Abstract
Background Non-steroidal anti-inflammatory drugs (NSAIDs) are known to be potent inhibitors of new bone formation. We investigated whether NSAIDs given at surgery influence the long-term results after total hip arthroplasty (THA).
Patients and methods We performed a 10-year follow-up on 142 of 144 patients who had taken part in a randomized trial on the preventive effects of the NSAID ibuprofen on heterotopic ossification after THA. 96 patients were treated with ibuprofen: 48 for 1 week postoperatively, 48 for 2 weeks postoperatively, and 48 patients were not treated.
Results 13 patients had been revised. All revisions except 1 belonged to groups treated with ibuprofen. The 10-year risk for revision was significantly higher in the ibuprofen-treated patients (p = 0.05). Eleven of the revisions occurred due to fractures of the femur (2) or aseptic loosening (9), reasons that may be attributed to negative effects of ibuprofen. For these patients, the 10-year risk for revision was not statistically significantly different between treated and untreated patients (p = 0.08). In addition to the revised patients, 94 other patients were alive at the 10-year follow-up and 84 underwent radiographic examination. 9 loose prostheses were found radiographically, but these were equally distributed between ibuprofen-treated and untreated hips.
Interpretation The high proportion of revisions in the ibuprofen groups, in combination with clinical and experimental evidence of inhibitory effects on new bone formation of NSAIDs, warrants further investigation of the effects of these drugs on prosthetic fixation.
▪
One major concern when using NSAIDs in a newly operated total hip arthroplasty is the possible effect on prosthetic fixation. There is both experimental and clinical evidence of inhibition of new bone formation by NSAIDs. For example, NSAIDs inhibit bone in-growth in porous implants (Keller et al. Citation1989), delay fracture healing (Rø et al. Citation1976, Sudmann et al. Citation1979, Altman et al. Citation1995), inhibit spinal fusion in rats (Dimar et al. Citation1996), and inhibit experimental bone induction (Törnkvist et al. Citation1985). Clinically, NSAIDs have been found to retard healing of diaphyseal femur fractures and spinal fusions (Glassman et al. Citation1998, Giannoudis et al. Citation2000). In addition, several randomized clinical studies have provided evidence of the high efficacy of NSAIDs in preventing heterotopic ossification, which strongly suggests that these drugs also have effects on human bone metabolism (Schmidt et al. Citation1988, Kjaersgaard-Andersen et al. Citation1993, Gebuhr et al. Citation1996, Persson et al. Citation1998). As in the case of fracture healing, the surgical trauma of THA induces reparative processes, which are necessary for a durable prosthetic fixation by bone regeneration on and into the bone cement or the prosthesis. Reduction or inhibition of bone repair will result in a less stable fixation, or even an unstable implant. For these reasons, we studied the long-term outcome of postoperative treatment with NSAIDs on prosthetic fixation. We had the opportunity to do so by performing a 10-year follow up on patients from a previous randomized study of our own, in which the effect of an NSAID on hetrotopic bone formation after hip arthroplasty was studied (Persson et al. Citation1998).
Patients and methods
In a previous study we used a prospective, randomized, double-blind and placebo-controlled design involving 144 patients operated on with primary THA for osteoarthritis between 1987 and 1989, to investigate the efficacy of short-term medication with NSAIDs in prevention of the development of HO after THA (Persson et al. Citation1998). Patients with rheumatoid disease or complications regarding fractures, and patients with contraindications to the use of NSAIDs (such as a history of liver or kidney failure, previous allergic reaction to salicylates or NSAIDs, or gastric ulcer/gastritis) were not included.
One half of the patients were operated at Karolinska Hospital, Stockholm, and the other half at Kristianstad Central Hospital. The study was approved by the local ethics committees of the hospitals, and all patients signed an informed consent form. The patients were randomized into 3 groups with 48 patients in each; these were equivalent regarding sex distribution and the hospital where the surgery was performed.
The different treatments were:
Ibuprofen from the day of surgery, for 3 weeks.
Ibuprofen for 1 week, and then placebo for 2 weeks.
Placebo for 3 weeks.
Treatment with ibuprofen (Ibumetin, Alfred Benzon AB, Helsingborg, Sweden; 400 mg 3 times daily) or placebo was started on the day of surgery. The medication was given as suppositories on the first two days postoperatively, and as tablets for the remaining time.
All patients were operated through a posterolateral incision. A conventional cementing technique with irrigation and cement pressurization was used. After insertion of a Charnley or an Exeter prosthesis, the wound was thoroughly irrigated with saline. Suction drainage was used for 24 hours. The patients were allowed full weight bearing from the first postoperative day.
Prophylaxis against thrombo-embolism was given with low molecular weight heparin (Fragmin, Pharmacia, Stockholm, Sweden; 5,000 IE subcutaneously) for 10 days from the day of surgery. 0.5 L Dextrane was given intravenously during surgery. A single dose of 2 g cloxacillin was given at the start of surgery.
The patients were not treated with other NSAIDs, salicylates, systemic steroids, bisphosphonates, or other drugs with known effects on bone during the first 3 months after surgery. The two ibuprofen-treated groups of patients developed less HO than the placebo group after 3 and 12 months of follow-up (Persson et al. Citation1998).
10-year follow-up (present report)
10 years after surgery, all 144 of the patient medical records were reviewed. 13 patients had had their THA revised and 37 patients had died. According to the records, none of the latter patients had been reoperated. A questionnaire concerning further surgery and symptoms from the operated hip was sent to the 107 patients who had survived. In Sweden, a unique 10-digit personal ID number makes it possible to identify patient records, radiographic examinations, current address, or even the time and cause of death.
94 patients who were still alive, but who had not been reoperated, were offered a follow-up radiographic investigation. 84 patients (51 women) participated in the radiographic follow-up. In addition, 6 patients answered the questionnaire but declined the radiographic follow-up. 2 patients were contacted by telephone but declined to participate due to advanced age, and 2 patients could not be located ().
Table 1. 10-year follow-up
We decided on two levels of failure before the 10-year follow-up:
Revision surgery with exchange or removal of one or both prosthetic components. This definition of revision is used by the Swedish National Hip Arthroplasty Register (Malchau et al. Citation2002).
Radiographic loosening in patients who were not reoperated.
Criteria for radiographic loosening
The acetabular cup was considered loose when one or more of the following criteria were fulfilled (Hodgkinson et al. Citation1988): 1) there was a visible zone around the whole circumference of the cement-bone interface on an AP radiograph, the width of the zone exceeding 2 mm along the entire circumference; 2) migration of more than 3 mm in any direction compared to the postoperative radiographs.
The femoral component was considered loose when one or more of the following criteria were fulfilled: 1) more than 5 mm distal migration of the femoral component within the cement mantle, 2) visible fracture of the cement mantle, 3) more than 5 mm distal migration of the femoral component between bone and cement, and presence of radiolucency between bone and cement which is more than 2 mm wide in more than one Gruen zone, 4) mid-stem pivoting of the prosthesis with a lateral stem-tip shift of more than 3 mm, 5) medial calcar shift of the prosthesis of more than 3 mm, 6) visible metal fatigue fracture of the femoral stem.
The THA was defined as radiographically loose when one or both components fulfilled one or more of the criteria above. Evaluation of the radiographs was performed by an experienced radiologist (A-M.B.) without knowledge of the treatment.
Statistics
All analyses were based on two groups: the placebo group and the combined ibuprofen groups.
We used the following definitions:
A THA was defined to be a failure if the THA was revised with exchange or removal of one or both prosthetic components (Malchau et al. Citation2002).
A THA was censored if the patient died without having had a revision operation, or if the patient survived the 10-year period without a revision.
A Kaplan-Meier survival analysis was done with revision of the prosthesis as the endpoint, and a log-rank test was used to determine whether there was a significant difference in risk for revision at 10 years between the placebo group and the combined ibuprofen groups.
In addition, we examined differences between the groups regarding risk for revision andradiographic loosening at 10 years.
Results
Revision
13 of the 107 patients who were still alive after 10 years had had their THA revised. The reasons for revision were: aseptic loosening (9 patients), fracture of the femur around the femoral stem after moderate trauma (2 patients), recurrent dislocations (1 patient) and septic loosening (1 patient) (). All 12 aseptic complications occurred in men; 11 of these belonged to the treatment groups (5 patients had been treated for 8 days, and 6 patients had been treated for 21 days). The revision rate was 9% for all patients at 10 years (13/144).
Table 2. Indications for revision surgery
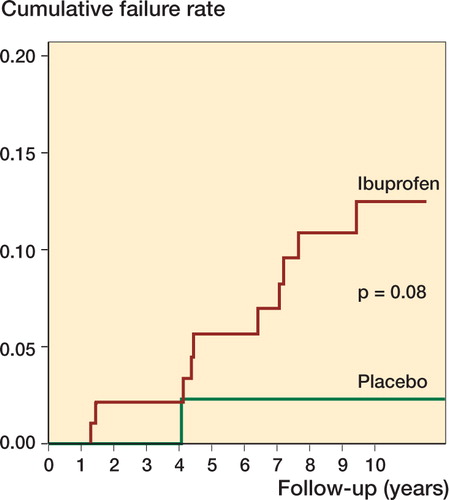
When we applied our criterion for failure (revision for any reason), the 10-year risk for revision in the combined ibuprofen groups was 15% (95% CI: 9%–24%) and it was 2.4% in the placebo group (95% CI: 0.3%–16%) (p = 0.05) ().
Figure 1. Failure (revision) curve for 142 of the original 144 THAs. Failure curve (Kaplan-Meier), showing all revisions.The placebo-treated patients (green) have been compared to the combined ibuprofen-treated groups (red).
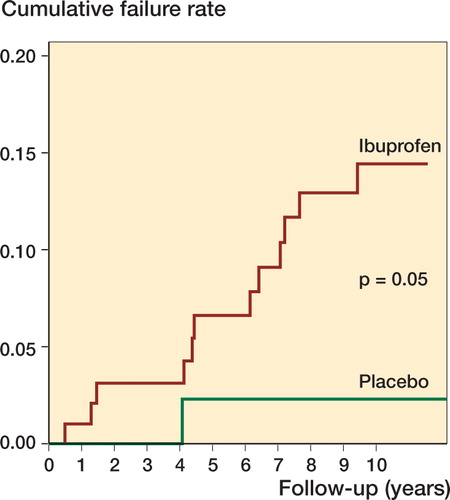
To specifically analyze the effects of ibuprofen on prosthetic fixation, we performed a second analysis in which the 2 patients who were revised due to recurrent dislocation or septic infection were not classified as failures, but were censored at the time of their reoperation. The 10-year risk of failurewas now 12% (95% CI: 6.8%–22%) in the ibuprofen-treated patients and 2.4% (95% CI: 0.3%–16%) in untreated patients (p = 0.08) ().
Radiographic loosening
Of the remaining 94 surviving and unrevised patients, 84 (51 women) accepted a radiographic examination. There were 33 patients in the placebo group, 26 in the 8-day treatment group, and 25 in the 21-day treatment group (). Radiographic loosening was found in 9 patients. 4 patients belonged to the placebo group and 5 patients to the group treated with ibuprofen for 21 days ().
Table 3. Radiographic loosening: 10-year follow-up
When all revisions and cases of radiographic loosening were combined, there were 5 failures in the placebo group, 6 in the 8-day ibuprofen group and 11 in the 21-day ibuprofen group (). The difference between the combined ibuprofen groups and the control group was not statistically significant (p = 0.2).
Table 4. Failures: revisions and radiographic loosening at the 10-year follow-up examination
Discussion
The mechanism of action of ibuprofen and other NSAIDs on bone formation is most probably through their effects on prostaglandin E2 (PGE2) and other PGs, as these substances have profound effects on osteogenesis and bone remodeling. Since NSAIDs act as potent inhibitors of prostaglandin synthesis, it is possible that perioperative and postoperative treatment with NSAIDs can deteriorate the interface between bone and prosthesis, thus increasing the risk of prosthetic loosening and failure. Similarly to fracture healing, the surgical trauma of THA induces a cascade of reparative processes, which are mediated to a great extent through the action of cytokines, including the prostaglandins. Interestingly, experimental and clinical studies have indicated that the early phase of bone regeneration after trauma is especially sensitive to inhibition by NSAIDs (Törnkvist et al. Citation1985, Nilsson et al. Citation1986, Sodemann et al. Citation1988) and this is also the time period during which a cemented implant becomes fixed by bone apposition.
One aspect of diagnosis of endoprosthetic loosening in THA concerns the necessary follow-uptime.The early fixation of the prosthetic components is probably of crucial importance for the long-term survival, and there may be a considerable time lag before micromotions in the cement-bone interface result in gross prosthetic failure(Mjöberg Citation1997). Thus, many authors consider even “late loosening” to be a consequence of early, deficient prosthetic fixation. This view is further supported by findings in studies using radiostereometric analysis (RSA) to investigate the pattern of motion of prosthetic components. RSA analyses have demonstrated a clear correlation between early micromotion in the cement-bone interface and subsequent prosthetic loosening, even though the clinical failure may not occur until late (Mjöberg Citation1997). Thus, long-term studies are necessary to determine the effects of different treatments on endoprosthetic fixation—even if the treatment is given early after surgery.
To investigate the risk of endoprosthetic revision in patients treated with NSAIDs, we performed 10-year follow-up investigation of 144 patients who had taken part in a double-blind, placebo-controlled study on the preventive effects of the NSAID ibuprofen on heterotopic ossification after THA. In our original study (Persson et al. Citation1998), 144 patients were operated with THA for osteoarthritis between 1987 and 1989, and randomized into 3 groups: 2 with short-term ibuprofen treatment (8 and 21 days) and 1 placebo group. After 10 years, 13 patients had been reoperated with exchange of one or both prosthetic components. 12 of these patients were men, 11 of them belonging to either of the treatment groups, and 1 to the placebo group. The difference between the placebo group and the treatment groups was significant (p = 0.05). The overall revision rate (9%) was acceptable. The only revision performed in a woman was done for deep infection, so all revisions for aseptic loosening were performed on men. The relatively small number of patients and the shorter mean survival time for men (more men were censored), combined with a low overall complication rate, makes the statistical analysis difficult to interpret. In one of the analyses, we censored 2 revisions (both belonging to the ibuprofen groups) since those revisions were performed for reasons that probably cannot be attributed to reduced bone formation: 1 recurrent dislocation and 1 deep infection. In this analysis, the difference was not statistically significant between the placebo group and the treatment groups (p = 0.08). However, the fact that 10 out of 11 revisions that were performed for aseptic loosening or femur fracture occurred in the ibuprofen-treated groups is a matter of great concern.
The authors wish to thank Jonas Ranstam Ph.D. for help with the statistical analysis.
This study was supported by grants from the Swedish Medical Research Council, grant no. 06577-13B.
No competing interests declared.
- Altman R D, Latta L L, Keer R, Renfree K, Hornicek F J, Banovac K. Effect of nonsteroidal antiinflammatory drugs on fracture healing: a laboratory study in rats. J Orthop Trauma 1995; 9(5)392–400
- Dimar J R, 2nd, Ante W A, Zhang Y P, Glassman S D. The effects of nonsteroidal anti-inflammatory drugs on posterior spinal fusions in the rat. Spine 1996; 21(16)1870–6
- Gebuhr P, Sletgård J, Dalsgård J, Soelberg M, Keisu K, Hänninen A, Crawford M. Heterotopic ossification after hip arthroplasty: a randomized double-blind multicenter study tenoxicam in 147 hips. Acta Orthop Scand 1996; 67(1)29–32
- Giannoudis P V, MacDonald D A, Matthews S J, Smith R M, Furlong A J, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg (Br) 2000; 82(5)655–8
- Glassman S D, Rose S M, Dimar J R, Puno R M, Campbell M J, Johnson J R. The effect of postoperative nonsteroidal anti-inflammatory drug administration on spinal fusion. Spine 1998; 23(7)834–8
- Hodgkinson J P, Shelley P, Wroblewski B M. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop 1988, 228: 105–9
- Keller J C, Trancik T M, Young F A, St Mary E. Effects of indomethacin on bone ingrowth. J Orthop Res 1989; 7(1)28–34
- Kjaersgaard-Andersen P, Nafei A, Teichert G, Kristensen O, Schmidt S A, Keller J, Lucht U. Indomethacin for prevention of heterotopic ossification. A randomized controlled study in 41 hip arthroplasties. Acta Orthop Scand 1993; 64(6)639–42
- Malchau H, Herberts P, Eisler T, Garellick G, Soderman P The Swedish Total Hip Replacement Register. J Bone Joint Surg (Am) (Suppl 2) 2002; 84: 2–20
- Mjöberg B. The theory of early loosening of hip prostheses. Orthopedics 1997; 20(12)1169–75
- Nilsson O S, Bauer H C, Brosjö O, Törnkvist H. Influence of indomethacin on induced heterotopic bone formation in rats. Importance of length of treatment and of age. Clin Orthop 1986, 207: 239–45
- Persson P E, Sodemann B, Nilsson O S. Preventive effects of ibuprofen on periarticular heterotopic ossification after total hip arthroplasty. A randomized double-blind prospective study of treatment time. Acta Orthop Scand 1998; 69(2)111–5
- Rø J, Sudmann E, Marton P F. Effect of indomethacin on fracture healing in rats. Acta Orthop Scand 1976; 47(6)588–99
- Schmidt S A, Kjaersgaard-Andersen P, Pedersen N W, Kristensen S S, Pedersen P, Nielsen J B. The use of indomethacin to prevent the formation of heterotopic bone after total hip replacement. A randomized, double-blind clinical trial. J Bone Joint Surg (Am) 1988; 70(6)834–8
- Sodemann B, Persson P E, Nilsson O S. Prevention of periarticular heterotopic ossification following total hip arthroplasty. Clinical experience with indomethacin and ibuprofen. Arch Orthop Trauma Surg 1988; 107(6)329–33
- Sudmann E, Dregelid E, Bessesen A, Morland J. Inhibition of fracture healing by indomethacin in rats. Eur J Clin Invest 1979; 9(5)333–9
- Törnkvist H, Bauer F C, Nilsson O S. Influence of indomethacin on experimental bone metabolism in rats. Clin Orthop 1985, 193: 264–70