Abstract
Background The frontal pelvic plane has traditionally served as the reference plane for implantation of the acetabular cup during total hip arthroplasty, with referencing performed with the patient supine on the operating table. During daily activities in an upright position, the frontal pelvic plane changes from a horizontal to a vertical orientation. If this change in orientation is accompanied by a substantial change in pelvic inclination angle, it would mean that the use of the frontal pelvic plane as a reference plane for implantation of the acetabular cup would not be valid for proper alignment of the cup. To evaluate this possibility, we measured the change of inclination of the pelvis from the supine to the standing position.
Subjects and methods We evaluated 120 patients, first positioned in a standing position and then supine on a table. Three pelvic landmarks were digitized percutaneously, and the spatial coordinates were calculated with regard to pelvic orientation in the horizontal and the vertical plane.
Results We found a mean inclination of 6.7° in the standing position and 5.6° in the supine position. Patients who were more than 60 years of age who did not have coxarthrosis had a greater inclination angle (8.7°) while standing. Pelvic orientation was stable with regard to the supine and standing positions. These results were independent of sex, level of arthrosis, or status after implantation of a total hip replacement.
Interpretation The frontal pelvic plane is a valid reference plane for implantation of the acetabular cup.
▪
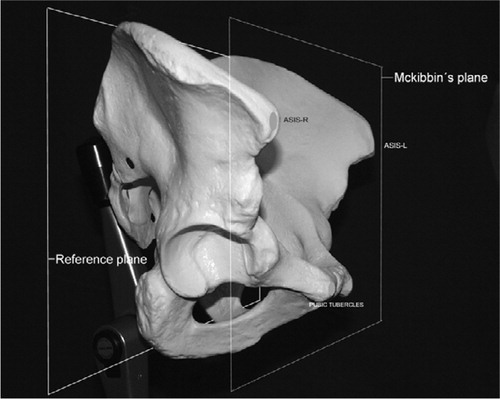
Malalignment of the acetabular cup may result in dislocation or impingement of the neck with resultant polyethylene wear causing early loosening (Di Gioia et al. Citation1998, Hassan et al. Citation1998). Correct placement of the acetabular cup requires correct knowledge of pelvic orientation. The frontal pelvic plane defined by the two anterosuperior iliac spines and the pubic tubercles, as described by McKibbin (Citation1970), serves as the reference plane during total hip arthroplasty. In conventional surgical procedures, this plane is usually determined indirectly with jigs that are mounted onto cup impactors and aligned with the operating table (the horizontal plane), the wall (the vertical plane), and the trunk of the patient (the estimated longitudinal axis).
In computer-assisted orthopedic surgery, computed-tomography-based, fluoroscopy-based, or imageless navigation devices are used to measure the frontal pelvic plane directly by digitizing the anterosuperior iliac spines and the pubic tubercles. The cup is then positioned by reference to this plane.
Direct or indirect referencing is done intraoperatively with the patient supine on the operating table. During daily activities such as standing or walking, however, the patient is in an upright position. Because the spatial orientation of the acetabulum depends on pelvic inclination (Anda et al. Citation1990), a change in the angle of pelvic inclination from the supine position to the standing position could lead to a different orientation of the acetabulum, thereby putting the load onto the cup in areas other than those planned for before the arthroplasty.
Our hypothesis was that the orientation of the pelvis and the frontal pelvic plane does not change relative to the patient's trunk in the standing and supine positions, and that the frontal pelvic plane is therefore a valid reference plane for positioning of the acetabular cup during total hip arthroplasty ().
We evaluated and compared the pelvic inclination angle in the standing and supine positions. Additionally, we investigated whether gender or the presence of artificial hip joints or coxarthrosis influenced the orientation of the pelvis.
Subjects and methods
120 adult volunteers (60 women) were included in the study. The average age was 59 (21–91). The protocol for human subjects was approved according to the regulations of our country, and written informed consent was obtained from all subjects. The patients were divided into four groups of 30 patients each (15 men and 15 women). Group 1 was defined as young (mean age 30 (21–46) years) and healthy persons without any history of hip or low back problems. Group 2 included patients of various ages (mean age 69 years) who had undergone total hip arthroplasty no more than 6 weeks before enrollment in the study. Group 3 consisted of patients of various ages (mean age 68 years) who had coxarthrosis regardless of cause or duration. Group 4 had the same inclusion criteria as group 1 (healthy persons without any history of hip or low back problems) but included only persons older than 55 years of age (mean age 72 years).
For assessment of reference points (anterosuperior iliac spines and pubic tubercle) a 3-dimensional digitizing arm (Micro-Scribe-3DX; Vizion, Glendale, CA) was mounted onto a table that was rigidly fixed to the ground.
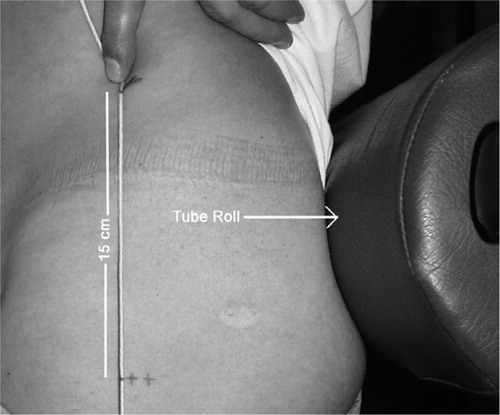
For measurements with the patient standing, a tube roll was manufactured and mounted to two bars fixed to the ground. The tube roll was adjustable to the height of the patient's lower back () and served to prevent the patient's pelvis from moving while the investigator digitized the landmarks of the pelvis. Patients were barefoot and were asked to position themselves in a comfortable standing position with the arms hanging free and the head held straight. A perspex plate with three machined holes was adjusted with the use of a spirit level to serve as the vertical plane and was digitized for each patient. The anterosuperior iliac spines and the left pubic tubercle on the pelvis were digitized percutaneously.
Figure 2. A. The settings for measurements in the standing position, highlighting the reference plane and the pelvic reference points. B. Photograph showing the settings for measurements in the supine position.
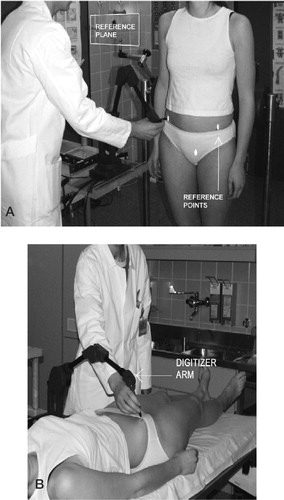
For the second part of the examination, another perspex plate with three holes was positioned onto the table to serve as the horizontal reference plane. With the patients in the supine position, the afore-mentioned landmarks on the pelvis were digitized in the same manner as before ().
To verify that the tube roll was able to hold patients in a natural upright position, patients in Group 1 first had to stand with their lower back positioned 20 cm in front of the tube roll. With a skin marker, the highest point of the iliac crest on one side was marked. A plumb-line was held to the point and another mark was made exactly 15 cm below on the lateral thigh. After this, patients had to step back until they touched the tube roll. The plumb-line was again placed on the mark of the iliac crest and another mark was made in the same way. The distance between the two points was measured, and the resulting change in the angle of inclination was calculated with a cotangents function ().
We calculated pelvic inclination as the angle between the frontal pelvic plane and the horizontal or vertical reference plane. Calculations were done using the mathematic software Maple 7 (Waterloo Maple Inc., Ontario, Canada). Statistical analysis was done with SPSS for Windows version 11 (SPSS Inc., Chicago, IL). All measurements were made by one author (EM).
Statistics
In view of the moderate sample size and the fact that data were not normally distributed, we used nonparametric tests. Differences between the four study groups were analyzed using Kruskal-Wallis H-test. Furthermore, we performed an analysis of covariance to adjust the pelvic inclination in the standing and supine position and the difference between the pelvic inclination in both positions for effects of sex and age. To test the effect of age, a rank correlation was performed. Partial correlation was performed to hold a third variable constant while examining the relations between two other variables. All p-values are two-tailed.
The reproducibility of the measurements was assessed by a pre-post comparison (baseline vs. 1 week) of 10 subjects. Spearman rank-order correlation coefficients were used as indices of test-retest reliability.
Results
The mean value of pelvic inclination in the standing position of the total sample size was 6.7°, and varied between 5.2° and 8.7° in the 4 groups (p = 0.004) (). The p-value of the pelvic inclination in the standing position increased to 0.05 after considering effects of gender and age by analysis of covariance. The effects of gender (p = 0.2) and age (p = 0.6) were not significant.
Table 1. Mean values and standard deviations of the pelvic inclination position
The mean value of pelvic inclination in the supine position of the total sample size was 5.6° and varied between 4.4° and 6.1° in the 4 groups () without statistical significance (p = 0.1). Analysis of covariance to adjust the inclination angle of the pelvis in the supine position by the effects of sex and age did not show significant differences between the groups. The effects of gender (p = 0.2) and age (p = 0.4) were not significant.
For each person, we computed the difference between pelvic inclination in the standing and in the supine position. The mean value of the difference of pelvic inclination in the two positions of the total sample size was −1.1° (SD 4.8°). In groups 1–4 it was 1.0° (SD 4.3°), −1.9° (SD 4.3°), 0.6° (SD 4.6°) and −3.0° (SD 5°), respectively. In the total material, the inclination differed between the two positions (p = 0.007). This difference disappeared after adjustment for gender and age. Gender (p = 0.07) and age (p = 0.9) had no influence.
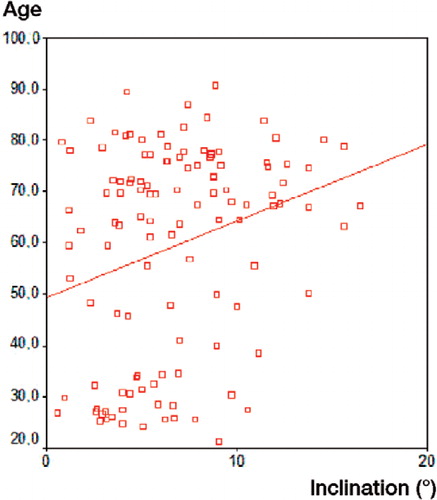
As the differences between the four groups were influenced by the age of the patients, we performed a Spearman's rank correlation between age, standing position, supine position and difference between supine and standing position to detect any relationship. We found a relation between age and standing position (p = 0.01) (). The pelvic inclination in the standing position increases when people become older (). Furthermore, we found a relation between age and the difference between supine and standing (p = 0.04). This relationship is obviously caused by the effects of the standing position. In a subsequent partial correlation, to control for these effects, we found no significant relationship between age and the difference between supine and standing (p = 0.4).
Table 2. Spearman's rank correlation between age, standing position, supine position and the difference between supine and standing
The correlation between repeated measurements in standing position was 0.78 (p = 0.008) and 0.99 (p < 0.001) in supine position.
Discussion
To identify the frontal pelvic plane intraoperatively, surgeons perform referencing with the patient in supine position on the operating table. However, the main load acting on the acetabular cup is with the patient standing. In this position, the load on the cup is not higher than the patient's body weight. According to an experimental study, however, this load doubles when the patient moves from seated to standing, and triples during walking (Bergmann et al. Citation2001). If acetabular orientation is related to the frontal pelvic plane, a change in pelvic inclination might have effects on the load distribution.
One aim of our study was to try to understand more about the orientation of the pelvis in different positions. By percutaneously digitizing three osseous landmarks, the frontal pelvic reference plane was defined for all experiments. Due to soft tissue coverage, these landmarks may be difficult to identify. This means that some inaccuracy can be expected in defining the frontal pelvic plane—which is a limitation of our study. For the same subject, the soft tissue thickness is the same in standing and supine position. We therefore assumed that the inaccuracy of the measurement was small and the same for both positions. We have little experience of the lateral decubitus position, which is probably more difficult to reproduce. Thus, we did not perform measurements with patients in the lateral position.
According to anatomic definitions, the frontal pelvic plane is assumed to be parallel to a horizontal plane in the supine position and to a frontal plane in the standing position (Williams et al. Citation1989). These definitions have been made without considering the different conditions of patients, such as age, sex, degree of coxarthrosis, or the presence of disorders of the lumbar spine. Despite anatomic definitions, none of our patients showed an inclination angle of 0°, comparing the digitized plane to the frontal plane. In both positions, all patients showed some degree of pelvic inclination. This is in contrast to the findings of Anda et al. (Citation1990), who described a reclination of the pelvis of 4° to 6° in both the standing and the supine position. Since they used a self-made inclinometer, which was hand-held and pressed onto the pelvis, movements could probably not be avoided, which may be the reason for the different findings. In addition, the authors reported that pelvic inclination was the same in standing and supine position with regard to the reference plane. Our measurements confirmed this finding of an essentially stable pelvic orientation. Jaramaz et al. (Citation1998) compared radiographs of patients in supine and standing position, and reported a change in pelvic flexion of between 5° and 20°. In addition, Eddine et al. (Citation2001) reported important variations of the position of the pelvis during change from the lying to the standing position, which can lead to an error of cup orientation of up to 20°. Nishihara et al. (Citation2003) used image matching between a 3-dimensional computed tomography model and anteroposterior radiographs to calculate pelvic flexion angles with the patients in different positions and found that in 10% of the cases, the difference between the supine and the standing position was more than 10°. Gelb et al. (Citation1995) showed a correlation between advancing age and overall sagittal balance in asymptomatic individuals. Most of their patients were able to maintain sagittal alignment in the standing position, and the authors made the assumption that the aging process can lead to a more forward sagittal vertical axis with loss of distal lumbar lordosis. Our results indicate that bending forward is the reason for increasing pelvic inclination: changes in pelvic inclination from standing to supine position were low in all groups except in group 4 which consisted of older patients without coxarthrosis. These patients showed a greater inclination angle in the standing position. The mean difference between standing and supine position in all 120 patients was only 1.1°, which is clinically irrelevant.
We conclude that the frontal pelvic plane is a valid reference plane for the implantation of the acetabular cup.
The authors thank Markus Ertl, M.Sc. for performing statistical analyses and Stryker-Leibinger (Freiburg, Germany) for providing the Micro-scribe digitizer arm.
No competing interests declared.
- Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum: A radiographic, computed tomographic and clinical investigation. Acta Radiol 1990; 31: 389–94
- Bergmann G, Deuretzbacher G, Heller M, Graichen F, Rohlmann A, Strauss J, Duda G N. Hip contact forces and gait patterns from routine activities. J Biomech 2001; 34: 859–71
- DiGioia A M, Jaramaz B, Blackwell M, Simon D A, Morgan F, Moody J E, Nikou C, Colgan B D, Aston C A, Labarca R S, Kischell E, Kanade T. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop 1998, 355: 8–22
- Eddine T A, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for measurements of positon of a prosthetic cup. Surg Radiol Anat 2001; 23(2)105–10
- Gelb D E, Lenke L G, Bridwell K H, Blanke K, McEnery K W. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 1995; 20: 1351–8
- Hassan D M, Johnston G H, Dust W N, Watson G, Dolovich A T. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty 1998; 13: 80–4
- Jaramaz B, DiGioia A M, 3rd, Blackwell M, Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop 1998, 354: 70–81
- McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg (Br) 1970; 52: 148–59
- Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop 2003, 411: 140–51
- Williams P L, Warwick R, Dyson M, Bannister L H. Gray's Anatomy 37th ed., P L Williams, R Warwick, M Dyson, L H Bannister. Churchill Livingstone, Edinburgh 1989