Abstract
Background Uncertainty exists as to whether metal backing (MB) of the tibial component is better than an all-polyethylene component (AP). This is valid for both horizontally and completely cemented components. We evaluated completely cemented MB vs. AP (Part 2).
Patients and methods In a randomized study, 39 patients (40 knees) with knee arthrosis were operated with cemented low-conforming total knee arthroplasty (AGC, Biomet) with a tibial component of uniform thickness (8 mm), cemented both beneath the tibial tray and around the stem. 20 patients had an all-polyethylene (AP) tibial component and 20 patients had an identical but metal-backed (MB) tibial component. We used clinical examination and radiostereometric analysis (RSA) to evaluate the hypothesis that MB improves component fixation. Fixation was evaluated using RSA up to 2 years after surgery. Clinical assessment was performed preoperatively and after 2 years using the Hospital for Special Surgeons (HSS) score.
Results We found no differences in micromotion, and no differences in clinical scores could be detected between the groups at any time point.
Interpretation Our findings indicate that there was equal initial fixation of the AP and MB stemmed monobloc components when they were cemented beneath the tibial plateau and around the stem.
▪
Metal-backing (MB) was initially introduced as a one-piece, non-modular component to improve longevity of fixation of tibial components. This assumption has never been proven in clinical research. The metal back also enabled modularity and the use of cementless fixation. There are, however, reasons to question its use. After some years of widespread use, problems relating to increased wear and insufficient locking mechanisms appeared, which have become an increasingly common cause of revision (Schai et al.Citation1998, Ewald et al. Citation1999). In primary cases the need for modularity may be limited, whereas this concept is often beneficial in cases of revision. Cementless fixation may be associated with long-term success (Whiteside Citation1994), but has also shown inferior results compared to cemented fixation (Duffy et al. Citation1998). Finally, a metal tray may increase the cost of the implant by up to 30% or more.
For the reasons given above, there has been renewed interest in the AP components. In matched-pair or retrospective studies, several authors have been unable to detect inferior clinical outcome when comparing AP components with their non-modular MB equivalents (Apel et al. Citation1991, L‘Insalata et al. Citation1992, Rand Citation1993). With modular MB design, such as Press Fit Condylar (PFC), one randomized study confirmed equal clinical outcome when comparing MB and AP components with a minimum of 3 years follow-up (Gioe and Bowman Citation2000). In another retrospective report (PFC) with a mean of 5 years follow-up, revisions due to osteolysis were found only in the MB group—amounting to 5% of the cases (Rodriguez et al. Citation2001).
In vitro, whether or not cement is used around the stem has been shown to infiuence the fixation differently depending on whether metal-backing is used (Reilly et al. Citation1982, Murase et al. Citation1983, Seki et al. Citation1997, Bert et al. Citation1998). Cement around the stem appears to improve fixation more in MB components than in AP components (Bert et al. Citation1998). This improvement would be achieved at the expense of proximal stress-shielding, which in itself might reduce longevity of the implant (Reilly et al. Citation1982, Murace et al. Citation1983, Lonner et al. Citation2001). Thus, in any comparison between MB and AP components, the cementing technique and the extent of the cement mantle should be similar. We are not, however, aware of any previous randomized evaluation comparing the fixation of completely cemented all-polyethylene stemmed non-modular tibial components with their metal-backed equivalents.
Comparison of horizontal cemented components (AP vs. MB) has been performed, using the same prosthesis (AGC) by Adalberth et al. (Citation2000) and Hyldahl et al. (Citation2005). Adalberth found fixation ”on par” but Hyldahl detected better fixation of AP components.
We used radiostereometric analysis (RSA; Selvik Citation1989) to compare the migration of all-polyethylene or metal-backed tibial components up to 2 years after operation, where the cement mantle also included the stem of the prosthesis.
Patients and methods
The set-up in this study was identical in all respects to that of a previous study (Hyldahl et al. Citation2005) except for one variable. The present study focused on the 2 groups of knees that were allocated completely cemented tibial components immediately before the operation: either all-polyethylene (APCC) or metal-backed MBCC), i.e. the stem was included in the cement mantle.
Consequently, there were 39 patients in the study group (40 knees, 1 operated bilaterally), all of whom received the 8mm thick tibial component—either APCC or MBCC (or both in the bilateral case) (). Thus, there were 20 knees in each group. 40 knees, 1 operated bilaterally, one side AP, the other MB.
Table 1. Patient profile with APCC (all-polyethylene completely cemented components) vs. MBCC (metal-backed completely cemented components) after randomization. MBCC/RSA denotes patient profile in group included in RSA after exclusions, see
The study was approved by the Ethics Committee of Karolinska Institute.
4 patients in the MBCC group could not be analyzed by RSA due to difficulties in visualizing sufficient numbers of tantalum markers in the tibial component radiographically. Reasons for exclusion are presented in . 1 patient in the APCC group could not be analyzed due to a missing post-operative RSA examination. There were no differences between the 2 groups in patient demographics, including or excluding patients with missing observations ().
Table 2. Patients in the MBCC group who were excluded from RSA. Patients are presented with their case letters in the series
Prosthesis
See Part 1 (Hyldahl et al. Citation2005).
Operation
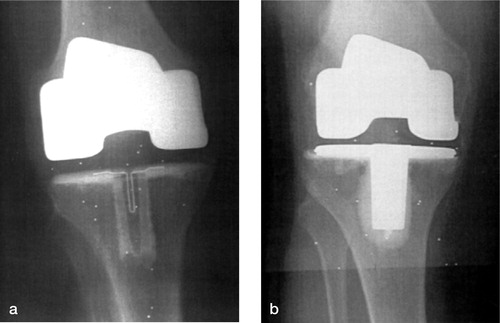
The method of operation was identical to that in Part 1 with one exception: before cement application a rectangular punch was used to create a cancellous cavity in the proximal tibia, and the cement gun was used for retrograde filling of the stem cavity. This was followed by application of cement to the horizontal tibial cut and the cut femoral surfaces. Postoperative radiographs using this complete cementing technique for AP and MB tibial components () are given in .
Figure 1. All-polyethylene (left) and metal-backed (right) tibial components of the AGC prosthesis. Both have non-modular, identical articulating surface and similar geometry.

Figure 2. Standard anterior postoperative radiographs of the a) all-polyethylene completely, cemented (APCC), and b) metal-backed, completely cemented (MBCC) tibial components.
Setup, examinations, calculations and precision all corresponded to those described by Hyldahl et al. (Citation2005). The limit for acceptance of mean error (m.e.) of rigid body fitting (marker instability) was the same (0.25 mm). No examination exceeded this value.
The condition number reflects scattering of the markers. The smaller the value, the better is the scattering—and hence the precision of the investigation. On three occasions we accepted values of 157, 156 and 153 (MB, prosthetic segment). All other values were less than 100.
Statistics
Statistical analysis was carried out as in Hyldahl et al. (Citation2005).
Results
Clinical result
There was no difference in preoperative HSS score and the HSS score at 2 years follow-up between the two groups: p = 0.7 and p = 0.2, respectively (Mann-Whitney U-test) ().
Table 3. HSS score (maximum 100 points). Values are median (range)
1 patient (APCC) was revised after 14 months because of patellofemoral pain, and received a cemented patellar component. The patient was not excluded since we felt that this operation did not affect prosthetic migration. No other revisions were performed within 2 years and no other complications requiring specific treatment occurred in any of the groups. No patients were lost to follow-up during the period of observation.
Radiographic results
The analysis of conventional radiographs showed that all prosthetic components were satisfactory, and we detected no technical errors or complications in the postoperative radiographs. The values of HKA angle indicated an overall neutral leg alignment and no differences were observed between the groups ().
Table 4. HKA (in degrees) for the separate groups. The figures denote the number of individuals within each HKA intervel
Radiostereometry
Rotations around the cardinal axes are given in . There were no statistical differences between the APCC and MBCC groups with regard to rotations, translations and MTPM at any time period. Regarding the direction of rotation, these were evenly spread around zero in the APCC group. In MBCC group, there was a tendency to anterior tilt of the components (11/14 at 12 months).
Table 5. Absolute rotations degrees and translations mm. median with range in parenthesis
According to the definition of Ryd et al. (Citation1995), 14 of 19 in the APCC group and 8 of 12 in the MBCC group could be defined as “stable” (i.e. MTPM < 0.2 mm during the second year). The difference was not statistically significant. The “continuously migrating implants” had the following MTPM values after 1–2 years: APCC: 0.25, 0.28, 0.3, 0.31 and 0.33; MBCC: 0.27, 0.40, 0.41 and 1.45. The three highest values in this latter group correspond to the individuals previously described in which relatively high values of condition number were accepted. That is, the measured markers were suboptimally separated, which may have influenced these recordings. The patient with the highest MTPM (1.45 mm) had a maximal rotation (anterior tilt) of 1.5° after 2 years. HSS score improved from 38 to 75 in this patient, who was 82 years of age. To date, there have been no signs of clinical failure or radiographic loosening.
Discussion
Early designs of TKA were consistently of the allpolyethylene monobloc type and some of these have shown excellent long-term results. The 10 year survival of the Total Condylar knee prosthesis has reached 90% or more (Ranawat et al. Citation1993, Gill et al. Citation1999) and is still considered to be the gold standard. Loosening of the tibial component was, however, a substantial problem in the early period of TKA. The AP design was put forward as a possible explanation and metal backing was introduced in the early 1980s as a solution to this problem. The arguments for this were mainly theoretical. Metal backing resulted in a more even load distribution, if the load was applied symmetrically (Bartel et al. Citation1982, Lewis et al. Citation1982, Reilly et Citation1982). However, asymmetrically or peripherally applied load resulted in increased tensile forces when metal-backed components were used. Such loading is more likely to occur in the clinical situation.
We have found only one randomized study com-paring completely cemented AP and MB tibial components (Gioe and Bowman Citation2000). With a minimum of 3 years follow-up, these authors eval-uated 111 AP and 102 MB press-fit condylar (PFC) prostheses and there were no differences regarding clinical or radiographic outcome. No aseptic loos-ening was observed. They included all diagnoses, but component thickness was not described. The conclusion was that a well-designed contemporary congruent AP component functions as well as a corresponding MB component over 3–5 years—and at lower cost.
There have been several retrospective studies comparing AP and MB tibial components, often biased chronologically; MB is often implanted later in the surgeon's experience with the same total knee (Apel et al. Citation1991, Rand Citation1993, Ritter et al. Citation1994). The Total Condylar knee changed to MB 1979, and more than 10 years later several authors reported retrospective comparisons before and after this change with no apparent differences regarding revision rate or loosening of the tibial component (Apel et al. Citation1991, L‘Insalata et al. Citation1992, Rand Citation1993). Apel concluded that “the use of AP in cemented TKA is recommended over MB because clinical results appear equivalent and the cost is lower”. In a retrospective comparison of modular MB and AP tibial components of the PFC pros-thesis with a minimum follow-up time of 5 years (243 knees, 175 patients), Rodriguez et al. (Citation2001) reported a 5% revision rate (6 knees) for metal-backed prostheses caused by ostoelysis and syno-vitis, but no revision in the AP group. The survival rate at 7 years was 96% ± 0.8% for AP and 75% ± 10% for MB. The authors stated that “modularity and MB was added to the PFC design to improve fixation. However, the superiority of the modular MB implants remains in question” (Rodriguez et al. Citation2001).
Udomkiat et al. (Citation2001) reported a matched-pair analysis of 96 knees (Apollo Knee System) with either an MB (AP-insert) monobloc tibial com-ponent or an AP monobloc tibial component with complete cemented mantle. Clinical and radio-graphic assessments up to 3 years postoperatively revealed no differences in clinical scores, self assessment or radiographic evaluation between the components. The authors concluded, as did L’Insalata et al. (Citation1992), that AP is preferable in the elderly because of a decreased risk of revision due to modularity. The restricted use of all-polyethyl-ene components to cover only the elderly popu-lation can be questioned. There is published data favoring AP regardless of age (Rodriguez et al. Citation2001) and Forster (Citation2003).
All these series evaluated congruent or semicon-gruent designs, and these designs are suggested to be optimal regarding AP tibial components. Based on these reports, AP and MB appear to allow equal fixation, whereas the AP component eliminates the risk of back-side wear—and at lower cost. Recently, Forster (Citation2003) reported a meta-analysis of 5,950 knees (16 articles) with survival analy-sis with minimum 5 years follow-up. Comparing posterior stabilized, non-stabilized, metal-backed or all-polyethylene cemented tibial components, the only design that showed significantly better survival was the non-stabilized all-polyethylene component.
We have found only one recent article reporting inferior results with AP tibial components com-pared with MB tibial components, both designs being completely cemented and followed for 10 years (Faris et al. Citation2003). This was a case series with a historic control group. AP tibial components at least 10 mm thick had a significantly higher revision rate regarding the AGC tibial component, basically due to medial collapse of the proximal cancellous tibia (3% revision, 14% medial collapse at 1 year). In most cases this was observed within 3 years postoperatively. The authors’hypothesis for this finding was that the AGC design, relatively low-conforming and “flat on flat” in the coronal plane, could not withstand edge loading.
Our findings after 2 years, using the same pros-thesis as in the series of Faris et al., but even thin-ner, are not in accordance with their finding of early failure of the AP component within 3 years. There are no published data supporting major changes regarding fixation during the third year after sur-gery. There might be explanations other than the composition of the component (in this case poly-ethylene) to explain their findings. AP failures have been reported in older series, for example Duch-eyne et al. (1978) who reported 7% failure at 2 years (UCI-prosthesis). In retrospect, the reasons for this were most probably multifactorial, such as use of thin components (5–7.5 mm), insufficient coverage of the cut tibial surface and perhaps an inferior cementing technique.
In our study, the comparatively small study population might imply a risk of type II error. If so, we may have failed to detect a superior initial fixation in AP components, which would not influ-ence our overall conclusion that all-polyethylene components are preferable—based on lower cost, use of thicker polyethylene and reduction of sur-face area, which may generate wear particles. On the other hand, if we have failed to detect better fixation using completely cemented MB-stemmed components, there would still be a need for stud-ies showing superior clinical results using a thin MB tibial component, which is a more expensive component with potential wear complications. We conclude that MB tibial components give no better fixation than AP tibial components when the components are completely cemented.
We have found better initial fixation of AP than MB when the components were only horizontally cemented (Hyldahl et al. Citation2005). Reason for this is unclear but we believe that it reflects different rigidity, metal vs. all-polyethylene. The more rigid MB, transforming asymmetric load throughout the entire component, needs a larger cement.bone contact area to resist clinically excentric load. AP, more elastic, may partly absorb such excentric forces without need of extra cement.
No competing interests declared.
- Adalberth G, Nilsson K G, Byström S, Kolstad K, Milbrink J. Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty. J Arthroplasty 2000; 15(6)783–92
- Apel D M, Tozzi J M, Dorr L D. Clinical comparison of all-polyethylene and metal-backed tibial components in total knee arthroplasty. Clin Orthop 1991, 273: 243–52
- Bartel D L, Burstein A H, Santavicca E A, Insall J N. Perfor-mance of the tibial component in total knee replacement. J Bone Joint Surg (Am) 1982; 64: 1026–33
- Bert J M, McShane M. Is it necessary to cement the tibial stem in cemented total knee arthroplasty?. Clin Orthop 1998, 356: 73–8
- Duffy G P, Berry D J, Rand J A. Cement versus cement-less fixation in total knee arhroplasty. Clin Orthop 1998, 356: 66–72
- Ewald F C, Wright R J, Poss R, Thomas W H, Mason M D, Sledge C B. Kinematic total knee arthroplasty. A 10- to 14-year prospective follow-up review. J Arthroplasty 1999; 14(4)473–80
- Faris P M, Ritter M A, Keating E M, Meding J B, Harty L D. The AGC all-polyethylene tibial component: a ten year clinical evaluation. J Bone Joint Surg (Am) 2003; 85(3)489–93
- Forster M C. Survival analysis of primary cemented total knee arthroplasty. J Arthroplast 2003; 18(3)265–70
- Gill G S, Joshi A B, Mills D M. Total condylar knee arthroplasty. 16-to 21-year result: Clin Orthop 1999, 367: 210–5
- Gioe T, Bowman K. A randomized comparison of all-poly-ethylene and metal-backed tibial components. Clin Orthop 2000, 380: 108–15
- Hyldahl H, Regnér L, Carlsson L, Kärrholm J, Weiden-hielm L. All-polyethylene vs. metal-backed tibial com-ponent in tota knee arthroplasty—a randomized RSA study comparing early fixation of horizontally and com-pletely cemented tibial components. Part 1. Horizontally cemented components: AP better fixated than MB. Acta Orthop 2005; 76: 769–77
- Lewis J L, Askew M J, Jaycox D P. A comparative evaluation of tibial components designs of total knee prostheses. J Bone Joint Surg (Am) 1982; 64(1)129–35
- L’Insalata J, Stern S, Insall J. Total knee arthroplast in elderly patients. J Arthroplast 1992; 7(39)261–6
- Lonner J H, Klotz M, Levitz C, Lotke P A. Changes in bone density after total cemented knee arthroplasty. J Arthroplasty 2001; 16(1)107–11
- Murase K, Roy D, Crowninshield R, Pedersen D, Chang T-S. An analysis of tibial component design in total knee arthroplasty. J Biomechanics 1983; 1: 13–22
- Ranawat C S, Flynn W F, Jr, Saddler S, Hansraj K K, May-nard M J. Long term results of the total condylar knee Arthroplasty. A 15-year survivorship study. Clin Orthop 1993, 286: 94–102
- Rand J A. Comparison of metal-backed and all-polyeth-ylene tibial components in cruciate condylar total knee arthroplasty. J Arthroplasty 1993; 8(3)307–13
- Reilly D, Walker P S, Ben D M, Ewald F C. Effects of tibial components on loadtransfer in the upper tibia. Clin Orthop 1982, 165: 273–82
- Ritter M A, Faris P M, Keating E M, Meading J B. Long term survival analysis of a posterior cruciate-retaining total condylar knee arthroplasty. Clin Orthop 1994, 309: 136–45
- Rodriguez J A, Norberto B, Rasquina V, Ranawat C S. Metal-backed and All-polyethylen tibial components in total knee replacement. Clin Orthop 2001, 392: 174–83
- Ryd L, Albrektsson B E, Carlsson L, Dansgård F, Herberts P, Lindstrand A, Regner L, Toksvik-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechan-ical loosening of knee prosthesis. J Bone Joint Surg (Br) 1995; 77(3)377–83
- Schai P A, Thornhill T S, Scott R D. Total knee arthroplasty with the PFC system. Results at a minimum of ten years and survivorship analysis. J Bone Joint Surg (Br) 1998; 80: 850–8
- Seki T, Bourgeault C, Chareancholvanich A K, Lew W, Bechtold J E, Gustilo R B. Does a central stem affect bone strain and the stability of a cemented tibial tray in primary revision TKA?. Trans Orthop Res Soc 1997; 22: 635
- Selvik G. Roentgen stereophotogrammetry. A method for the study of kinematics of the skeleton system. Acta Orthop Scand (Suppl 232) 1989; 1–51
- Udomkiat P, Dorr L, Long W. Matched pair analysis of All Polyethylene versus metal-backed tibial components. J Arthroplasty 2001; 16(6)689–96
- Whiteside L A. Cementless total knee replacement. Nine to 11 years result and 10-year survivorshipanalysis. Clin Orthop 1994, 309: 185–92
