Abstract
Background Various studies have reported good long-term results using femoral stems with either smooth or rough surfaces. In this retrospective cross-sectional survivorship study, we reviewed the 10-year results of 51 bilateral staged cemented total hip arthroplasties using the Harvard or the Charnley femoral stems—which have almost similar geometry but a different surface finish.
Methods 51 patients were reviewed at median interval of 10 (Harvard group) and 11 years (Charnley group) after the primary operation. We evaluated cement mantle thickness, alignment of the components, presence of radiolucent lines, and aseptic loosening. Kaplan-Meier analysis was performed to calculate the survival rate using various endpoints.
Results 8 hips in the Harvard group were revised for aseptic loosening of thefemoral component at a median interval of 6.3 years after the primary procedure. 3 hips in the Charnley group were revised for aseptic loosening of the femoral and acetabular components between 10 and 11 years after the primary procedure. The 10-year survival rate for the femoral component using revision surgery for aseptic loosening as an endpoint was 80% (95% CI: 31–42) and 95% (95% CI: 44–47) in the Harvard and the Charnley group, respectively. Cox regression analysis did not reveal any statistically significant effect of various radiographical parameters on the survival rate (p < 0.05).
Interpretation Our results demonstrate that in the group of patients studied, the femoral stem component with the matt surface finish had less satisfactory 10-year survival than the femoral stem of similar design which had a smooth surface finish.
▪
Aseptic loosening is an important cause of revision surgery in total hip arthroplasty (THA) (Ebramzadeh et al. Citation1994). Various changes in the design have been tried to improve the long-term survival of the cemented femoral component. These alterations include size of the stem, design changes (e.g. collars, flanges, grooves), surface finish, and properties of the materials used. (Sarmiento et al. Citation1988). The original Charnley femoral stem has undergone several changes. Some studies have reported rates of aseptic loosening that are higher with the second-generation Charnley femoral stem than with the first generation (Dall et al. Citation1993). A change in the original Exeter femoral surface from a smooth, polished surface to a matt finish surface led to increased rates of aseptic failure (Fowler et al. Citation1988, Rockbom and Olsson Citation1993).
Patient characteristics such as weight, level of physical activity, age and sex can affect the final outcome of the femoral stem (Harris Citation1998). The study of patients who have had bilateral staged THA using a different prosthesis on either side can control for the effect of these patient-related variables. There have been studies reporting good results using femoral stems with either smooth surface (Collis and Mohler Citation1998, Citation2002, Howie et al. Citation1998, Hinrichs et al. Citation2003) or rough surface (Wroblewski and Siney Citation1992, Malchau et al. Citation1993, Sanchez-Sotelo et al. Citation2002). In this study, we reviewed the results of bilateral staged cemented THA with almost similar geometryusing a smooth-surface femoral stem on one side and a femoral stem with matt finish on the other side.
Patients and methods
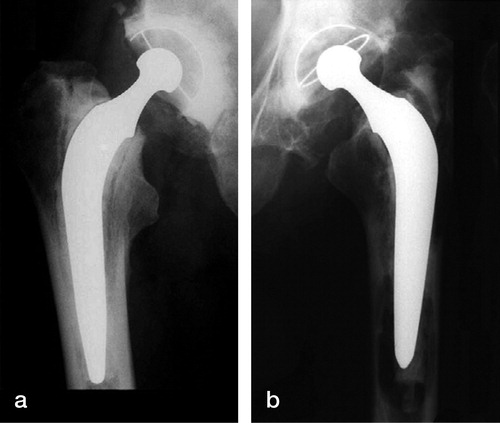
We retrospectively reviewed 51 bilaterally cemented THAs with a smooth-surface-finish Charnley design (Ra 0.8 μm) on the one side and matt-surface-finish Harvard design (Ra 2.2 μm) on the other. Both stems were made of stainless steel. The Harvard femoral stem (Harvard Healthcare Ltd., Wakefield, West Yorkshire, UK) was used in our hospital between 1990–1994. Of 51 THAs performed using the Charnley femoral stem (DePuy, Leeds, UK), 40 were done between 1987 and 1998 and 11 between 1978 and 1987. Three patients, in whom one of the prostheses was used for revision of a failed THA, were excluded from the study. The mean ages in the Charnley and the Harvard group at the time of the index procedure were 66 (51–81) years and 69 (56–82) years, respectively.
In all but three patients, the preoperative diagnosis was primary osteoarthritis. As the cases included in the study were performed between 1978 and 1994, the procedures had been performed by a number of surgeons (consultants and registrars), but all operations were performed at the same hospital. The anterolateral approach was used in 45 hips in the Harvard group and in 37 hips in the Charnley group. In the Charnley group, 8 THAs were performed using the transtrochanteric approach. Three procedures were performed using the posterior approach in both groups. Second-generation cementing techniques were used in almost all of the procedures except those carried out before 1987 (11 Charnley THAs). A femoral stem with 22.25-mm head was used in all patients. A cemented Charnley acetabular component of similar design was used in both groups.
We performed a review of the medical notes and radiographs of all patients. Patients for whom there had been no radiographs of their hips since the year 2000 were invited for a review and a radiograph of the pelvis with both hips. Patients who were incapacitated due to other medical conditions and who were unable to come to the hospital for a radiograph were contacted by telephone, so that we could obtain information about the status of the hip. Cementing quality assessed using Barrack grading system (Barrack et al. Citation1992). Cement mantle thickness was studied in three acetabular regions (Delee and Charnley Citation1976) and seven femoral regions (Gruen et al. Citation1979) on postoperative serial radiographs (n = 46). Femoral component alignment was defined as neutral (if less than 10° of varus or valgus), varus (more than 10° varus) or valgus (more than 10° valgus). Acetabular component alignment was defined as neutral (if the cup alignment was between 30° and 60°), horizontal (if < 30°) or vertical (if < 60°). Acetabular loosening was defined as presence of radiolucent lines more than 1 mm in thickness around the entire circumference of the acetabular component involving all 3 regions (Delee and Charnley Citation1976), or migration of the acetabular component (Stauffer Citation1982). Definite loosening of the femoral stem was defined as migration of the component, as demonstrated by more than 10° of change in the alignment of the femoral component (Harris et al. Citation1982) or more than 5 mm of subsidence. Possible loosening of the femoral component was defined as the appearance of a radiolucent line of up to 2 mm in width at the cement-prosthesis interface which had not been present on the postoperative radiograph (Massoud et al. Citation1997).
Survival analysis of Harvard and Charnley femoral stems was performed according to the Kaplan-Meier method using various endpoints. Cox proportional-hazard analysis was used to evaluate the effect of various factors on the survival of the prosthesis. Log-rank sum test was performed to compare the survival of the Harvard and Charnley femoral stems. Student's two-tailed t-test was used for comparison of the stem alignment and cement mantle thickness between the two groups.
Results
Charnley group
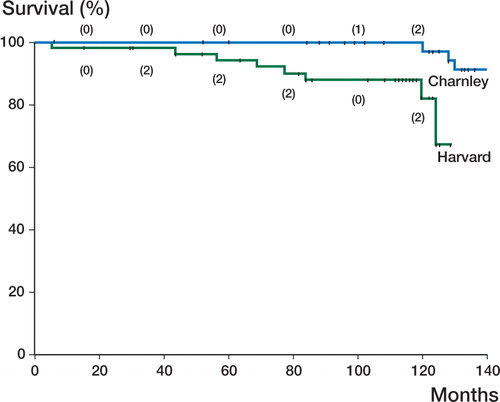
Median follow-up for the patients who did not have any revision hip surgery was 11 (4.3–21) years. Of these, 3 patients had a follow-up duration of between 4.3 and 7 years. In 37 of 48 patients, Charnley femoral stem THA was performed before the Harvard femoral stem THA (mean interval 4.9 years). Cementing quality was noted in 41 hips. It was grade A in 17 patients (41%), grade B in 22 patients (54%), and grade C in 2 patients (5%). Femoral stem alignment was neutral in 98% and varus (more than 10°) in 2% of the patients. Acetabular component alignment was neutral in 95%, and horizontal (closed) in 5% of the patients. It was seen that 2 out of 3 revisions performed for ASL were in the group in which the cement mantle was less than 2 mm thick in regions 2, 3 and 4. 3 hips were revised for aseptic loosening of the femoral and acetabular components between 10 and 11 years after the primary procedure. 2 hips showed evidence of possible loosening, 7 years and 17.1 years after the primary THA. 1 hip was revised in two stages for deep infection 6 months after the primary procedure. The 10-year survival for the femoral and acetabular component using revision surgery for aseptic loosening as an end-point was 95% (95% CI: 44–47) (). The 10-year survival for the femoral component using aseptic loosening (with or without revision surgery) as an endpoint was 92% (95% CI: 42–46).
Figure 1. Kaplan-Meier curve for the Charnley (top curve) and Harvard (bottom curve) femoral stems using revision for aseptic loosening as an endpoint. (Numbers in parentheses indicate the events occurring at that point in time).
Comparison of cement mantle thickness in the Harvard and Charnley groups. Values are the number of hips with cement mantle thickness of greater than 2 mm (%)
Harvard group
Median follow-up time for the patients who had no revision hip surgery was 10 (9.3–10.7) years. Cementing quality was noted in 42 hips. It was grade A in 19 patients (45%), grade B in 22 patients (53%), and grade C in 1 patient (2%). Femoral stem alignment was neutral in 45 patients (94%) and valgus (more than 10°) in 3 patients (6%). Acetabular component alignment was neutral in 46 patients (95%), and horizontal in 2 patients (5%). 5 of 8 revisions performed for ASL were in the group in which the cement mantle was less than 2 mm thick in regions 2, 3 and 4 .
8 hips were revised for aseptic loosening of the femoral component at a median interval of 6.3 (3–10.4) years after the primary procedure. Of 8 revision procedures performed for aseptic loosening of the femoral component, 6 were done between 3 and 7.1 years after the index procedure. The remaining two revision procedures were performed at 10 and 10.4 years after the primary THA. 1 patient sustained periprosthetic femoral fracture due to aseptic loosening around the femoral component. 1 patient had partial sciatic nerve injury after the THA. The acetabular component was also revised in 2 of these 8 hips. 1 hip showed evidence of possible loosening. 3 hips were revised in two stages for deep infection at 10, 24 and 28 months after the primary hip procedure. The 10-year survival for the femoral component using revision surgery for aseptic loosening as an endpoint was 80% (95% CI: 34–42) (). The 10-year survival for the femoral component using aseptic loosening (with or without revision surgery) as an endpoint was 70% (95% CI: 30–36). The 10-year survival for the acetabular component using revision surgery for aseptic loosening as an endpoint was 95% (46, 95% CI: 44–47).
Comparison
12 patients were already deceased at the time of the study, without any of the hips being revised—except one hip in the Harvard group, which was revised for aseptic loosening 4 years after the primary THA. The difference between 10-year survival rates of the femoral stem was statistically significant (log-rank sum test p = 0.006). In 75% of the patients (37 out of 48), Charnley femoral stem arthroplasty had been performed almost 5 years prior to the Harvard femoral stem arthroplasty. Hence, the patients were 5 years younger and relatively more active when Charnley femoral stem arthroplasty was performed. Despite this, the 10-year survival of the Harvard femoral stem was significantly less than that of the Charnley femoral stem. The percentage of THA in which the cement mantle thickness was more than 2 mm in various femoral and acetabular regions was almost similar in both groups, except for regions 2, 3 and 6 . More femora had cement mantle thicker than 2 mm in the Harvard group than in the Charnley group in region 2 (35% vs 22.5%, p = 0.2) and region 6 (92.5% vs 75%, p = 0.02). Alignment of the femoral stem was neutral in 83 and 73 of the hips in the Charnley and Harvard groups, respectively (p = 0.9). Cox regression analysis was performed to identify effect of multiple factors on the survival of the THA. We also performed logistic regression analysis to identify any effect of individual factors on the final out-come. None of these factors (thickness and quality of the cement mantle, alignment of the acetabular and femoral implants) had any influence on implant survival (p < 0.05 for all parameters)
Discussion
It has been shown in a review of 3,153 bilateral staged THAs that the second of the bilateral THAs had better survival than the unilateral THAs (Visuri et al. Citation2002). In our study, although the Charnley stem was inserted before the Harvard stem in most of the patients, 10-year survivorship was better for the former design. This poor outcome in the Harvard group could be due to matt surface finish of the femoral stem. The other difference between the two femoral components is a gradual taper near the tip of the Harvard femoral stem. One laboratory study (Estok et al. Citation2000) has suggested that the peak cement strains adjacent to a stem tip remain well below the endurance limit of cement, as long as the transition region where the narrow tip meets the body of the implant is gradual. Race et al. (Citation2002) reported more gaps at the metal-cement interface with a grit-blasted cemented Charnley femoral stem (Ra 5.3 μm) than with a similar design with a satin surface (Ra 0.75 μm).
Some studies have reported a less satisfactory outcome using femoral components with a rough surface (Rockbom and Olsson Citation1993, Mohler et al. Citation1995, Collis and Mohler Citation1998, Fowler et al. Citation1988). However, there have also been reports of satisfactory results with rough-surfaced femoral components (Wroblewski and Siney Citation1992, Malchau et al. Citation1993, Mulroy et al. Citation1995, Sanchez-Sotelo et al. Citation2002, Meneghini et al. Citation2003). These studies suggest that components with a rough surface can yeild satisfactory results when other factors are such that the bond between cement and stem remains intact for a sufficient length of time. Failure of THAs is of multifactorial origin (cementing, patient characteristics, component design) (Harris Citation1998); thus, valid comparison cannot be made unless most of the factors are similar between the studies being compared.
Some studies have compared the results of femoral stems with identical geometry but different surface finish. Hinrichis et al. (Citation2003) compared Marburg femoral stems made of titanium alloy with smooth (Ra 1.3 μm) and rough surface (Ra 4.3 μm) finish, but with similar stem geometry. They reported 95.4% survival (at 13 years) for the smooth-surface femoral component and 76.7% survival (at 8 years) for the equivalent component with a rough surface. Howie et al. (Citation1998) reported better survival rates for polished Exeter femoral stems than for those with a rough finish. Similarly, Collis and Mohler (Citation2002) reported a higher failure rate for Iowa femoral stems with a rough surface than for the corresponding design with a polished surface. Dall et al. (Citation1993) reported 11.4% and 3.1% incidence of aseptic loosening with matt- finish and polished-surface Charnley femoral stems, respectively.
A recent prospective randomized controlled trial comparing 4.8-year results of polished and grit-blasted femoral stems of the same geometry found no significant difference regarding the incidence of lysis or radiolucent lines (Vail et al. Citation2003). It remains to be seen whether these short-term results persist after longer follow-up duration. Cementing quality (Barrack grade), component alignment, and cement mantle thickness do not appear to have any effect on the final outcome of the THAs in our study, which is in contrast with the findings of other studies (Ebramzadeh et al. Citation1994, Kobayashi et al. Citation1997, Chambers et al. Citation2001). The reason for this observation may be due to the relatively small number of patients in our study.
This retrospective review lacks prospective information about clinical outcomes in terms of clinical scores. The procedures were carried out by a number of surgeons, but at the same hospital. As the same group of surgeons operated on most of the patients in our two study groups, we believe that the effect of differences in individual surgical techniques and levels of skill should be minimal. Our results suggest that smooth-surface femoral components have a better 10-year survivorship than rough-surface femoral components of similar geometry.
No competing interests declared.
- Barrack R L, Mulroy R D, Harris W H. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg (Br) 1992; 74: 385–9
- Chambers I R, Fender D, McCaskie A W, Reeves B C, Gregg P J. Radiographical features predictive of aseptic loosening in cemented Charnley femoral stems. J Bone Joint Surg (Br) 2001; 83(6)838–42
- Collis D K, Mohler C G. Loosening rates and bone lysis with rough finished and polished stems. Clin Orthop 1998, 355: 113–22
- Collis D K, Mohler C G. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented ctems with essentially the same geometry. J Bone Joint Surg (Am) 2002; 84: 586–92
- Dall D M, Learmonth I D, Solomon M l, Miles A W, Davenport J M. Fracture and loosening of Charnley femoral stems. Comparison between first-generation and subsequent designs. J Bone Joint Surg (Br) 1993; 75(2)259–65
- DeLee J G, Charnley J. Radiographical demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Ebramzadeh E, Sarmiento A, McKellop H A, Llinas A, Gogan W. The cement mantle in total hip arthroplasty. Analysis of long-term radiographic results. J Bone Joint Surg (Am) 1994; 76(1)77–87
- Estok D M, 2nd, Harris W H. A stem design change to reduce peak cement strains at the tip of cemented total hip arthroplasty. J Arthroplasty 2000; 15(5)584–9
- Fowler J L, Gie G A, Lee A J, Ling R S. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am 1988; 19(3)477–89
- Gruen T A, McNeice G M, Amstutz H C. “Modes of failure” of cemented stem- ype femoral components: a radio-graphic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Harris W H. Long term results of cemented femoral stems with roughened precoated surfaces. Clin Orthop 1998, 355: 137–43
- Harris W H, McCarthy J C, Jr, O'Neill D A. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg (Am) 1982; 64(7)1063–7
- Hinrichs F, Kuhl M, Boudriot U, Griss P. A comparative clinical outcome evaluation of smooth (10-13 year results) versus rough surface finish (5-8 year results) in an otherwise identically designed cemented titanium alloy stem. Arch Orthop Trauma Surg 2003; 123(6)268–72
- Howie D W, Middleton R G, Costi K. Loosening of matt and polished cemented femoral stems. J Bone Joint Surg (Br) 1998:; 80(4)573–6
- Kobayashi S, Takaoka K, Saito N, Hisa K. Factors affecting aseptic failure of fixation after primary Charnley total hip arthroplasty. Multivariate survival analysis. J Bone Joint Surg (Am) 1997; 79(11)1618–27
- Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978-1990. Acta Orthop Scand 1993; 64(5)497–506
- Massoud S N, Hunter J B, Holdsworth B J, Wallace W A, Juliusson R. Early femoral loosening in one design of cemented hip replacement. J Bone Joint Surg (Br) 1997; 79(4)603–8
- Meneghini R M, Feinberg J R, Capello W N. Primary hybrid total hip arthroplasty with a roughened femoral stem: integrity of the stem-cement interface. J Arthroplasty 2003; 18(3)299–307
- Mohler C G, Callaghan J, Collis D K, Johnston R C. Early loosening of the femoral component at the cement-prosthesis interface after total hip replacement. J Bone Joint Surg (Am) 1995; 77(9)1315–22
- Mulroy W F, Estok D M, Harris W H. Total hip arthroplasty with use of so-called second-generation cementing techniques. A fifteen-year-average follow-up study. J Bone Joint Surg (Am) 1995; 77(12)1845–52
- Race A, Miller M A, Ayers D C, Cleary R J, Mann K A. The influence of surface roughness on stem-cement gaps. J Bone Joint Surg (Br) 2002; 84(8)1199–204
- Rockborn P, Olsson S S. Loosening and bone resorption in Exeter hip arthroplasties. Review at a minimum of five years. J Bone Joint Surg (Br) 1993; 75(6)865–8
- Sanchez-Sotelo J, Berry D J, Harmsen S. Long-term results of use of a collared matte-finished femoral component fixed with second-generation cementing techniques. A fifteen-year-median follow-up study. J Bone Joint Surg (Am) 2002; 84(9)1636–41
- Sarmiento A, Natarajan V, Gmen T A, McMahon M. Radiographic performance of two different total hip cemented arthroplasties. A survivorship analysis. Orthop Clin North Am 1988; 19(3)505–15
- Stauffer R N. Ten-year follow-up study of total hip replacement. J Bone Joint Surg (Am) 1982; 64(7)983–90
- Vail T P, Goetz D, Tanzer M, Fisher D A, Mohler C G, Callaghan J J. A prospective randomized trial of cemented femoral components with polished versus grit-blasted surface finish and identical stem geometry. J Arthroplasty (Suppl) 2003; 18(7)95–102
- Visuri T, Turula K B, Pulkkinen P, Nevalainen J. Survivorship of hip prosthesis in primary arthrosis: influence of bilaterality and interoperative time in 45,000 hip prostheses from the Finnish endoprosthesis register. Acta Orthop Scand 2002; 73(3)287–90
- Wroblewski B M, Siney P D. Charnley low-friction arthroplasty in the young patient. Clin Orthop 1992, 285: 45–7