalational exposures to other fluoride-containing compounds, include characteristic electrolyte abnormalities (hypocalcemia, hypomagnesemia, and hyperkalemia), delayed dysrhythmias, and death (Citation5). Animal models of sulfuryl fluoride poisoning have supported this by demonstrating the metabolism of inhaled sulfuryl fluoride Citation6),and detailing the clinical course of toxicity (Citation2). The published human case reports also support this mechanism by providing a variable degree of information on a total of seven patients exposed to sulfuryl fluoride (Citation1,Citation3,Citation4,Citation7). Most revealing are three of these reports in which delayed dysrhythmias and death are described (Citation3,Citation4). However, detailed descriptions of the clinical course, including electrolytes are lacking. In the following unfortunate case, we provide a detailed progression of the clinical course of severe sulfuryl fluoride poisoning. We also provide a discussion of potential treatment options and summarizing reported cases.
Table 1. Summary of sulfuryl fluoride cases
Case report
A thirty-seven-year-old woman with a history of depression and methamphetamine abuse was brought into the Emergency Department (ED) immediately after attempting to crawl out from underneath a tarpaulin used to enclose an apartment complex being fumigated with chloropicrin and sulfuryl fluoride. A fumigation employee helped pull the patient out from the tent and activated emergency medical services (EMS). Why the patient remained in the area of fumigation even after pre-instillation of chloropicrin remains disputed. It appears that she received approximately three hours of exposure to the fumigation. Paramedics arrived to find the patient with labored breathing and complaining of abdominal pain. She refused intravenous (IV) access and oxygen administration. Initial vital signs were blood pressure124/80 mmHg, pulse 80 beats per/minute, and respirations 20 per/minute. Paramedics noted a normal sinus rhythm on the cardiac monitor and a pulse oximeter reading of 98% on room air. During transport, the patient was noted to be agitated and confused, and had a single episode of vomiting.
Upon arrival to the ED vital signs were the following: blood pressure 74/48 mmHg, pulse 104/minute, and temperature 97.6° F (36.4°C). The patient was disoriented and was slightly agitated, but was able to describe abdominal pain, a burning sensation in the eyes, nausea, and shortness of breath. Physical examination was remarkable for bilateral scleral injection, lacrimation, normal sized and reactive pupils, patent nares and oropharynx without edema or erythema, clear lung sounds bilaterally, and a normal abdominal examination. Her skin was without diaphoresis or rashes, and her strength was normal.
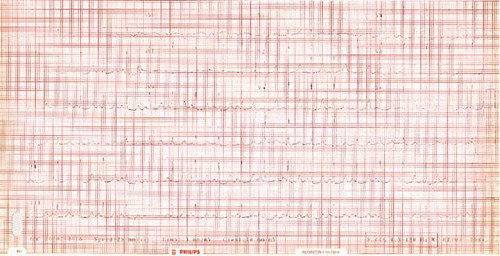
A peripheral IV was established, normal saline was administered for hypotension, 10 milligrams of metoclopramide was administered for nausea, and saline irrigation of her eyes was performed bilaterally. An electrocardiogram (ECG), done prior to metoclopramide administration, revealed sinus tachycardia, normal QRS width, slight ST-segment depression in the infero-lateral leads and a slightly prolonged QT interval (QTc 492 milliseconds) (). A chest radiograph performed soon after arrival was normal. A room air arterial blood gas, also performed soon after arrival revealed a pH of 7.45, pCO2 21 mm Hg, P02 104 mm Hg, and carboxyhemoglobin of 1.8%. Initial chemistry tests revealed: sodium, 146 mEq /L; potassium, 4.8 mEq/L; chloride, 108 mEq/L; bicarbonate, 20 mEq/L; BUN, 12 mg/dL; creatinine, 1.3 mg/dL; glucose 164 mg/dL and calcium, 5.3 mg/dL (reference 8.4 to 10.3 mg/dL). An AST, creatinine kinase, INR/PTT, lipase, and total bilirubin were all normal, and a pregnancy test was negative. A complete blood count was normal except for a slight leukopenia of 3,000/mm3. Ethanol was not detected in the serum, and a rapid urine drugs of abuse panel was positive only for amphetamines as a class. Blood testing for albumin, ionized calcium, and magnesium was unfortunately never performed.
Based on an initial discussion with a poison control center the emergency physician administered one gram of calcium gluconate IV empirically. Despite 3 liters of IV normal saline the systolic blood pressure remained between 70 to 80 mm Hg. Approximately two hours after arrival to the ED the patient deteriorated and was noted to have stool incontinence, to be foaming at the mouth, to have seizure-like activity that was interpreted by some observers as tetany, and was soon noted to be pulseless with an initial cardiac rhythm interpreted as torsade de pointes. Hypoxia was never documented on pulse oximeter prior to cardiac arrest. Cardiopulmonary resuscitation, central IV access, and tracheal intubation were all done quickly in conjunction with IV administration of more calcium, along with epinephrine and magnesium. Over the next thirty minutes the patient had various cardiac rhythms that were interpreted as torsade de pointes, ventricular fibrillation, and ultimately asystole. Approximately fifteen minutes into the resuscitation and after a total of six grams of calcium, a repeat chemistry was significant for a bicarbonate concentration of 12 mEq/L, a potassium concentration of 6.0 mEq/L, and a calcium concentration of 25.2 mg/dL. She was pronounced dead approximately three hours after EMS arrival at the scene. During her ED course she received IV doses totalling seven grams of calcium salts (two grams in the form of calcium gluconate and five grams in the form of calcium chloride), six grams of magnesium, two milligrams of epinephrine, two ampules of sodium bicarbonate, and one milligram of atropine.
An autopsy performed by the medical examiner was remarkable for acute tracheitis with pulmonary congestion and edema. There was no evidence of external or internal trauma. Antemortem toxicological blood testing excluded the presence of acetone, ephedrine, isopropanol, methanol, and pseudoephedrine. Both methamphetamine and amphetamine were detected in postmortem peripheral blood at concentrations of 0.71 mg/L and 0.36 mg/L, respectively. Additionally, atropine and metoclopramide were detected. Testing for fluoride revealed an antemortem blood concentration of 24 mg/L and a postmortem urine concentration of >100 mg/L. Chloropicrin was also detected in the urine. The cause of death was attributed to pesticide poisoning.
Discussion
The use of the fumigant sulfuryl fluoride requires pre-instillation of the lacrimating agent chloropicrin. As a result, case reports are confounded by the potential contribution of both agents (Citation1,Citation3,Citation4,Citation7). However, the effects of chloropicrin are predictable based on its local irritant properties, and isolated exposures are relatively well characterized (Citation8). The lacrimation, scleral injection, respiratory difficulty and delayed onset of pulmonary edema that occurred in our case were likely due to chloropicrin. Pulmonary congestion, however, has been described after isolated sulfuryl fluoride exposure (Citation3). Despite a description of the patient as “foaming at the mouth” just prior to cardiac arrest, the lack of coincident hypoxia suggests the “foam” may not have been entirely of pulmonary origin and that pulmonary edema was not the primary cause for deterioration. Therefore, although chloropicrin likely contributed to her presentation, it seems unlikely that it was predominantly responsible for her death, and does not explain many of the systemic manifestations that occurred.
The patient did manifest many systemic symptoms and signs previously described with sulfuryl fluoride poisoning including abdominal pain, confusion, convulsions, dysrhythmias, hypotension, incontinence, vomiting, and ultimately death (Citation1,Citation3,Citation4). She also manifested characteristic findings reported previously in systemic fluoride poisoning. The presence of initial hypocalcemia and subsequent refractory ventricular dysrhythmias and death is typical of what has been described in systemic fluoride poisoning from other agents (Citation5,Citation9–11). Hypomagnesemia is also common in systemic fluoride toxicity (Citation5) and although a magnesium concentration was not measured, the patient did manifest torsade de pointes, a ventricular dysrhythmia associated with hypomagnesemia, (Citation12) and previously reported in the setting of systemic fluoride poisoning (Citation9). It is possible that the administration of metoclopramide, an agent known to have adverse effects on the QT interval (Citation13) and which has been associated with torsade de pointes (Citation14), contributed as well. Delayed hyperkalemia is frequently found in significant systemic fluoride toxicity (Citation5,Citation10). In fact, hyperkalemia, refractory to standard therapy, is temporally more associated with ventricular dysrhythmias than hypocalcemia, in systemic fluoride poisoning (Citation10,Citation15). In our case, hyperkalemia did not appear to be predominantly responsible for the initial dysrhythmias. Despite significant metabolic acidosis (serum bicarbonate of 12 mEq/L) fifteen minutes after cardiac arrest, the potassium concentration was only 6.0 mEq/L. The absence of life threatening hyperkalemia, however, does not diminish the potential role of fluoride toxicity in our case, as ventricular fibrillation has been documented despite normal potassium and other electrolytes in systemic fluoride poisoning (Citation16). This has been suggested to occur from a direct myocardial effect of the fluoride ion (Citation16). The repeat calcium level of 25.2 mg/dL was obtained well after deterioration occurred and after a total of six grams of IV calcium. It was administered empirically and successively for persistent clinical deterioration. Although retrospectively the elevated level represents potentially harmful overaggressive calcium administration, it does highlight that calcium administration is not the panacea for systemic fluoride poisoning.
Testing for fluoride in our case revealed an antemortem blood concentration of 24 mg/L and a postmortem urine concentration of >100 mg/L. Two quantitative antemortem blood fluoride concentrations, and no urine concentrations, have been reported in the total of seven previously described patients with sulfuryl fluoride exposure (Citation1,Citation3,Citation4,Citation6). An antemortem blood concentration of 20 mg/L was reported in a fatal case with a very similar exposure, and clinical manifestations to the one presented here (Citation3). In the other case described, where the exposure was more prolonged, but to a presumably much lower concentration, the antemortem fluoride level was 0.5 mg/L one day prior to death (Citation4). A concentration of 50.42 mg/L was detailed in the only case in which a postmortem blood fluoride concentration was reported after sulfuryl fluoride exposure (Citation3). The patient we describe here had a known history of methamphetamine abuse and methamphetamine exposure was confirmed by testing. The postmortem levels of methamphetamine and amphetamine of 0.71 mg/L and 0.36 mg/L, respectively, confirm recent methamphetamine exposure. The postmortem methamphetamine level of 0.71 mg/L is within the typical range of those individuals who have been exposed recreationally to methamphetamine and who have died for a reason other than methamphetamine poisoning (Citation17). In our case methamphetamine intoxication may have contributed to the patient's poor decision to enter and remain in the fumigated structure, and may have contributed to her agitation. By diminishing coronary artery blood flow it may have also exacerbated the cardiac effects of the fluoride ion.
The optimal treatment strategy for sulfuryl fluoride poisoning is unclear. Prevention and immediate removal from exposure are obvious. Observation and supportive care for the local irritant effects from co-administered chloropicrin, and pulmonary edema from either agent is necessary after significant exposure. Health care providers should recognize that there is a risk of rapid deterioration with systemic fluoride poisoning. It appears prudent to avoid agents such as metoclopramide that can have adverse effects on the QT interval and which could precipitate torsades de pointes. Little research exists on treatment specific to sulfuryl fluoride poisoning. An animal study demonstrated survival improvement (but not convulsion protection) with calcium, but only when administered prior to exposure (Citation2). Phenobarbital and to a lesser extent diazepam were effective in decreasing convulsions and improving survival when administered either prior to, or after exposure (Citation2). Given the likelihood that the fluoride ion is the principal mechanism for toxicity with sulfuryl fluoride, information on therapies for other etiologies of systemic fluoride poisoning may be useful. Survival from severe systemic fluoride poisoning has been described with the administration of calcium and magnesium (Citation18,Citation19). However, electrolyte correction does not ensure protection from ventricular dysrhythmias (Citation18,Citation19). Delayed onset hyperkalemia may occur in systemic fluoride poisoning that may be refractory to standard treatments such as insulin and bicarbonate (Citation10). An in vitro model recently demonstrated that amiodarone, in addition to quinidine may attenuate fluoride-induced hyperkalemia, presumably by potassium channel blockade (Citation20). In another animal model of systemic fluoride poisoning quinidine administration was demonstrated to enhance survival (Citation11). Correcting systemic acidosis with bicarbonate may be beneficial. In an animal model bicarbonate pretreatment to create alkalosis improved outcome and renal clearance of fluoride (Citation21). Hemodialysis has been used with apparent success in a severe case of systemic fluoride poisoning with hydrofluoric acid (Citation18), and has been suggested to be initiated promptly to remove both potassium and fluoride (Citation10).
In summary, we present a fatal case of sulfuryl poisoning. The predominant mechanism proposed for sulfuryl fluoride poisoning is the in vivo release of fluoride ions (Citation2,Citation3,Citation5). The patient's course, marked by hypocalcemia, delayed ventricular dysrhythmias, and death, strongly supports fluoride as being one of the principal mechanisms for toxicity.
References
- EP Taxay. Vikane inhalation. J Occup Med 1966; 8:425–6.
- KD Nitschke, RR Albee, JL Mattsson, and RR Miller. Incapacitation and treatment of rats exposed to a lethal dose of sulfuryl fluoride. Fundam Appl Toxicol 1986; 7:664–70.
- EH Scheuerman. Suicide by exposure to sulfuryl fluoride. J Forensic Sci 1986; 3:154–8.
- Centers for Disease Control (CDC). Fatalities resulting from sulfuryl fluoride exposure after home fumigation--Virginia. MMWR Morb Mortal Wkly Rep 1987; 36:602–4.609–11.
- EM Caravati. Acute hydrofluoric acid exposure. Am J Emerg Med 1988; 6:143–50.
- WJ Hayes. Mortality in 1969 from pesticides, including aerosols. Arch Environ Health 1976; 31:61–72.
- AL Mendrala, DA Markham, and DL Eisenbrandt. Rapid uptake, metabolism, and elimination of inhaled sulfuryl fluoride fumigant by rats. Toxicol Sci. 2005; 86:239–47.
- K Gonmori, H Muto, T Yamamoto, and K Takahashi. A case of homicidal intoxication by chloropicrin. Am J Forensic Med Pathol 1987; 8:135–8.
- AE Klasner, AJ Scalzo, C Blume, and P Johnson. Ammonium bifluoride causes another pediatric death. Ann Emerg Med 1998; 31:525.
- ME McIvor, CE Cummings, MM Mower, RE Wenk, JA Lustgarten, RF Baltazar, and J Salomon. Sudden cardiac death from acute fluoride intoxication: the role of potassium. Ann Emerg Med 1987; 16:777–81.
- CC Cummings, and ME McIvor. Fluoride-induced hyperkalemia: the role of Ca2+-dependent K+ channels. Am J Emerg Med. 1988; 6:1–3.
- SR Ramee, CJ White, JT Svinarich, TD Watson, and RF Fox. Torsade de pointes and magnesium deficiency. Am Heart J 1985; 109:164–7.
- E Ellidokuz, and D Kaya. The effect of metoclopramide on QT dynamicity: double-blind, placebo-controlled, cross-over study in healthy male volunteers. Aliment Pharmacol Ther 2003; 18:151–5.
- CC Chou, and D Wu. Torsade de pointes induced by metoclopramide in and elderly woman with preexisting complete left bundle branch block. Chang Gung Med J 2001; 24:805–9.
- RF Baltazar, MM Mower, R Reider, M Funk, and J Salomon. Acute fluoride poisoning leading to fatal hyperkalemia. Chest 1980; 78:660–2.
- V Bjornhagen, J Hojer, C Karlson-Stiber, AI Selden, and M Sundbom. Hydrofluoric acid-induced burns and life-threatening systemic poisoning--favorable outcome after hemodialysis. J Toxicol Clin Toxicol 2003; 41 (6):855–60.
- BK Logan, CL Fligner, and T Haddix. Cause and manner of death in fatalities involving methamphetamine. J Forensic Sci Jan, 1998; 43 (1):28–34.
- BM Bordelon, JR Saffle, and SE Morris. Systemic fluoride toxicity in a child with hydrofluoric acid burns: a case report. J Trauma 1993; 34:437–9.
- ES Stremski, GA Grande, and LJ Ling. Survival following hydrofluoric acid ingestion. Ann Emerg Med 1992; 21:1396–99.
- M Su, J Chu, MA Howland, LS Nelson, and RS Hoffman. Amiodarone attenuates fluoride-induced hyperkalemia in vitro. Acad Emerg Med 2003; 10:105–9.
- KE Reynolds, GM Whitford, and DH Pashley. Acute fluoride toxicity: the influence of acid-base status. Toxicol Appl Pharmacol 1978; 45:415–27.