Abstract
A Brugada electrocardiographic pattern (BEP) associated with tricyclic antidepressant (TCA) overdose has been reported rarely, but its reversal by sodium bicarbonate has not been described previously. We reported a case of amitriptyline overdose induced Type 1 BEP which was reversed by 150 mEq of intravenous sodium bicarbonate.
Introduction
Brugada syndrome (BS) is a genetic myocardial sodium channel dysfunction that results in slow inward current and ventricular dysrhythmias. It is a clinical and electrocardiogram (ECG) entity with features including sudden cardiac death, right bundle branch block (RBBB), and unusual ST-segment elevation in leads V1–V3. The responsiveness of Brugada electrocardiographic pattern (BEP) to sodium bicarbonate (NaHCO3) after a tricyclic antidepressant (TCA) overdose has not been described. We report a case of Type 1 BEP after an intentional amitriptyline overdose that responded to NaHCO3 treatment.
Case report
A 42-year-old man with a chief complaint of low back pain was brought by paramedics to our emergency department (ED). Apart from a history of chronic low back pain, his medical history included a diagnosis of somatoform disorder that was treated with amitriptyline. He was found fully alert, but during the transfer to ED, his level of consciousness decreased and he had a Glasgow Coma Scale score of 7/15 (E1V1M5) on arrival. His blood pressure was 134/75 mmHg, pulse rate 120 beats/min, respiratory rate 20 breaths/min, and SpO2 98%. He was afebrile and there were no focal neurological deficits or anti-cholinergic signs. His reflexes were not brisk. The patient vomited once and was subsequently intubated for airway protection using etomidate and succinylcholine. The pH of his arterial blood gas analysis was 7.40. His serum glucose (5.6 mmol/L, 101 mg/dL) and electrolytes (Na 143 mmol/L, K 3.5 mmol/L) were normal.
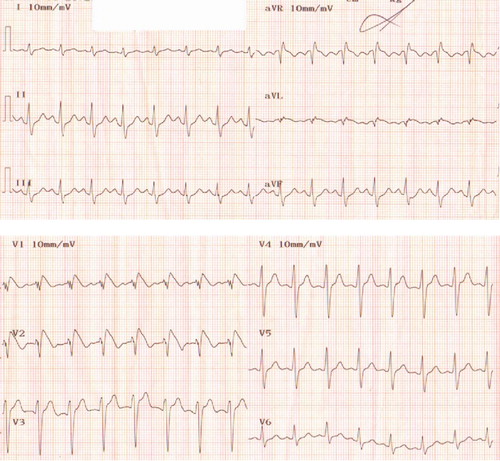
His first ECG () showed cove-shaped ST segment elevation over leads V1–V3 with RBBB and T-wave inversion, compatible with Type 1 BEP. A prominent terminal R wave was found in lead aVR. The QRS and QTc were 0.131 and 0.465 s, respectively.
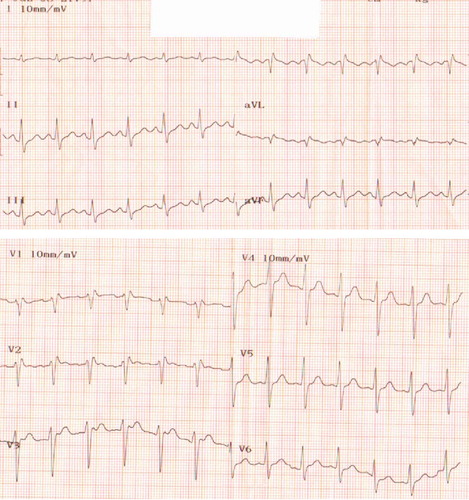
In view of the patient's ECG findings and his pharmacological history, an amitriptyline overdose was suspected. A total of 150 mEq NaHCO3 was given by three separate boluses. The venous pH after NaHCO3 treatment was 7.57. The ECG was repeated 5 min after the third bolus of NaHCO3 () and the cove-shaped ST elevation was gone. The QRS was 0.123 s. Further investigation revealed a normal brain computed tomography (CT).
The patient remained comatose and was admitted to the intensive care unit (ICU) for further management. Gastrointestinal decontamination using activated charcoals was attempted, but the orogastric tube could not be inserted. Serum acetaminophen and salicylate concentrations were undetectable. Serum troponin T was <0.03 μg/L. At this time, suicidal notes were discovered at patient's home.
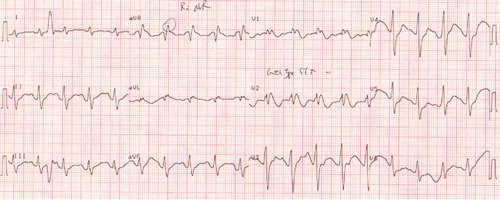
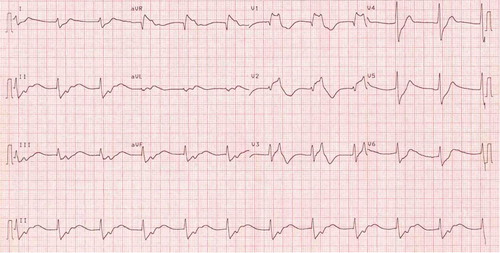
Fourteen hours after admission to the ICU, Type 1 BEP reappeared in the ECG and QRS was widened to 0.134 s (). The patient suddenly developed status epilepticus, which was controlled by propofol infusion. He was found to have hypotension with metabolic acidosis with an arterial pH of 6.99 after the convulsion. There was one episode of witnessed pulseless ventricular tachycardia (but no ECG record) that was responded to resuscitation. A total of 200 mEq NaHCO3 with fluid resuscitation was given. The arterial pH rose to 7.23 and his ECG () showed a junctional rhythm and persistent BEP with a QRS interval of 0.126 s. His condition continued to deteriorate even with maximal inotropic support, and he developed asystole 10 h afterwards. An ante-mortum serum amitriptyline concentration was 1.8 mcg/mL (reference 0.05–0.3 mcg/mL). No co-ingestants were detected and the coroner's report attributed the death to amitriptyline overdose.
Discussion
We have reported a psychiatric patient who was brought to the ED with rapid deterioration in conscious level. At the initial presentation, apart from reduced conscious level and ECG abnormities, our patient did not present any typical anticholinergic toxidrome, hypotension, or brisk jerks, which would be suggestive of TCA toxicity. BEP in our patient's ECG could be due to therapeutic dose (Citation1) or overdose of amitriptyline. However, later recurrence of BEP in ICU suggested that there was a continuous absorption of amitriptyline from the gut. The supra-therapeutic antemortem amitriptyline concentration confirmed that it was a case of amitriptyline overdose.
Several mutations on the cardiac sodium channel gene such as SCN5A (Citation2) have been reported. A reduction in the inward sodium current and a prominent outward current result in a shortened action potential in the right ventricular epicardial tissue. Spatial heterogeneity of action potential duration between the epicardium and the endocardium causes ST segment elevation in leads V1–V3.
Overdose of medications with type 1A antidysrhythmic effects, such as cocaine, anti-psychotic agents, and TCAs, have been reported to be associated with BEP (Citation3). However, BEP after TCA intentional ingestion is uncommon (less than 3% of patients developed BEP) (Citation4). Hypotension, widened QRS duration, and seizures were more commonly found in patients with BEP after TCA overdose. A case series of BEP after TCA overdose showed that there was no statistically significant increase in the risk of death from cardiac causes related to the development of BEP after TCA overdose (Citation5).
The mechanism of BEP after TCA overdose is not well known. One possibility is that TCA, like other sodium channel blockers, might block myocardial sodium channels in right ventricle causing BEP (Citation6). This could explain the efficacy of NaHCO3 on the TCA-induced BEP in our case. In our patient, BEP was initially reversed by intravenous NaHCO3 treatment. However, it is possible there was on-going absorption of amitriptyline from the gut. BEP with widening of the QRS reappeared in ICU and persisted after 200 mEq NaHCO3 administration. Further NaHCO3 should have been considered at that time because the end points of plasma alkalization (QRS <0.1 s or pH 7.50–7.55) had not been reached. BEP might have resolved if further NaHCO3 had been given.
In one case, BEP after a large amitriptyline overdose did not respond to NaHCO3 up to 350 mEq by intravenous bolus despite narrowing of the QRS complex (Citation7). The treatment of BEP that is unresponsive to NaHCO3 therapy is unclear. Although hypertonic saline has been used in the treatment of a TCA overdose (Citation8), there is no study or case report to evaluate the use of hypertonic saline on TCA overdose induced BEP.
Conclusion
BEP may be one of the many manifestations of TCA overdose, but the mechanism is still not clear. As demonstrated in this case report, amitriptyline-induced BEP may be reversed by intravenous NaHCO3.
References
- VC Babaliaros, and JW Hurst. Tricyclic antidepressants and the Brugada syndrome: an example of Brugada waves appearing after the administration of desipramine. Clin Cardiol 2002; 25:395–398.
- S Wataru. The Brugada syndrome – an update. Int Med 2005; 44 (12):1224.
- F Rouleau, P Asfar, S Boulet, L Dube, JM Dupuis, P Alquier, and J Victor. Transient ST segment elevation in right precordial leads induced by psychotropic drugs: relationship to the Brugada syndrome. J Cardiovasc Electrophysiol 2001; 12:61–65.
- VS Bebarta, S Phillips, A Eberhardt, KJ Callihan, K Heard, and J Waksman. Incidence and outcomes of patients with the Brugada pattern in a large case series of tricyclic overdoses. J Toxicol Clin Toxicol 2004; 42 (5):714.
- D Goldgran-Toledano, G Sideris, and JP Kevorkian. Overdose of cyclic antidepressants and the Brugada syndrome. N Engl J Med 2002; 346:1591–1592.
- JT Niemann, HA Bessen, RJ Rothstein, and MM Laks. Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol 1986; 57:1154–1159.
- VS Bebarta, JC Waksman, and M Minick. Brugaga pattern after large amitriptyline overdose not responsive to sodium bicarbonate. J Toxicol Clin Toxicol 2004; 42 (5):734.
- PE McKinney, and R Rasmussen. Reversal of severe tricyclic antidepressant-induced cardiotoxicity with intravenous hypertonic saline solution. Ann Emerg Med 2003; 42 (1):20–24.