Abstract
Background Controversy still exists as to whether to mount the tibial bearing on a metal baseplate or not. Furthermore, the tibial component can be either horizontally or completely cemented. We evaluated metal backing versus all-polyethylene using horizontal cementing technique.
Patients and methods We randomized 40 patients with knee arthrosis (40 knees) to 2 groups: cemented total knee arthroplasty (AGC, Biomet) using either all-polyethylene (AP) or metal-backed (MB) tibial compo-nents (n = 20 for each group). All tibial implants had a total thickness of 8 mm. We used proximal cement-ing, including only the horizontal part of the tibia with avoidance of the stem-bone interface.
Results The positioning of the implants, as judged by the HKA angle, showed an average neutral alignment in both groups. Preoperatively and after 2 years, there was no statistically significant difference between the HSS scores in both groups (p = 0.6 and 0.4). After 2 years, the metal-backed components had rotated more around the longitudinal axis, median 0.5° vs. 0.2° (internal or exter-nal rotation, p = 0.002), and showed increased maximum total point motion, median 1.0 vs. 0.4 mm (maximum migration or MTPM, p = 0.003).
Interpretation Our study indicates that better fixation can be obtained with the all-polyethylene design if proximally cemented thin components are used.
▪
Until the late 1980s, fixation failure of the tibial component was considered to be the major reason for revision in total knee arthroplasty (TKA). This could be attributed to poor cementing, malalign-ment, and, in some cases, design problems related to component size, degree of constraint and lack of sufficiently accurate surgical instruments. TKAs of early design were always all-polyethylene (AP) single plateau. Excellent 10–20 year survival rates of 91–98% (Ranawat et al. Citation1993, Gill et al. Citation1999) of the gold standard “total condylar” (AP-mono-bloc until 1984) and its derivates were difficult to achieve with AP plateaus, which were proposed to inferiorly accommodate and improperly distribute stresses at the interfaces (Bartel et al. Citation1982).
In the 1980s, calculations based on finite ele-ment analysis indicated that metal backing of the tibial component would improve the distribution of forces and pressure between the implant and the cement, and thereby theoretically reduce the risk of clinical loosening (Bartel et al. Citation1982, Citation1986).
This concept spread rapidly to almost every design. The popularity of metal backing was enhanced because it opened the way for modular designs. At that time, the potential negative proper-ties of these constructs—such as backside wear and wear of thin polyethylene inlays—were unknown or were disregarded. Modular polyethylene inserts still dominate the market. With the thinnest inserts, there is a risk of accelerated plastic damage, which may eventually result in need for revision, including the femoral component (Bert et al. Citation1998).
The excellent results reported with the total condylar design were based on an all-polyethyl-ene monobloc tibial component (Insall et al. Citation1983, Vince et al. Citation1989), which justifies further studies of this concept. Manufacture of these designs is cheaper, which is another reason for the regained interest in all-polyethylene components (Rand Citation1993, Adalberth et al. Citation2000, Hyldahl et al. Citation2001, Udomkiat et al. Citation2001).
We compared two stemmed monobloc tibial com-ponents, one all-polyethylene and one with metal backing, inserted with the proximal cementing technique. All implants had the same design oth-erwise and equal thickness (8 mm). We used radio-stereometric analysis (RSA) to measure migration over 2 years postoperatively. Our hypothesis was that the model with metal backing would improve fixation, in accordance with reported biomechani-cal results.
Patients and methods
Between 1995 and 1998, 80 knees (77 patients) with knee arthrosis were operated on at St. Göran's Hospital, Stockholm, using the AGC total knee prosthesis (Anatomic Graduated Component; Biomet, Warsaw, IN). Patients with grade III–V primary arthrosis (Ahlbäck Citation1968) who were on our waiting list for TKA were included. Bilateral dis-ease with or without surgery of the other knee was accepted. No age or weight limit was used. Patients with previous meniscectomy were included, but no other type of previous surgery was accepted. The patients were entered consecutively after giving informed consent. Immediately before surgery, the knees were allocated to one or other group using the minimization method (Pocock Citation1983). The groups were (1) only proximal cementing leaving the stem uncemented (this study) or (2) proximal cementing with cement around the stem (see part 2). Within each stratum, the choice of component—all-poly-ethylene (AP) or metal-backed (MB)—was allo-cated randomly. To further minimize any influence of confounders, the patients were also stratified according to age (< 65 years, ≥ 65 years), body weight (< 75 kg, ≥ 75 kg), degree of knee defor-mity (< 10°, ≥ 10°), and gender. 40 patients (40 knees; 20 AP and 20 MB), all operated with proxi-mal cementing, constituted the study group for the present paper (). In 4 patients with metal-backed components, a sufficient number of tanta-lum markers could not be visualized at the RSA examinations, leaving 16 MB and 20 AP implants to be studied. Exclusion of these patients did not change the patient demographics statistically. The study was approved by the Ethics Committee of Karolinska Institute, Stockholm.
Table 1. Patient profile with APHC (all-polyethylene horizontally cemented components) vs. MBHC (metalbacked horizontally cemented components) after randomization. MBHC/RSA denotes patient profile in group included in RSA after exclusions
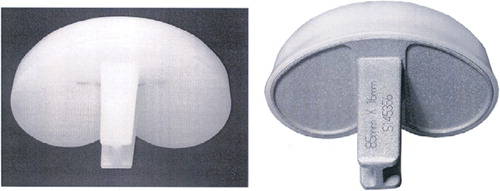
Prosthesis
The AGC is a minimally constrained, posterior cruciate retaining prosthesis. It is well-documented and has a good long-term survival rate (Emerson et al. Citation2000). The tibial component (AP and MB) is a one-piece (nonmodular), press-moulded poly-ethylene type using resin GUR 1900. Sterilization was performed by gamma irradiation in argon. In metal-backed tibial components, the tray is 3.7 mm thick and made of cobalt-chromium alloy. The polyethylene is 3.8 mm at its thinnest part, whereas the all-polyethylene component has a minimum thickness of 8 mm.
The articulating surface is flat on flat in the coro-nal plane and has a slight anterior lip in the sagittal plane. The underside of the surface has a periph-eral rim, which may contribute to increase cement compression during the insertion. Typically, the horizontal cement mantle becomes 1–2 mm wide with both the AP and the MB design. The stem is H-shaped in cross section and slightly conical. The stem is proportionally longer for the larger compo-nent sizes (range 32–48 mm). The femoral com-ponent is made of cobalt-chromium alloy and any femur fits any tibial component size ().
Operation
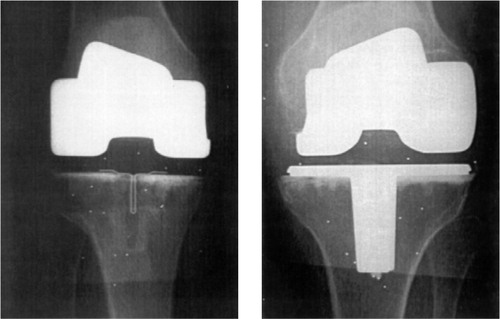
All operations were done using epidural anesthe-sia, tourniquet, (300–350 mm Hg), straight ante-rior skin incision, and medial arthrotomy. We used the manufacturer's standard instrumentation with intramedullary femoral and extramedullary tibial guide, respectively. Size of prosthesis was chosen to obtain optimal coverage of the cut tibial surface. Before cement application with the press-fit stem, an H-shaped punch was used, thus creating a press-fit cancellous cavity in the proximal tibia. All bone cuts were cleaned by pulse-lavage and dried before application of cement. Cement was applied to the horizontal surface of the tibia, avoiding the stem cavity, and on the cut surface of the femur. Both components were cemented in a one-stage proce-dure using a cement gun and vacuum-mixed bone cement (Palacos cum gentamicin, Schering Corp., Labo, Belgium). The cement was allowed to cure with the leg in full extension. No patellar resurfac-ing was used (). Two surgeons with long experience of total knee arthroplasty performed or participated during the surgical procedures. Drainage and epidural anesthesia-catheter were withdrawn within 24 h and full weight bearing (as much as could be tolerated, according to level of pain) was started on the postoperative day.
Clinical and radiographic evaluation
Clinical assessment was performed preoperatively and after 2 years using the Hospital for Special Surgery (HSS) score (Insall et al.Citation1976). The Hip-Knee-Ankle angle (HKA) (Jeffery et al. Citation1991) was determined 2 months postoperatively.
Pre-and postoperative radiographs included anterior-posterior and lateral short weight-bear-ing radiographs. Merchant patellar view was only exposed postoperatively. We classified the radio-graphs as satisfactory if there was no obvious notching on the femur, no mismatching between the proximal tibia and the tibial component size, and no defects in the cement mantle. Tilting of components was only measured in cases where the observer classified component position as unsat-isfactory. An independent radiologist who was blinded to the study evaluated all radiographs.
Radiostereometric analysis
During the operation, we prepared the skeleton and prosthesis for RSA by inserting 6–9 tantalum balls (diameter 0.8 mm) in the proximal tibial metaphy-sis, 6 balls (0.8 and 0.5 mm) in the polyethylene tray, and another marker into the tip of the polyeth-ylene stem (AP group only). The manufacturer had inserted a corresponding marker at the end of the metal-backed stem. We used a biplanar technique (Kärrholm Citation1989, Selvik Citation1989, Nilsson and Kär-rholm Citation1993). RSA examinations were done 3–4 days postoperatively and after 3, 12 and 24 months. The postoperative examination was used as refer-ence for the position of the laboratory coordinate system and as starting position for subsequent measurements of migration. Accordingly, transla-tions and rotations are presented as migration (mm and degrees, respectively) during the first 3, 12 and 24 months postoperatively. The stereoradiographs were scanned and the resultant digitized images were measured and evaluated using the UmRSA software (RSA Biomedical, Umeå, Sweden).
We evaluated the rotations and selected param-eters representing translations of the tibial compo-nent. The rotations around the transverse (x-axis, anterior-posterior tilt), longitudinal (y-axis, inter-nal-external rotation) and sagittal (z-axis, varus-valgus tilt) axes were evaluated in terms of signed and absolute values (indicating direction and disre-garding direction, respectively).
We evaluated translations of standardized posi-tions on the tibial tray according to Kärrholm (Citation1989) and Nilsson and Kärrholm (Citation1993). We chose to use maximum subsidence and maximum lift-off corresponding to any of the 8 standardized posi-tions which displayed the most pronounced distal and proximal displacements, respectively. In addi-tion, we evaluated the maximum total point motion (MTPM) corresponding to the vector length of the translation of the point on the tibial component exhibiting the most pronounced translation (irre-spective of direction). The MTPM between 1 and 2 years has been shown to be of prognostic value (Ryd et al. Citation1995). Since the translation may change direction over time, this parameter was calculated using the 1-year examination as reference. Com-ponents with an MTPM of < 0.2 mm during the second year were classified as “stable”, while an MTPM of < 0.2 mm was classified as “continuous migration”, according to the definition of Ryd et al. (Citation1995).
In 32 of the 80 knees, we assessed the precision of RSA for knee replacements in our set-up by double examinations with an interval of about 10 min (). These values are on a par with other set-ups in other departments. The stability of indi-vidual markers within each segment is essential for accurate radiostereometric calculations. In RSA, the degree of marker stability is expressed in the mean error (m.e.) of rigid body fitting. High values indicate marker instability. The limit for acceptance was set to 0.25 mm. No examination exceeded this value. The condition number reflects scattering of the markers; the smaller the value, the better the scatter. In our study, all examinations were based on condition numbers less than 100—except on two occasions with values of 160 and 139 (follow-up of 12 months in the MB group).
Table 2. Precision in actual set-up
Statistics
We used non-parametric tests since the migration data were not normally distributed. Kruskal-Wallis analysis was performed on the complete material, including all 80 knees and at each follow-up occa-sion. If lack of homogeneity was indicated at the probability level of 90% or more (p < 0.1), pair-wise testing focusing on the two subgroups with proximally cemented components was done for the purpose of the present evaluation. We considered p-values of < 0.05 to be statistically significant.
We used multiple regression analysis to study any influence of age and weight on rotation around the cardinal axes, subsidence, lift-off and MTPM at the 2-year follow-up. The Mann-Whitney U-test was used to evaluate any differences in migration between men and women and between surgeons.
Results
Clinical results
All patients attended the 2-year follow-up. The median HSS scores increased from 59 (37–83) to 88 (70–100) in the AP group and from 62 (37–72) to 88 (76–98) in the MB group without statistically significant differences between the two groups (p = 0.65 and 0.43, preoperatively and at follow-up, respectively; Mann-Whitney U-test). There were no major complications, and no revisions. One 80-year-old woman in the AP group had an HSS score of 53 at 2 years, indicating poor outcome. The operated knee was painful during weight bear-ing and she had severe arthrosis in her other knee. RSA showed that the tibial component was “stable” during the second year (MTPM = 0.07).
Radiographic result
All prosthetic components were classified as satis-factory on conventional radiographs. The median HKA 3 months postoperatively was 180° (167–187) in the AP group and 179° (174–184) in the MB group (median, range), indicating an overall neutral leg alignment, and no statistically significant difference was observed between the groups. Grouping values are presented in . 1 patient in the AP group had an HKA of 167° (i.e. 13° varus). At 2 years, the HSS scores amounted to 88 and the MTPM in the second year was zero.
Table 3. HKA (in degrees) 3 months postoperatively, for the separate groups. Figures denote number of individuals within each HKA interval
Radiostereometry
Since the metal tray and the stem act as radio-graphic “shadows”, we had problems in detecting a sufficient number of tantalum balls in both expo-sures in the MB group. 4 knees in the MB group were therefore excluded, while another 3 knees were excluded on a separate occasion for similar reasons. All AP knees could be analyzed. On all occasions, there was a tendency for higher rotation of the MB than of the AP components. A statisti-cally significant difference was found at 3 months concerning anterior/posterior and varus/valgus tilt in favor of the AP group. Increased internal/exter-nal rotation in the MB group was found on all 3 follow-up occasions (3, 12 and 24 months) (). In the AP group, the direction of rotation was evenly distributed around zero. In the MB group, there was a tendency for internal rotation and ante-rior tilt of the components.
Table 4. Rotations along the 3 cardinal axes. Figures denote degrees
On all follow-up occasions, the metal-backed components also demonstrated increased MTPM (). There was no difference in maximum subsidence, but the metal-backed components showed more lift-off at 3 months (p = 0.001) ().
Figure 3. Box-plot illustrating subsidence of components in all-polyethylene, horizontally cemented (APHC) and metal-backed, horizontally cemented (MBHC) groups. There were no statistically significant differences. The line within the box denotes the median, the box represents the 25–75% range, and the whiskers represent non-outlier min and max. Extremes are marked “♦”.
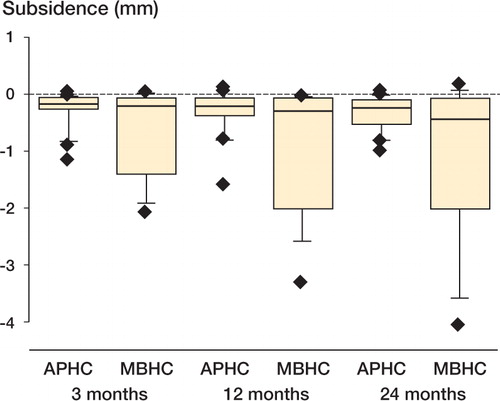
Table 5. Maximal total point motion (MTPM) in mm. Values are median (range)
Age, weight, sex or identity of the surgeon had no influence on the degree of micromotion recorded. In the MB group, 1 patient had an MTPM of 2.5 mm and a maximal inward rotation of 8.5°at 2 years, but the HSS score was 90 at 2 years. 2 other patients had an MTPM in the second year of 1.9 and 1.4 mm, respectively, and rotations of about 2–3.5° around all three axis. The HSS scores were 90 and 98. To date, none of these patients have been scheduled for revision. According to the definition of Ryd et al. (Citation1995), 8 of 13 components in the MB group and 5 of 20 in the AP group could be classified as “continuous migration” during the second year. There was no statistically significant difference between the groups (Fischer's exact test, p = 0.07) (). 3 knees in the MB-RSA group could not be classified due to missing MTPM at either the 1- or 2-year examination.
Discussion
All patients in this study had the same diagnosis and were operated with the same cementing tech-nique. They received components of the same thickness and of the same implant design. Even so, MB components migrated more than AP com-ponents, especially when measured as maximum migration regardless of direction (MTPM) and internal/external rotation.
We used the same RSA set-up and arrived at approximately the same degree of precision as Adalberth et al. (Citation2000), indicating that relevant comparisons could be done. Adalberth et al. (Citation2000) performed a similar study comparing proximally cemented all-polyethylene and metal-backed AGC TKAs. They found a “tendency” to higher MTPM and statistically significantly higher “lift-off” in the MB group, and concluded that the migration of AP implants was on a par with that of the MB implants. However, these authors compared com-ponents of different thickness, with higher total component thickness in the MB group and thicker polyethylene in the AP group. This can be expected to influence the results, since the influence of thick-ness becomes less with increasing height of the implant (Burstein Citation1990, Seki et al. Citation1998). Equal biomechanical rigidity of AP and MB is reached at a height of about 13 mm (Burstein Citation1990). Thus, the influence of metal backing on the fixation of the implant can be expected to be most pronounced when components thinner than 13 mm are used. Optimal comparison can be expected when the tibial components used are of equal height.
We believe that our findings reflect different rigidity of the tibial components, as proposed by Murase and co-workers (Citation1983). They performed an in-vitro evaluation of cemented all-polyethylene components with 3- and 6-cm-long stems. They found proximal bone stress reduction when stems were used. In a corresponding series of metal-backed tibial components, higher proximal stress reduction was found due to the cemented stem. This harmonizes with the “teeter-totter” effect. Using metal-backed trays, peripheral compressive load on one side will induce tensile forces on the opposite side due to the stiffness of the implant (Bartel et al. Citation1982). Adalberth et al. (Citation2000) found significantly more lift-off using metal-backed tibial components. We detected such a difference at 3 months. Exclusion of the stem from the cement mantle might imply that the metal tray has less resistance to eccentric loading.
Previous clinical studies comparing AP with MB have not been consistent regarding the optimum choice (Apel et al. Citation1991, Rand Citation1993, Adalberth et al. Citation2000, Udomkiat et al. Citation2001). The reason for this is not clear, but the presence of confounding fac-tors and inclusion of various thicknesses of tibial components could be of importance. As long as AP designs perform as well as MB designs, the cost speaks in favor of the former. In the past, many authors have concluded that AP functions as well as MB in “low demand” patients (L'Insalata et al. Citation1992, Rand Citation1993). Important arguments for AP are simplicity, thicker polyethylene with higher resistance to wear, absence of back-side wear and avoidance of mechanical interlocking problems. Age and activity level do not affect any of these arguments. The argument that a modular insert can be exchanged more easily will lose its importance if modularity in itself introduces new, more severe hazards.
Hvid (Citation1988) showed that the strength of the metaphyseal tibial bone became reduced with increasing proximal bone resection. This observa-tion and the risk of future loosening and revision favor minimal bone resection and the use of thin tibial components. Although the metal backing was developed to offer a stronger baseplate and prevent deformation of the polyethylene, several authors found that thin plastic remained a cause of failure despite the presence of metal backing (Engh et al. Citation1992, Wright et al. Citation1992). This means that a metal-backed component requires more bone resection than an all-polyethylene component to achieve equal polyethylene thickness.
During the past decade, the frequency of fixation failure of TKA has decreased, whereas wear and osteolysis have become increasingly common (Schai et al. Citation1998, Ewald et al. Citation1999). One reason for this could be that plastic inserts used on metal-backed designs frequently show micromotions, which may result in back-side wear (Wasielewski et al. Citation1997, Parks et al. Citation1998). Modularity has advantages, as it facilitates any revision procedure by offering a wide selection of implant designs in difficult cases. In the primary situation, the need for modularity can be debated. Bert et al. (Citation1998) described revisions of 62 modular TKAs due to tibial insert failure, where almost 90% required total revision due to significant scoring and/or damage of metal tray, and secondary damage to femur components. Babis et al. (Citation2002) reported a similar series of 56 insert exchanges where all other reasons for failure were excluded. Cumula-tive 6-year survival was 64% and these authors concluded that change of insert should only be per-formed with “caution”. Failure of an all-polyethyl-ene tibial component can be expected to cause less damage to the femoral component.
We studied a “flat on flat” arthroplasty design, which is considered not to be associated with opti-mal load transfer between the components. This “fact” seems to trace its origin from the classical studies of Bartel and co-workers (Bartel Citation1982), where infinite element analysis this single-plateau design showed low resistance to protect edge-loaded compressive forces to cancellous bone when varus/valgus tilt was applied. The only article we have found giving support for these in-vitro biome-chanical findings is the work by Faris et al. (Citation2003), where substantially inferior results comparing AP components (10 mm or thicker) with MB compo-nents were reported in a retrospective series lasting up to 10 years. This was a case series with a his-torical control group. 75% of failures were due to medial tibial collapse, the majority of tibial loosen-ing occurring within three years. The discrepancy between these results and ours is obvious.
We found that AP components had better fixation than MB tibial components using 8 mm pla-teaus and only proximal cementing. Based on these findings, we believe that AP components should be used more frequently, especially in the standard patient when thin components are to be inserted.
No competing interests declared.
- Adalberth G, Nilsson K G, Byström S, Kolstad K, Milbrink J. Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty. J Arthroplasty 2000; 15(6)783–92
- Ahlbäck S. Osteoarthrosis of the knee. A radiographic inves tigation. Acta Radiol Diagn (Stockh) 1968; 277: 7–72, (Suppl)
- Apel D M, Tozzi J M, Dorr L D. Clinical comparison of all- polyethylene and metal-backed tibial components in total knee arthroplasty. Clin Orthop 1991; 273: 243–52
- Babis G C, Trousdale R T, Morrey B F. The effectiveness of isolated tibial insert exchange in revision total knee arthroplasty. J Bone Joint Surg (Am) 2002; 84(1)64–8
- Bartel D L, Burstein A H, Santavicca E A, Insall J N. Perfor-mance of the tibial component in total knee replacement. J Bone Joint Surgery (Am) 1982; 64(7)1026–33
- Bartel D L, Bicknell V L, Wright T M. the effect of con-formity, thickness and material on stresses in ultrahigh molecular weight components for total joint replacement. J Bone Joint Surg (Am) 1986; 68: 1041–51
- Bert J M, Reuben J, Kelly F, Gross M, Elting J. The inci-dence of modular tibial polyethylene insert exchange in total knee arthroplasty when polyethylene failure occurs. J Arthroplasty 1998; 13(6)609–14
- Burstein A H. Wear factors in total knee replacement. Oral presentation, state of the art: total knee replacements. Laguna BeachCalifornia Oct 5th, 1990
- Emerson R, Higgins L, Head W. The AGC total knee pros-thesis at average 11 years. J Arthroplasty 2000; 15(4)418–23
- Engh G A, Dwyer K A, Hanes C K. Polyethylene wear of metal-backed tibial components in total and unicompartmental knee prosthesis. J Bone Joint Surg (Br) 1992; 74: 9–17
- Ewald F C, Wright R J, Poss R, Thomas W H, Mason M D. Kinematic total knee arthroplasty. A 10-to 14-year pro-spective follow up review. J Arthroplasty 1999; 14(4)473–80
- Faris P, Ritter M, Keating M, Meding J, Harty L. The AGC all-polyethylene tibial component: a ten year clinical evaluation. J Bone Joint Surg (Am) 2003; 85(3)489–93
- Gill G S, Joshi A B, Mills D M. Total condylar knee arthroplasty. 16-20 year results. Clin Orthop 1999; 367: 210–5
- Hvid I. Trabecular bone strenght at the knee. Clin Orthop 1988; 227: 210–21
- Hyldahl H C, Regner L, Carlsson L, Kärrholm J, Weiden-hielm L. Does metal backing improve fixation of tibial component in unicondylar knee prosthesis?. J Arthroplasty 2001; 16(2)174–9
- Insall J N, Ranawat C S, Aglietti P, Shine J. A comparison of four models of total knee replacement prosthesis. J Bone Joint Surg (Am) 1976; 58: 754–65
- Insall J N, Hood R W, Flawn K B, Sullivan D J. The total condylar knee prosthesis in gonarthrosis. A 5- to 9-year follw-up of the first 100 consecutive replacements. J Bone Joint Surg (Am) 1983; 65: 619–28
- Jeffery R S, Morris R W, Denham R A. Coronal alignment after total knee replacement. J Bone Joint Surg (Br) 1991; 73: 709–14
- Kärrholm J. Roentgen stereophotogrammetry. Review of orthopaedic applications. Acta Orthop Scand 1989; 60(4)491–503
- L'Inslata J, Stern S, Insall J. Total knee arthroplasty in elderly patients. J Arthroplasty 1992; 7(3)261–6
- Murase K, Crowninshield R, Pedersen D, Chang T-S. An analysis of tibial component design in total knee arthroplasty. J Biomechanics 1983; 16(1)13–22
- Nilsson K G, Kärrholm J. Increased varus-valgus tilting of screw-fixated knee-prosthesis. J Arthroplasty 1993; 8(5)529–40
- Parks N L, Engh G A, Topoleski L D, Emperado J. Modular tibial insert micromotion. A concern with contemporary knee implants. Clin Orthop 1998; 356: 10–5
- Pocock S J. Clinical trials. A practical approach. Wiley, Chichester 1983
- Ranawat C S, Flynn W F, Saddler S, Hansraj K, May-nard M J. Long-term results of the Total Condylar knee arthroplasty: a 15 year survivorship study. Clin Orthop 1993; 286: 94–102
- Rand J A. Comparison of metal-backed and all-polyeth-ylene tibial components in cruciate condylar total knee arthroplasty. J Arthroplasty 1993; 8(3)307–13
- Ryd L, Albrektsson B E, Carlsson L, Dansgård F, Herberts P, Lindstrand A, Regner L, Toksvik-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechan-ical loosening of knee prosthesis. J Bone Joint Surg (Br) 1995; 77(3)377–83
- Schai P A, Thornhill T S, Scott R D. Total knee arthroplasty with the PFC-system. Results at a minimum of ten years and survivorship analysis. J Bone Joint Surg (Br) 1998; 80(5)850–8
- Seki T, Tashiro T, Omori G. Does an all-polyethylene tibial component reduce impact force to distal femur, as com-pared to a metal-backed tibial component in total knee arthroplasty?. Trans Orthop Res Soc 1998; 44: 1105
- Selvik G. Roentgen stereophotogrammetry. A method for the study of kinematics of the skeleton system. Acta Orthop Scand 1989; 1–51, (Suppl 232)
- Udomkiat P, Dorr L, Long W. Matched pair analysis of All Polyethylene versus metal-backed tibial components. J Arthroplasty 2001; 16(6)689–96
- Wasielewski R C, Parks N, Williams I, Suprenant H, Collier J P, Engh G. Tibial insert undersurface as a contributing source of polyethylene wear debris. Clin Orthop 1997; 345: 53–9
- Vince K G, Insall J N, Kelly M A. The total condylar prosthe-sis.10-to 12-year results of a cemented knee prosthesis. J Bone Joint Surg (Br) 1989; 71(5)793–7
- Wright T M, Rimnac C M, Stulberg S D, Mintz L, Tsao A K, Klein R W, McCrae C. Wear of polyethylene in total knee replacements. Observations from retrieved PCA knee implants. Clin Orthop 1992; 276: 126–34