Abstract
Background There is no consensus as to whether to use a posterior cruciate ligament (PCL) retaining design or a posterior-stabilized design for total knee arthroplasty. The objective of this study was to establish the difference in functional, clinical, and radiological outcome between retention and removal of the PCL.
Methods We conducted a search in Medline, EMBASE, the Cochrane database, and Current Contents, along with reference checks and citation tracking. Randomized controlled trials were selected and methodological quality was assessed with the van Tulder and Jadad checklists by 2 independent reviewers.
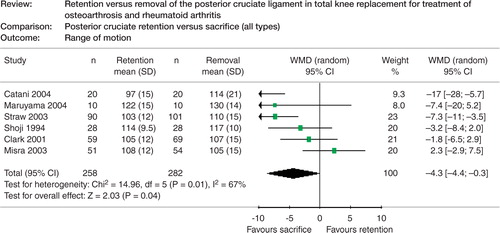
Results We found 8 randomized controlled trials. 2 treatment options were compared against PCL retention: PCL removal without post and cam mechanism (2 studies), and posterior-stabilized design (5 studies). 1 study included all 3 options. Range of motion was found to be 8° higher (105° vs. 113°) in the posterior-stabilized group compared to the PCL retention group (p = 0.01, 95% CI (1.7, 15)).
Interpretation These results should be interpreted with caution, as the methodological quality of the studies was highly variable. Suggestions are given to improve future research on this specific aspect of knee arthroplasty.
▪
In the healthy knee, the posterior cruciate ligament (PCL) causes posterior translation of the femur onto the tibia when the knee is flexed. This is produced by the nature of its relative insertion sites posteriorly on the tibia and femur. As the knee is flexed, the PCL is tensioned because the femoral insertion site moves anteriorly. As a result, the femur is pulled posteriorly onto the tibia. This phenomenon is called “roll-back” and determines the AP contact position of the femur on the tibia. The contact point is maintained at approximately 2–5 mm posterior to the middle of the tibia plateau, located at 54–60% of the anteroposterior diameter of the medial tibia (Freeman and Pinskerova Citation2003, Komistek et al. Citation2003). Also, the PCL is the strongest ligament that prevents opening of the joint in flexion. Removal of the PCL results in an increase in the flexion gap of 5 mm (Mihalko and Krackow Citation1999).
For total knee arthroplasty (TKA), it is desirable to reproduce the natural knee movements and stability during the whole range of motion. In patients for whom the PCL can be retained, the PCL can provide these requirements (Mihalko and Krackow Citation1999, Lombardi et al. Citation2001). In TKA, AP laxity gives the best results if between 8–11 mm, and the contact point in flexion should be at approximately the posterior one-third of the AP dimension of the tibia (Pellengahr et al. Citation1999). If the PCL is removed, this increase is generally compensated for with a thicker polyethylene insert or larger femoral components.
The factors influencing the choice of either removal or retention are the degenerative status of the PCL, the type of implant used, or just the personal preference of the surgeon. Lomardi et al. (Citation2001) proposed a decision tree based on the patient's history, the clinical examination, and the intraoperative findings. Some randomized studies on the effect of retention or removal of the PCL have been published (Vinciguerra et al. Citation1994, Stiehl et al. Citation1997, Tanzer et al. Citation2002, Straw et al. Citation2003). None of these studies (individually) could find a difference between the two treatments. The question remains whether the studies allow for pooling and whether the pooled results favor retention or removal of the PCL.
The objective of this study was to identify the difference in functional, clinical, and radiological outcome between retention and removal of the posterior cruciate ligament in total knee arthroplasty in patients with osteoarthrosis and other non-traumatic diseases. A secondary objective was to identify factors that influence the results, such as disease severity, polyethylene bearing mobility, patella resurfacing, age, and sex.
Methods
Search strategy for identification of studies
In order to assemble all the relevant literature, we used a sensitive search in the most common data-bases of published medical literature: the Cochrane database of randomized controlled trials (issue 2004–1), Current Contents (January 1996–March 2004), Medline (via Pubmed; January 1966–March 2004) and Embase (up to and including March 2004). The search strings are given in . The same search strategy was adopted for the different databases. We made no restrictions as to language or date. A final check that no relevant articles had been missed was carried out both by screening the references from the articles and by performing citation tracking on the articles that had been selected.
Table 1. Search strings
Selection of studies
One reviewer conducted the literature search and retrieved the references to be evaluated. Two reviewers independently selected the trials to be included in the review. Disagreements were resolved by consensus. When no consensus could be reached, a third reviewer was available to give a decisive vote. Articles were selected in 2 steps. In the first step, some were excluded when it was apparent from the title or abstract that the study did not meet all of the following criteria. The study type had to be a randomized controlled trial. Quasi-randomized trials such as those using date of birth or alternating sequences were excluded. The intervention evaluated in the trials had to be primary total (bi- or tri-compartmental) knee replacement (excluding post-patellectomy and post-osteotomy studies) comparing one treatment in which the PCL was retained against one in which it was removed. Procedures with removal of the PCL were considered when the same prosthesis design was used as for the retention group, or when a posterior-stabilized design or a deep dish insert was used. The indication for the subjects to receive total knee arthroplasty had to be osteoarthrosis or other nontraumatic diseases of the knee joint. Studies which included a wider range of indications were excluded if the proportion of osteoarthrosis and other nontraumatic diseases was lower than 95% of the group. The outcome measurement in the studies had to be a functional, clinical or radiological measure. Primary outcome measures were pain, impairment (anterior-posterior stability, range of motion) or disability/handicap (WOMAC, SF-36). The minimal follow-up had to be 12 months.
In the first step, only the title and abstract were available. In the second step, articles which passed the first step were retrieved and again evaluated against the criteria of the first step. In this step, multiple publications of the same study population were excluded. We did not apply blinding in this step. Reference details were managed with the aid of Reference Manager (ISI ResearchSoft, CA). In addition, relevant information was recorded pertaining to database source, reason for exclusion and consensus of reviewers.
Assessment of methodological quality
Articles that met all the above criteria were examined closely by Two reviewers independently. Methodological quality was assessed with the aid of the checklists by van Tulder (Citation1997, Citation2003) and Jadad et al. (Citation1996) (). We did not use a cut-off point for methodological quality. When no consensus between the two reviewers was achieved, a third reviewer was consulted for the decisive vote.
Table 2. Methodological criteria
Data collection
Data was extracted using a predeveloped form and entered into Review Manager software version 4.2.7 (RevMan Oxford, England, The Cochrane Collaboration, 2003) by 2 reviewers. Items in this form were study type, population, sample size, treatment characteristics, and outcome parameters. For study type, randomization technique, allocation concealment, and blinding were recorded. For population, the affiliation, the period of inclusion, the inclusion and exclusion criteria, and the age, sex, work status, and race of the patients were recorded. For sample size, the number of patients who met the inclusion criteria, who were randomized and who were followed up were recorded. For all outcome variables, quantitative results were recorded as well as complications encountered in the treatment groups.
Analysis
Statistical analyses were conducted using RevMan. Continuous data (e.g. visual analog scales of pain, patient global assessment) were entered as means and standard deviations, and dichotomous out-comes (e.g. response, improvement) as number of events. Standard deviations were used when available. When not provided, standard deviations were imputed from comparable studies or from original scores when calculating change scores. In the absence of significant heterogeneity, and given sufficient included trials, results were combined using weighted mean difference or standardized mean difference (depending on comparability of scales) for continuous data, and relative risk for dichotomous data (given that the event is not rare). A random-effects model was used for all analyses in this review (Fleiss Citation1993). A test of heterogeneity of the data was performed and if significant (p < 0.05 using the X2 statistic), the source of heterogeneity was investigated by performing a sensitivity analysis and considering clinical reasons for potential clinical heterogeneity.
Results
The individual databases resulted in 512 (Medline), 306 (Current Contents), 364 (EMBASE), and 186 (Cochrane Central register of controlled trials) references. After citation tracking, 17 abstracts were retrieved because the studies were possibly relevant; and after screening of the references, 14 more abstracts. 1 study (Maruyama et al. Citation2004) was found with a final check with the same search strings in Medline after the review process. The total search resulted in 939 references, duplicate references not included.
From the information in the title, we excluded 876 references, and 46 references were excluded after examination of the abstract. For 9 references, we needed to examine the article in more detail to decide either that the outcome parameter or timing (1 study; Cope et al. Citation2002) was not within the goal of the review, or that the randomization technique was not valid (8 studies; Dorr et al. Citation1988, Vinciguerra et al. Citation1994, Cash et al. Citation1996, Laskin Citation1996, Citation1997, Simmons et al. Citation1996, Stiehl et al. Citation1997, Ishii et al. Citation1998). This left 8 studies involving 576 patients in the review ().
Table 3. Characteristics of randomized controlled trials included
2 studies (Shoji et al. Citation1994, Misra et al. Citation2003) were included which compared the same implant with and without removal of the PCL. 5 studies (Clark et al. Citation2001, Tanzer et al. Citation2002, Catani et al. Citation2004, Maruyama et al. Citation2004, Swanik et al. Citation2004) were included which compared a posterior cruciate retaining design with a posterior-stabilized design. 1 study (Straw et al. Citation2003) randomized patients into all 3 groups. The decision to use these types of comparisons was made after the articles had been selected and the comparisons found had been evaluated.
Description of studies
Participants: In 5 studies, there were no selection criteria (Shoji et al. Citation1994, Tanzer et al. Citation2002, Straw et al. Citation2003, Misra et al. Citation2003, Catani et al. Citation2004). Osteoarthrosis and rheumatoid arthritis patients were included. In the remaining studies (Clark et al. Citation2001, Maruyama et al. Citation2004, Swanik et al. Citation2004), osteoarthrosis and deformity less than 10–20 degrees were specific selection criteria.
Interventions: In 5 studies, the comparison was a PCL retention prosthesis versus PCL removal in a posterior-stabilized prosthesis (AMK (Clark et al. Citation2001), PFC (Maruyama et al. Citation2004), Nexgen (Swanik et al. Citation2004), Nexgen/Legacy (Tanzer et al. Citation2002), and Optetrak (Catani et al. Citation2004)). In 2 studies, the same kind of prosthesis was used for both groups (PFC (Misra et al. Citation2003), and Total Condylar Modifier (Shoji et al. Citation1994)). 1 study used all 3 treatments (Genesis-I (Straw et al. Citation2003)). The patella was resurfaced in 1 study (Clark et al. Citation2001), partly resurfaced in 2 studies (Tanzer et al. Citation2002, Misra et al. Citation2003) and not described in the other 5 studies. The type of polyethylene bearing (mobile, fixed or rotating) was not described in any study. Description of the brand of the prosthesis can usually give an indication of the bearing type, but the increasing tendency of the prosthesis industry to offer any type of implant makes this uncertain. 4 studies (Clark et al. Citation2001, Tanzer et al. Citation2002, Misra et al. Citation2003, Catani et al. Citation2004) used a cemented implant, while the other studies did not provide information about cementing. The anterior-posterior balancing of the flexion space was described in 3 studies (spacer blocks (Clark et al. Citation2001, Tanzer et al. Citation2002), and Monogram Balancer), mediallateral flexion space balancing was described in 3 studies (posterior condylar axis (Maruyama et al. Citation2004), Monogram Balancer (Straw et al. Citation2003), and epicondylar axis (Tanzer et al. Citation2002)).
Outcome: All studies used a clinical rating scale (Knee Society score or Hospital for Special Surgery score) and range of motion or flexion measurements.
Sponsorship: There was a mention of lack of sponsorship in 6 of the trials (Tanzer et al. Citation2002, Misra et al. Citation2003, Straw et al. Citation2003, Catani et al. Citation2004, Maruyama et al. Citation2004, Swanik et al. Citation2004), and in 2 trials sponsorship was not mentioned at all (Shoji et al. Citation1994, Clark et al. Citation2001).
Methodological quality of the studies included
Among the reviewers, there was disagreement on 46% of the item scores of the van Tulder et al. (Citation1997, Citation2003) checklist and on 9% of the items of the Jadad (Citation1996) checklist, but disagreements could all be solved in consensus. Overall, the methodological quality of the trials was found to be low. This was only partly a result of poor methodology, and may have been more a consequence of incomplete reporting. Blinding is rarely used in orthopedic surgery trials, which was confirmed by the studies found in this review. None of the studies used blinding of the surgeon. 2 studies used patient blinding and 4 studies used observer blinding. The randomization technique was only mentioned in 2 of the 8 trials (“table-generated randomization”) and allocation concealment was never documented. The methodological score of the trials (with general remarks) is given in . These scores are based on the published article, and are thus not a judgement of the trial, but only of the printed report of the trial.
Table 4. Methodological quality of randomized controlled trials found in the review
Meta-analysis
A meta-analysis was performed for the parameters which were presented in more than one study. For both treatment comparisons, these were range of motion, change in range of motion, flexion angle, Knee Society clinical, functional and total score, Hospital for Special Surgery score, or any clinical score. For the separate comparisons (PCL-retention vs. posterior-stabilized or using the same prosthesis), only range of motion and change in range of motion could be used in a meta-analysis. Complications were reported in only 4 trials ().
Range of motion showed a difference favoring PCL removal (p = 0.04). The results were heterogeneous (; p = 0.01). A clinical reason for this heterogeneity could be whether or not a post-and-cam system (also called a posterior-stabilized (PS)) system was used to replace the PCL. When looked at separately, PCL retention versus PCL removal without PS system did not show any significant difference (; difference –4°; 95% CI (–11, 3.4); p = 0.3), whereas PCL removal (105°) versus PS (113°) system showed a significant difference of 8° (95% CI (1.7, 15)) in favor of the PS design (; p = 0.01). Heterogeneity was reduced for the second comparison (p = 0.03), but increased with the first (p = 0.003).
Figure 2a. Meta-analyses of range of motion for combination of studies comparing PCL retention with sacrifice in the same kind of prosthesis.
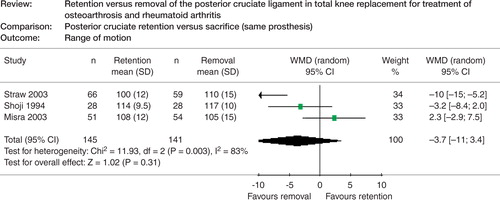
Figure 2b. Meta-analyses of range of motion for combination of studies comparing PCL retention with sacrifice and replacement with a post-and-cam mechanism.
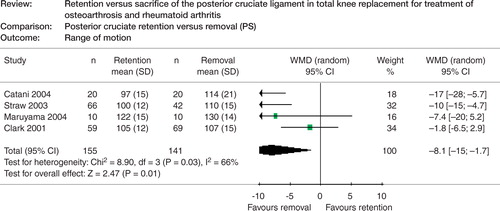
Table 5. Complications
Hospital for Special Surgery score also showed a difference (p = 0.03) favoring PCL removal (with or without PS) of –1.6 points (95% CI (–3.1, –0.1)). For all other outcome parameters, no significant difference was found. Further subgroup analyses to answer the secondary question of the study could not be performed.
Best evidence synthesis
There were 2 studies (Tanzer et al. Citation2002, Swanik et al. Citation2004) which scored “yes” on 50% or more of the van Tulder et al. (Citation1997, Citation2003) criteria. However, in orthopedic surgery concerning implants “surgeon blinding” is not feasible. In that case 4 studies (Tanzer et al. Citation2002, Misra et al. Citation2003, Catani et al. Citation2004, Swanik et al. Citation2004) would score “yes” on 50% or more of the criteria, and can be used in the best evidence synthesis.
1. Posterior cruciate retention versus removal using identical prostheses
The only high-quality study was that of Misra et al. (Citation2003). They found no difference for any of their parameters (range of motion, Hospital Special Surgery score, satisfaction).
2. Posterior cruciate retention versus posterior-stabilized (PS) implant
The 3 high-quality studies were those of Catani et al. (Citation2004), Tanzer et al. (Citation2002), and Swanik et al. (Citation2004). Catani et al. found a higher range of motion for the PS group. No differences in migration parameters and for Knee Society score and Hospital for Special Surgery score were found. Tanzer et al. found no difference between the two groups for Knee Society Score, range of motion, flexion, pain or radiological measurements. Swanik et al. measured proprioception, kinesthesia and balance. The group with PS design had a significantly better reproduction angle when moving from extension. Unfortunately, no other outcome variables were measured.
Discussion
The choice of whether to use a posterior cruciate retaining design or a posterior stabilized design for total knee arthroplasty relies on limited scientific evidence. Our meta-analysis showed only a difference in range of motion favoring posterior-stabilized designs over PCL retention designs of 8 degrees. Although the evidence can be classified as “strong” (meta-analyses of more than one high-quality RCT), one should be aware that the effect is still unstable and sensitive to the inclusion of new studies.
Looking at the best available evidence—individual, high-quality RCTs—there is strong evidence that there is no difference between PCL retention and PCL removal in the same prosthesis. There is also strong evidence that the PS design results in a better range of motion and reproduction angle.
Even in a systematic review, publication bias can never be ruled out with certainty. We applied a relatively broad search strategy in the databases used, which meant that 937 references could be evaluated. Some references are not indexed in the data-bases. Thus, we also used citation tracking, and we checked the reference lists of the articles that were included. A critical note has to be made on pooling data from separate studies. The Hospital for special surgery score and Knee Society score are composite scores, and it is not immediately clear what the implication is of a score change if it is not clear what part of the score changes. The subscores such as range of motion provide more meaningful results.
During the search, we found several studies which used inappropriate randomization techniques or did not claim to be randomized, and they were thus excluded (Dorr et al. Citation1988, Becker et al. Citation1991, Maloney and Schurman Citation1992, Hirsch et al. Citation1994, Vinciguerra et al. Citation1994, Cash et al. Citation1996, Laskin Citation1996, Simmons et al. Citation1996, Stiehl et al. Citation1997, Ishii et al. Citation1998, Pereira et al. Citation1998, Udomkiat et al. Citation2000, Cope et al. Citation2002). In all of these studies, we cannot rule out selection bias, so the results should be interpreted with less certainty than the results from the meta-analysis and best-evidence synthesis.
Range of motion was the parameter most measured. Only 1 trial (Straw et al. Citation2003) found a significant difference favoring PCL removal, and the pooled result of 6 trials was just significant. Stiehl et al. (Citation1997) found a better range of motion for a PCL retaining implant and Maloney et al. (Citation1992) found a better range of motion for a PS design. Both studies were, however, not adequately randomized and had a higher preoperative range of motion for the superior group. Preoperative range of motion is believed to have a large influence on the postoperative results. Therefore, change of range of motion should be calculated and reported as well. This was done in only 3 trials, which found no difference. Hirsch (Citation1994) also found a superior range of motion for a PS design over as well PCL removal as retention in a prosthesis without posterior stabilization.
Fluoroscopy (Udomkiat et al. Citation2000) has revealed more natural anteroposterior femorotibial translation for the PS design. As shown in some studies (Mahoney et al. Citation1994, Dennis et al. Citation1998), the lack of posterior translation in PCL-retaining TKA is thought to be attributable to negligence in balancing the PCL in flexion (Emodi et al. Citation1999, Nozaki et al. Citation2002, Most et al. Citation2003). Balancing the PCL means choosing the insert thickness and component sizes such that the PCL is adequately under tension in the flexed position, but relaxed in extension. Alternatively, a PCL release can be used in cases with a tight ligament and a tight flexion gap. When PCL balancing has not been performed adequately, the patient has a PCL-deficient TKA with pain and flexion instability if the PCL is too loose (Pagnano et al. Citation1998, Waslewski et al. Citation1998, Morberg et al. Citation2002). If the PCL is too tight, the patient suffers from limited flexion, and the polyethylene insert is subjected to high stresses and wear (Pagnano et al. Citation1998, Migaud and Tirveilliot Citation2002).
The PCL has been reported to have proprioceptive properties (Hogervorst and Brand Citation1998). Swanik found a better reproduction angle for a PS design in grade II and III arthrosis. Cash et al. (Citation1996) found no difference in proprioception between a PCL retention design and a PS design. Simmons et al. (Citation1996) found no difference in pro-prioception in moderate grades of osteoarthrosis, but in higher grades, the cruciate-retaining group performed better.
Gait analysis can provide more meaningful results. In the review, however, we did not find any studies that evaluated this. Significant differences have, however, been found in non-randomized studies. Dorr et al. (Citation1988) evaluated gait analysis and found greater medial reaction forces and higher joint reaction forces for PS implants, which may lead to more wear. Ishii et al. (Citation1998) found increased abduction and adduction and increased proximal and distal translation during gait analysis for the PS design, which may indicate reduced stability. Laskin (Citation1996) included large fixed deformities and found that PCL retention in these cases led to increased pain, radiolucencies, range of motion and consequently increased revision rate. The outcomes anterior-posterior stability and contact position are highly relevant to the question at hand. These questions were not addressed in any of the studies. In a laboratory study, Most et al. (Citation2003) concluded that proper balancing is imperative in order to achieve proper rollback.
Sensitivity analysis
Assuming that the criteria where an “unknown” was scored in the van Tulder et al. (Citation1997, Citation2003) score had actually been met, results in assigning all the low-quality studies to the high quality group. This only has an effect on the “best evidence synthesis”. For comparison 1, this would not change the conclusions since the PCL removal group, where the only differences were found, was a subgroup of the total PCL retention group. For comparison 2, this would change the conclusion because the improvement in range of motion in the study of Maruyama et al. (Citation2004) would gain more weight for the conclusions.
Implications for research
Total knee arthroplasty is a successful procedure. To improve an already successful procedure, the small details should be examined. We believe that the treatment of the PCL during TKA is one of these details. Thus, choices regarding retention, release or removal of the PCL should be thoroughly investigated in adequate trials. We have summarized our findings in for those wishing to pursue a randomized trial on this topic.
Table 6. Methodological aspects that need attention in the process of design and reporting of randomized controlled trials
Implications for practice
Based on this review, we cannot make a recommendation between retention or removal of the PCL, or between retention and removal accompanied by a PS design. The number of studies that have been found to support any conclusions on such comparisons are too limited, and less than half of them are of high quality. The technique of PCL balancing is very demanding and complicated, and was unfortunately not described carefully in the trials selected. Techniques for improvement of balancing of the PCL during total knee arthroplasty are still under development, as this is a new area of focus within TKA research. When these techniques have been developed and described in sufficient detail, renewed scientific experiments in patient series should be undertaken.
We wish to thank Dr R. Schrijnemakers, librarian at Sint Maartenskliniek Nijmegen, for assisting in the searches and arranging reprints, and also the Dutch Cochrane Center for assisting us with additional searches.
No competing interests declared.
- Becker M W, Insall J N, Faris P M. Bilateral total knee arthroplasty. One cruciate retaining and one cruciate substituting. Clin Orthop 1991, 271: 122–4
- Cash R M, Gonzalez M H, Garst J, Barmada R, Stern S H. Proprioception after arthroplasty: role of the posterior cruciate ligament. Clin Orthop 1996, 331: 172–8
- Catani F, Leardini A, Ensini A, Cucca G, Bragonzoni L, Toksvig-Larsen S, Giannini S. The stability of the cemented tibial component of total knee arthroplasty: posterior cruciate-retaining versus posterior-stabilized design. J Arthroplasty 2004; 6(19)775–82
- Clark C R, Rorabeck C H, MacDonald S, MacDonald D, Swafford J, Cleland D. Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop 2001, 392: 208–12
- Cope M R, O'Brien B S, Nanu A M. The influence of the posterior cruciate ligament in the maintenance of joint line in primary total knee arthroplasty: a radiologic study. J Arthroplasty 2002; 2(17)206–8
- Dennis D A, Komistek R D, Colwell C E, Jr., Ranawat C S, Scott R D, Thornhill T S, Lapp M A. In vivo anteroposterior femorotibial translation of total knee arthroplasty: A multicenter analysis. Clin Orthop 1998, 356: 47–57
- Dorr L D, Ochsner J L, Gronley J, Perry J. Functional comparison of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. Clin Orthop 1988, 236: 36–43
- Emodi G J, Callaghan J J, Pedersen D R, Brown T D. Posterior cruciate ligament function following total knee arthroplasty: the effect of joint line elevation. Iowa Orthop J 1999; 19: 82–92
- Fleiss J L. The statistical basis of meta-analysis. Stat Methods Med Res 1993; 2: 121–45
- Freeman M A, Pinskerova V. The movement of the knee studied by magnetic resonance imaging. Clin Orthop 2003, 410: 35–43
- Hirsch H S, Lotke P A, Morrison L D. The posterior cruciate ligament in total knee surgery. Save, sacrifice, or substitute?. Clin Orthop 1994, 309: 64–8
- Hogervorst T, Brand R A. Mechanoreceptors in joint func-tion. J Bone Joint Surg (Am) 1998; 9(80)1365–78
- Ishii Y, Terajima K, Koga Y, Takahashi H E, Bechtold J E, Gustilo R B. Gait analysis after total knee arthroplasty. Comparison of posterior cruciate retention and substitution. J Orthop Sci 1998; 3(6)310–7
- Jadad A R, Moore R A, Carroll D, Jenkinson C, Reynolds D J, Gavaghan D J, McQuay H J. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Control Clin Trials 1996; 17(1)1–12
- Komistek R D, Dennis D A, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop 2003, 410: 69–81
- Laskin R S. The Insall Award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop 1996, 331: 29–34
- Laskin R S. Cemented total knee replacement in patients with osteoarthritis: A five-year follow-up study using a prosthesis allowing both retention and resection of the posterior cruciate ligament. Knee 1997; 4(1)1–6
- Lombardi A V, Mallory T H, Fada R A, Hartman J F, Capps S G, Kefauver C A, Adams J B. An algorithm for the posterior cruciate ligament in total knee arthroplasty. Clin Orthop 2001, 392: 75–87
- Mahoney O M, Noble P C, Rhoads D D, Alexander J W, Tullos H S. Posterior cruciate function following total knee arthroplasty. A biomechanical study. J Arthroplasty 1994; 9(6)569–78
- Maloney W J, Schurman D J. The effects of implant design on range of motion after total knee arthroplasty. Total condylar versus posterior stabilized total condylar designs. Clin Orthop 1992, 278: 147–52
- Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty 2004; 19(3)349–53
- Migaud H, Tirveilliot F. Preservation, resection or sub-stitution of the posterior cruciate ligament in total knee replacement. EFORT 2002; 176–84
- Mihalko W M, Krackow K A. Posterior cruciate ligament effects on the flexion space in total knee arthroplasty. Clin Orthop 1999, 360: 243–50
- Misra A N, Hussain M R, Fiddian N J, Newton G. The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg (Br) 2003; 85(3)389–92
- Morberg P, Chapman-Sheath P, Morris P, Cain S, Walsh W R. The function of the posterior cruciate ligament in an anteroposterior-gliding rotating platform total knee arthroplasty. J Arthroplasty 2002; 17(4)484–9
- Most E, Zayontz S, Li G, Otterberg E, Sabbag K, Rubash H E. Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop 2003, 410: 101–13
- Nozaki H, Banks S A, Suguro T, Hodge W A. Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop 2002, 404: 308–14
- Pagnano M W, Hanssen A D, Lewallen D G, Stuart M J. Flexion instability after primary posterior cruciate retaining total knee arthroplasty. Clin Orthop 1998, 356: 39–46
- Pellengahr C, Jansson V, Durr H R, Refior H J. The importance of the sagittal stability in knee arthroplasty. An analysis in 76 cases with unconstrained knee resurfacing. Zeitschrift fur Orthopadie und Ihre Grenzgebiete 1999; 137(4)330–3
- Pereira D S, Jaffe F F, Ortiguera C. Posterior cruciate ligament-sparing versus posterior cruciate ligament-sacrificing arthroplasty. Functional results using the same prosthesis. J Arthroplasty 1998; 13(2)138–44
- Shoji H, Wolf A, Packard S, Yoshino S. Cruciate retained and excised total knee arthroplasty. A comparative study in patients with bilateral total knee arthroplasty. Clin Orthop 1994, 305: 218–22
- Simmons S, Lephart S, Rubash H, Borsa P, Barrack R L. Proprioception following total knee arthroplasty with and without the posterior cruciate ligament. J Arthroplasty 1996; 11(7)763–8
- Stiehl J B, Voorhorst P E, Keblish P, Sorrells R B. Comparison of range of motion after posterior cruciate ligament retention or sacrifice with a mobile bearing total knee arthroplasty. Am J Knee Surg 1997; 10(4)216–20
- Straw R, Kulkarni S, Attfield S, Wilton T J. Posterior cruciate ligament at total knee replacement. Essential, beneficial or a hindrance? J Bone Joint Surg (Br) 2003; 85(5)671–4
- Swanik C B, Lephart S M, Rubash H E. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg (Am) 2004; 86(2)328–34
- Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty 2002; 17(7)813–9
- Udomkiat P, Meng B J, Dorr L D, Wan Z. Functional comparison of posterior cruciate retention and substitution knee replacement. Clin Orthop 2000, 378: 192–201
- van Tulder M W, Assendelft W J, Koes B W, Bouter L M. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine 1997; 22(20)2323–30
- van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003; 28(12)1290–9
- Vinciguerra B, Pascarel X, Honton J L. Results of total knee prostheses with or without preservation of the posterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot 1994; 80(7)620–5
- Waslewski G L, Marson B M, Benjamin J B. Early, incapacitating instability of posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty 1998; 13(7)763–7