1. Introduction
House dust mites (HDM) are among the main causes of asthma by inducing a type 2 bronchial inflammation in genetically susceptible individuals. The mechanisms underlying the origin and maintenance of this response have been studied during the last years, showing that innate immunity participates not only in the generation of specific IgE but also inducing inflammation and even bronchial remodeling without a relevant role of these antibodies. Besides, there have been advances in the characterization of the allergenic activity of some mite allergens, supporting their clinical relevance. In this Editorial, I will focus on two points: first, the analysis of some selected examples of HDM-induced inflammation where innate immunity plays a central role, and second, a brief discussion of new studies showing significant associations between sensitization to HDM allergens and asthma.
2. A wider vision of the immune response to HDM allergens
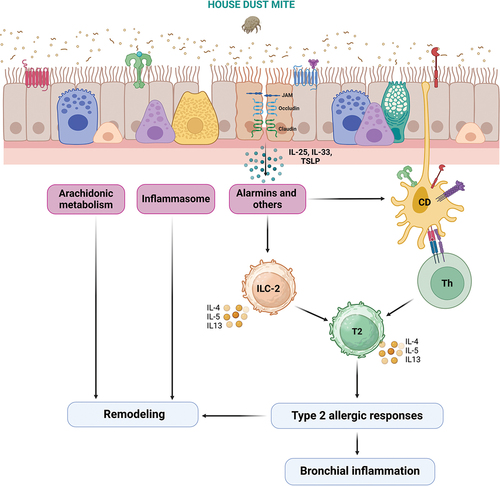
One important advance in asthma pathogenesis has been the discovery that the allergic response to HDM allergens starts with their sensing by pattern recognition receptors of the bronchial epithelium. The initial works showing the interactions of Der p 1 and Der p 2 with protease associated receptors (PAR) and toll-like receptors (TLR) have been extended to other allergens and receptors that participate in more than 40 cellular pathways [Citation1,Citation2]. An example of the current research in this field is the work of Smole et al., who discovered that Blo t 13 and Der p 13 can interact with serum amyloid A1 (SAA1) that, in contrast to the known sensing receptors, is a soluble recognition receptor. The resulting SAA1 monomers activate the SAA1-binding receptor formyl methyl receptor 2 (FMR2) inducing the production and release of IL33, which in turn activate Type 2 Innate Lymphoid Cells (ILC2), triggering a type 2 inflammation. Interestingly, among several HDM allergens tested, Blo t 13 induced the strongest production of IL-33 in bronchial epithelium cells [Citation3]. Since group 13 allergens are well represented in the HDM extract, they could play a role during the beginning of the allergic response to other allergens, as has been suggested for Der p 1 through its protease activity [Citation2]. Another interesting pathway was reported by Brusilovsky et al., who found that HDM can trigger the RIPK1-caspase 8 ripoptosome activation in epithelial cells. The active caspase 8 subsequently engages caspases 3 and 7, which directly mediate intracellular maturation and release of the well-known IL-33 alarmin [Citation4].
As the studies revealing new innate pathways of allergic inflammation are increasing [Citation1], a wider and deeper vision of the response to HDM allergens is emerging, which includes the innate immune machinery as an essential component for starting and maintaining this process.
3. The intrinsic proinflammatory effects of innate type 2 immunity
At the beginning of the past decade Barret et al. reported that HDM, by contacting dectin-2, induced an inflammatory process lead by cysteinyl leukotrienes, before IgE synthesis [Citation5,Citation6]. Five years later, it was shown that HDM induced an epithelium-dependent (sensed by protease activating receptor 2) production of leukotriene C4, increasing the proliferation of the smooth muscle from patients with severe asthma. In this case, the authors were experimentally able to confirm that specific IgE was not necessary for the observed effects on the bronchial smooth muscle [Citation7], suggesting that HDM could activate different, non-IgE mediated, pathways leading to bronchial remodeling. Another work revealed that, stimulated by Alternaria, the cysteinyl leukotrienes pathways have the potential to activate ILC2s and stimulate their production of IL-33, independently of adaptive immunity [Citation8,Citation9]. More recently, Park et al. found that HDM, sensed by dectin-1, induced the Akt-ERK1/2-C/EBP beta pathway that, in turn, triggers CCL20-mediated inflammation and epithelial-mesenchymal transition for airway remodeling without the involvement of IgE [Citation10]. Thus, these studies suggest that the innate type 2 response is able to induce bronchial inflammation and remodeling by itself, without the participation of adaptive forms of immunity.
4. ILC2s maintain chronic airway inflammation
ILC2s are an important integral of the pathophysiology of asthma. Their generation and behavior have been investigated using various strategies, including models of the allergic responses to HDM and the mold Alternaria. One of this works demonstrated that in a mouse model of chronic asthma, ILC2 and IL-33, but not T cells, were essential for maintaining the airway inflammation [Citation11]. In addition, the same group also described Alternaria-induced epigenetic changes leading to the generation of memory ILC2 that play a crucial proinflammatory role by stimulating the production of type-2 cytokines and maintaining bronchial inflammation [Citation12]. Interestingly, the proinflammatory role of ILC2, acting independently of adaptive immunity and in connection with IL-33 had been reported 12 years ago in a glycolipid-induced model of airway hyperreactivity [Citation13] suggesting that this mechanism could be induced by other molecules present in several allergen sources.
The examples described in the previous sections show different aspects of the HDM-induced type 2 bronchial inflammation, highlighting the great importance of the innate immunity. This is strongly supported by findings in other research areas such as trained immunity (in fact, recently, this type of innate memory has been demonstrated in macrophages from type 2 asthmatic patients and a mouse model of allergic airway inflammation [Citation14]), and neuroimmune mechanisms of allergic inflammation [Citation2,Citation15].
Case-control studies further explore the HDM allergens and asthma relationships.
Several case-control studies have shown the association between sensitization to HDM extracts and asthma; however, the same cannot be said for individual allergens; actually, there are few studies specially designed to perform this type of analysis. One of these works compared the IgE sensitization to Blo t 21 among 272 patients and 298 healthy controls living in the tropics, finding a significant association of this allergen with asthma (OR = 1.83, p = 0.007) [Citation16]. In this study, which included a set of 8 recombinant allergens from Blomia tropicalis, a significant association was also found between Blo t 5 and asthma (OR = 1.61 p = 0.03). Regarding D. pteronyssinus, Huang H et al. found that patients IgE-positive to Der p 37 had a higher risk of asthma (OR = 3.1) compared with Der p 37-IgE negative patients [Citation17]. The rationale of this type of research is that specific IgE antibodies result from a process that involves both innate and adaptive immunity, being a biomarker for HDM-induced inflammation and then very useful for evaluating the clinical role of allergens in asthma [Citation18]. It is expected that these studies will be done more frequently, helping to select individual allergenic components for diagnosis and immunotherapy.
5. Conclusions
Here, two critical aspects of the relationships between HDM and asthma were analyzed. As a result, the great relevance of innate mechanisms during allergic inflammation has been revealed. This in turn has been possible because of the increasing number of investigations on the mechanisms of action of allergens, which have discovered new pathways involved in the pathogenesis of HDM-induced inflammation. Interestingly, several of these pathways lead to an effector role of the ILC2/IL-33 axis, which seems to be a frequent meeting point between the innate and adaptive branches of immunity during the response against HDM allergens. Therefore, the recognition of the role of innate type 2 response is generating a new landscape of the molecular and cellular relationships between HDM and asthma (). In addition, positive association resulting from case-control studies reinforces the possibility that individual allergens have a real clinical impact. It can be said that we are experiencing a new era of HDM/allergy research that by sure will improve our understanding of the pathogenesis and management of asthma.
6. Expert opinion
Although there have been great advances in the IgE- mediated mechanisms of inflammation [Citation1], most of the data generating new research perspectives in the field are related to innate immunity. Now the possibilities of new treatments focused upstream of the IgE synthesis are becoming clearer. Also, new biomarkers for early bronchial inflammation could be found, increasing our capacity for precision allergology. In addition, it is possible that new asthma endotypes emerge associated with particular innate pathways or their combinations. Furthermore, the opportunities to define more accurately the role of individual components are now higher. Finally, a crucial, and perhaps the most difficult aspect that could start to be explored, is whether the early/innate inflammatory response induces clinical symptoms. However, there are important limitations for achieving these goals. First, so far it is almost impossible to accurately separate the innate from the adaptive response during a real in vivo inflammatory response. Looking for strategies to resolve this point should be a matter of research in the forthcoming years. Second, since not all allergens have the same mechanism of action, it is expected that the evaluation of the causes of bronchial inflammation in a specific patient will be a great challenge for personalized allergology, that goes beyond the IgE sensitization profile. Third, the idea that an allergen is a molecule that induces inflammation exclusively by binding to specific IgE is still present, limiting the scope of the research in this area. Overcoming this theoretical limitation depends on the support of projects on HDM mechanisms of action, which are expected to provide enough data for broadening the current definition of an allergen [Citation1].
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Dramburg S, Hilger C, Santos AF, et al. EAACI molecular allergology user’s guide 2.0. Pediatric Allergy Immunol. 2023 Mar;34(Suppl 28):e13854.
- Jacquet A. The HDM allergen orchestra and its cysteine protease maestro: stimulators of kaleidoscopic innate immune responses. Mol Immunol. 2023 Apr;156:48–60. doi: 10.1016/j.molimm.2023.03.002
- Smole U, Gour N, Phelan J, et al. Serum amyloid a is a soluble pattern recognition receptor that drives type 2 immunity. Nat Immunol. 2020 Jul;21(7):756–765. doi: 10.1038/s41590-020-0698-1
- Brusilovsky M, Rochman M, Rochman Y, et al. Environmental allergens trigger type 2 inflammation through ripoptosome activation. Nat Immunol. 2021 Oct;22(10):1316–1326.
- Barrett NA, Maekawa A, Rahman OM, et al. Dectin-2 recognition of house dust mite triggers cysteinyl leukotriene generation by dendritic cells. J Immunol. 2009 Jan 15;182(2):1119–1128. doi: 10.4049/jimmunol.182.2.1119
- Barrett NA, Rahman OM, Fernandez JM, et al. Dectin-2 mediates Th2 immunity through the generation of cysteinyl leukotrienes. J Exp Med. 2011 Mar 14;208(3):593–604. doi: 10.1084/jem.20100793
- Trian T, Allard B, Dupin I, et al. House dust mites induce proliferation of severe asthmatic smooth muscle cells via an epithelium-dependent pathway. Am J Respir Crit Care Med. 2015 Mar 1;191(5):538–546. doi: 10.1164/rccm.201409-1582OC
- Doherty TA, Khorram N, Lund S, et al. Lung type 2 innate lymphoid cells express cysteinyl leukotriene receptor 1, which regulates TH2 cytokine production. J Allergy Clin Immunol. 2013 Jul;132(1):205–213.
- Barrett NA, Boyce JA. Activation of group 2 innate lymphoid cells: a new role for cysteinyl leukotrienes. J Allergy Clin Immunol. 2013 Jul;132(1):214–216. doi: 10.1016/j.jaci.2013.05.019
- Park SY, Kang MJ, Jin N, et al. House dust mite-induced akt-ERK1/2-C/EBP beta pathway triggers CCL20-mediated inflammation and epithelial-mesenchymal transition for airway remodeling. FASEB J. 2022 Sep;36(9):e22452.
- Christianson CA, Goplen NP, Zafar I, et al. Persistence of asthma requires multiple feedback circuits involving type 2 innate lymphoid cells and IL-33. J Allergy Clin Immunol. 2015 Jul;136(1):59–68 e14. doi: 10.1016/j.jaci.2014.11.037
- Verma M, Michalec L, Sripada A, et al. The molecular and epigenetic mechanisms of innate lymphoid cell (ILC) memory and its relevance for asthma. J Exp Med. 2021 Jul 5;218(7):e20201354. doi: 10.1084/jem.20201354
- Kim HY, Chang YJ, Subramanian S, et al. Innate lymphoid cells responding to IL-33 mediate airway hyperreactivity independently of adaptive immunity. J Allergy Clin Immunol. 2012 Jan;129(1):216–27 e1–6.
- Lechner A, Henkel FDR, Hartung F, et al. Macrophages acquire a TNF-dependent inflammatory memory in allergic asthma. J Allergy Clin Immunol. 2022 Jun;149(6):2078–2090.
- Serhan N, Basso L, Sibilano R, et al. House dust mites activate nociceptor-mast cell clusters to drive type 2 skin inflammation. Nat Immunol. 2019 Nov;20(11):1435–1443.
- Zakzuk J, Donado K, Mondol E, et al. IgE sensitization to Blo t 21 and Blo t 5 is associated with asthma in the tropics: a case-control study. J Investig Allergol Clin Immunol. 2023;34(3): Feb 21:0. doi: 10.18176/jiaci.0892
- Huang HJ, Resch-Marat Y, Casset A, et al. IgE recognition of the house dust mite allergen Der p 37 is associated with asthma. J Allergy Clin Immunol. 2022 Mar;149(3):1031–1043.
- Caraballo L, Valenta R, Puerta L, et al. The allergenic activity and clinical impact of individual IgE-antibody binding molecules from indoor allergen sources. World Allergy Organ J. 2020 May;13(5):100118.