1. Introduction
Heart failure (HF) is a life-threatening condition that affects millions of people worldwide and is associated with significant morbidity and mortality. The prevalence of HF is rising continually, and hospitalizations related to HF decompensation contribute significantly to increased healthcare expenditure and are associated with worse prognosis [Citation1]. Hypervolemia and increased intrathoracic fluid accumulation are believed to be the inciting factors of acute HF decompensation. Monitoring of fluid status would, at least theoretically, can detect early decompensation and lead to early treatment, thus preventing rehospitalizations. However, several challenges in early detection exist and classical physical signs [Citation2] as well as echocardiographic and radiographic indices [Citation3,Citation4] are of limited use in the early detection of fluid status. Over the past few decades, novel methods were introduced to assess volume status in HF patients, one of which is thoracic impedance monitoring. Our objective is to summarize the current knowledge on impedance monitoring as a strategy for early detection of HF exacerbations.
2. Basis of impedance measurement
Impedance is a measure of effective resistance exerted by the body to a low intensity alternating current. Thoracic tissue exerts higher resistance (200–5000 Ω.cm) to the current as compared to blood and fluids (65–150 Ω.cm). As a result, regions of the body with higher fluid content will result in lower impedance as compared to body regions with more solid tissue [Citation5]. This physical basis has been utilized to assess hemodynamics and changes in fluid accumulation in patients with HF. Impedance can be measured non-invasively using band electrode methods or using implanted devices. Since the placement of electrodes varies significantly between both methods, algorithms to measure impedance vary widely even among different devices.
3. Measurement of impedance
3.1. Band electrode methods
The band electrode method uses externally placed band electrodes between the neck and thorax before a high-frequency low-amplitude current (50–100 kHz, 1–4 mA) is applied between the first pair of contact while the second pair of contact measures the potential difference reflecting the thoracic impedance () [Citation6]. Silva Lopes et al. found impedance cardiography was an adequate method to detect differences in blood flow parameters, contractility, and left stroke work index in patients with and without HF [Citation7]. Thoracic impedance has been validated against the thermodilution method in a study by Faini et al. [Citation8].
The whole-body impedance method using two electrodes placed at the ankle and wrist has been validated against the Fick and thermodilution method to estimate cardiac output [Citation9]. A more recent study by Hassan-Tash et al. correlated stroke volume measured by impedance cardiography and magnetic resonance-derived measurements [Citation10]. The noninvasive methods using external electrodes can provide an assessment of relative cardiac output changes in response to therapy. Nevertheless, the use of this method is very limited and may not be practical as it requires the patient to be in a location for the test. Additionally, variable electrode placement sites would affect reproducibility and hence lead to confounding of the results.
3.2. Implanted device-based method
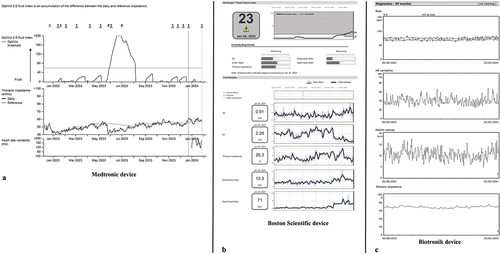
Implanted cardiac rhythm management devices including pacemakers, implantable cardioverter defibrillators (ICD) and cardiac resynchronization therapy devices (CRT-D) have become widely utilized in HF patients. Multiple advances in these devices added the capability of monitoring thoracic impedance to reflect pulmonary fluid status and predict HF decompensation [Citation11]. Different algorithms for impedance monitoring are used by different device manufacturers. OptiVol™ fluid trend by Medtronic tracks intrathoracic impedance changes over time. Impedance measurements are made at 20-min intervals using the right ventricle coil to the tip of the can passing through the tissue within the thoracic cavity. The average impedance value is calculated for that day and graphed showing daily trends (). The Fluid Accumulation Status Trial (FAST) followed 156 HF patients with ICD or CRT devices modified to record daily changes in intrathoracic impedance and compared them to weight gain [Citation12]. The study showed that impedance data was more sensitive than weight gain (76% vs. 23%, p < 0.0001). The Program to Access and Review Trending Information and Evaluate Correlation to Symptoms in Patients With HF (PARTNERS-HF) study was a prospective study of 694 patients over 12 months follow-up that prospectively evaluated the utility of impedance data to predict HF hospitalizations [Citation13]. Patients with a positive combined HF device diagnostics had a 5.5-fold increased risk of HF hospitalization with pulmonary signs or symptoms within the next month (hazard ratio: 5.5, 95% confidence interval: 3.4 to 8.8, p < 0.0001). HeartLogic™ index is used by Boston Scientific and combines multiple data points including accelerometer-based first and third heart sounds, thoracic impedance, respiration rate, relative tidal volume, heart rate, and patient activity (). Updated daily, an alert is generated when the index crosses a certain threshold. The MultiSENSE (Multisensor Chronic Evaluation in Ambulatory Heart Failure Patients) study included 900 patients that were followed for up to 1 year [Citation14]. The predictive sensitivity to HF exacerbation in this study was 70%, with a median early warning of 34 days before the event. The development of an alert management guide was implemented in The Multiple cArdiac seNsors for mAnaGEment of Heart Failure (MANAGE-HF) study which enrolled 200 patients with either an HF hospitalization within the preceding year, an unscheduled HF exacerbation visit within 90 days or elevated natriuretic peptide levels [Citation15]. HF treatment was intensified during 74% of the alert cases resulting in more rapid recovery of the HeartLogic Index. Another algorithm used by Biotronik (HeartInsight HF score) was validated in Selection of potential predictors of worsening heart failure (SELENE HF) study [Citation16]. The algorithm included thoracic impedance along with other variables such as heart rate, physical activity, atrial high-rate burden, and the number of premature ventricular complexes per hour (). The algorithm predicted HF hospitalizations with a sensitivity of 65.5% and 0.69 false alerts per patient years. Lastly, CorVue™ monitoring algorithm was developed by St. Jude Medical (currently Abbott) and applies combined vectors to estimate intrathoracic impedance. This multivector algorithm was subsequently evaluated in the Detect Fluid Early from Intrathoracic Impedance Monitoring (DEFEAT-PE) study [Citation17] and demonstrated a low sensitivity of 21.6% to predict HF events.
Figure 2. (a) Optivol index rising with decreasing thoracic impedance with return to baseline upon adjustment of HF medical therapy. 2(b): Heartlogic index rising with worsening impedance, S3 sounds, respiratory and nightly heart rate, indicating decompensation. 2(c): heart failure monitoring indices used by Biotronik devices including heart rate, variability, patient activity and thoracic impedance.
3.3. Implications of impedance monitoring
The impact of intrathoracic impedance monitoring on survival and HF hospitalizations was evaluated in a large cohort of 1,565 Medicare ICD registry patients [Citation18]. Over a median follow-up of greater than 6 years, patients who had more than 15.1% of follow-up days above OptiVol threshold had at least a 4-fold increased mortality rate and a 3-fold HF hospitalizations rate. On the contrast, lung impedance guided preemptive treatment of HF was found to reduce HF hospitalizations, cardiovascular and all-cause mortality in a randomized controlled study that included 256 patients with LVEF ≤ 35% and NYHA class II-IV [Citation19]. The mechanism of improved outcomes in the impedance-guided group was further explored in a post hoc analysis [Citation20]. The improved outcome was thought to be related to diuretic up-titration at the preclinical stage of lung congestion which led to better clinical outcome.
Recently published data from pooled analysis of 2,050 patients revealed that remote monitoring-based multi-parametric HeartInsight HF score was significantly higher at 12 weeks before hospitalization compared to those who were not hospitalized, and it further increased by 22% until hospitalization [Citation21]. Further analysis suggested that parameters such as 24-h heart rate (HR), HR variability, and thoracic impedance were already higher 12 weeks before hospitalization with 71% contribution to the HF score while nocturnal HR, atrial tachyarrhythmia, ventricular extrasystoles, and patient activity significantly changed closer to hospitalization with 31% contribution to the HF score. This further highlights the need to better fine tune our remote monitoring strategies to identify those at risk.
4. Limitations
Several limitations restrict the broad adoption of impedance technologies in HF management. First, many factors can affect impedance measurements. Electrode placement, skin moisture, body movement and composition can affect the signal’s fidelity [Citation22]. The flow of electrical current in the aorta can be affected by valvular regurgitation leading to variability in stroke volume readings [Citation23]. Fluid distribution can be altered by postural changes, causing variation in impedance over time [Citation24]. Second, there was a considerable number of false-positive alerts in device-based impedance algorithms which can lead to increased healthcare utilization. Fourth, there is a paucity of data regarding the effect of therapeutic interventions based on impedance data and the impact of utilizing this method on health care expenditures. Lastly, there is a lack of a universally adopted gold standard strategy for clinical monitoring and objective assessment of HF patients.
5. Conclusions
Impedance monitoring can be used to determine changes in hemodynamics and fluid overload which can be used as a strategy for early detection of HF exacerbation. However, the integration of such a strategy in HF care faces several challenges owing to undetermined clinical utility and a lack of meaningful outcome measures to justify its widespread adoption.
6. Expert opinion
HF hospitalization and mortality add a significant burden to healthcare. Therefore, device-based remote monitoring in HF patients presents a perfect opportunity to alleviate the risk of full decompensation before potential hospitalization is needed. Although multiparameter algorithms have shown better diagnostic accuracy over single sensor monitoring, inconsistency in prospective trials and studies have dampened the enthusiasm for application of the technology to routine patient care. In our judgment, careful selection of patients at high risk for acute decompensated HF, as well as standardized care protocols to adjust diuretics with monitoring may yield the best results.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Additional information
Funding
References
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American heart association. Circulation. 2021 Feb 23;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950
- Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989 Feb 10;261(6):884–888. doi: 10.1001/jama.1989.03420060100040
- Dokainish H, Zoghbi WA, Lakkis NM, et al. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004 May 25;109(20):2432–2439. doi: 10.1161/01.CIR.0000127882.58426.7A
- Mahdyoon H, Klein R, Eyler W, et al. Radiographic pulmonary congestion in end-stage congestive heart failure. Am J Cardiol. 1989 Mar 1;63(9):625–627. doi: 10.1016/0002-9149(89)90912-0
- Tang WH, Tong W. Measuring impedance in congestive heart failure: current options and clinical applications. Am Heart J. 2009 Mar;157(3):402–411. doi: 10.1016/j.ahj.2008.10.016
- Patterson RP. Fundamentals of impedance cardiography. IEEE Eng Med Biol Mag. 1989;8(1):35–38. doi: 10.1109/51.32403
- Silva Lopes B, Craveiro N, Firmino-Machado J, et al. Hemodynamic differences among hypertensive patients with and without heart failure using impedance cardiography. Ther Adv Cardiovasc Dis. 2019 Jan;13:1753944719876517. doi: 10.1177/1753944719876517
- Faini A, Omboni S, Tifrea M, et al. Cardiac index assessment: validation of a new non-invasive very low current thoracic bioimpedance device by thermodilution. Blood Press. 2014; Apr23:(2):102–108.
- Paredes OL, Shite J, Shinke T, et al. Impedance cardiography for cardiac output estimation: reliability of wrist-to-ankle electrode configuration. Circ J. 2006; Sep70:(9):1164–1168.
- Hassan-Tash P, Ismail U, Kirkpatrick IDC, et al. Correlation of impedance cardiography-derived and cardiac magnetic resonance-derived stroke volumes. Curr Probl Cardiol. 2023; Feb48:(2):101457.
- Small RS, Wickemeyer W, Germany R, et al. Changes in intrathoracic impedance are associated with subsequent risk of hospitalizations for acute decompensated heart failure: clinical utility of implanted device monitoring without a patient alert. J Card Fail. 2009; Aug15:(6):475–481.
- Abraham WT, Compton S, Haas G, et al. Intrathoracic impedance vs daily weight monitoring for predicting worsening heart failure events: results of the fluid accumulation status trial (FAST). Congest Heart Fail. 2011; Mar17:(2):51–55.
- Whellan DJ, Ousdigian KT, Al-Khatib SM, et al. Combined heart failure device diagnostics identify patients at higher risk of subsequent heart failure hospitalizations: results from PARTNERS HF (program to access and review trending information and evaluate correlation to symptoms in patients with heart failure) study. J Am Coll Cardiol. 2010 Apr 27;55(17):1803–1810. doi: 10.1016/j.jacc.2009.11.089
- Boehmer JP, Hariharan R, Devecchi FG, et al. A multisensor algorithm predicts heart failure events in patients with implanted devices: results from the MultiSense study. JACC Heart Fail. 2017; Mar5:(3):216–225.
- Hernandez AF, Albert NM, Allen LA, et al. Multiple cArdiac seNsors for mAnagement of heart failure (MANAGE-HF) - phase I evaluation of the integration and safety of the HeartLogic multisensor algorithm in patients with heart failure. J Card Fail. 2022; Aug28:(8):1245–1254.
- D’Onofrio A, Solimene F, Calo L, et al. Combining home monitoring temporal trends from implanted defibrillators and baseline patient risk profile to predict heart failure hospitalizations: results from the SELENE HF study. EP Europace. 2022 Feb 2;24(2):234–244. doi: 10.1093/europace/euab170
- Heist EK, Herre JM, Binkley PF, et al. Analysis of different device-based intrathoracic impedance vectors for detection of heart failure events (from the detect fluid early from intrathoracic impedance monitoring study). Am J Cardiol. 2014 Oct 15;114(8):1249–1256. doi: 10.1016/j.amjcard.2014.07.048
- Brown JR, Alonso A, Warman EN, et al. Long-term impact of intrathoracic impedance findings on survival and heart failure hospitalizations after cardiac resynchronization therapy in ICD registry patients. EP Europace. 2018 Jul 1;20(7):1138–1145. doi: 10.1093/europace/eux197
- Shochat MK, Shotan A, Blondheim DS, et al. Non-Invasive Lung IMPEDANCE-Guided preemptive treatment in chronic heart failure patients: a randomized controlled trial (IMPEDANCE-HF trial). J Card Fail. 2016 Sep; 22:(9):713–722.
- Kleiner Shochat M, Fudim M, Kapustin D, et al. Early Impedance-guided intervention improves long-term outcome in patients with heart failure. J Am Coll Cardiol. 2021 Oct 26;78(17):1751–1752. doi: 10.1016/j.jacc.2021.08.036
- Botto GL, Sinagra G, Bulava A, et al. Predicting worsening heart failure hospitalizations in patients with implantable cardioverter defibrillators: is it all about alerts? A pooled analysis of nine trials. Europace. 2024 Feb 1;26(2). doi: 10.1093/europace/euae032
- Imhoff M, Lehner JH, Lohlein D. Noninvasive whole-body electrical bioimpedance cardiac output and invasive thermodilution cardiac output in high-risk surgical patients. Crit Care Med. 2000 Aug;28(8):2812–2818. doi: 10.1097/00003246-200008000-00022
- Campos PC, D’Cruz I. Functional mitral regurgitation in decompensated heart failure: combined bio-impedance and 2D echocardiography follow-up monitoring. Echocardiography. 2004 May;21(4):337–339. doi: 10.1111/j.0742-2822.2004.03118.x
- Lozano-Nieto A, Turner AA. Effects of orthostatic fluid shifts on bioelectrical impedance measurements. Biomed Instrum Technol. 2001 Jul;35(4):249–258.