Abstract
Background Treatment of severely displaced supracondylar fracture of the humerus in children remains a challenge. We retrospectively assessed the outcomes of the minimally invasive open reduction techniques used in our institutions for the treatment of grade 3 supracondylar fractures in children which could not be reduced by closed manipulation.
Patients and methods 78 children (58 boys) with severely displaced supracondylar fractures of the humerus and severe swelling were treated with either a minimal incision in the anticubital fossa and manipulation of the distal fragment with the thumb, or a small stab incision and manipulation of the fracture fragment with a small-sized suction tip. The fractures were stabilized with 1.6-mm Kirschner wires.
Results and interpretation The outcome after a follow-up of at least 3 years was excellent in 76 cases and poor in 2 cases. No scar contractures or other complications were observed. These techniques seem safe and effective in the treatment of irreducible grade 3 supracondylar fractures of the humerus in children.
▪
Closed reduction and Kirschner wire fixation is a widely accepted method for treatment of severely displaced supracondylar fractures of the humerus in children (Flynn et al. Citation1974, Mostafavi and Spero Citation2000). Open reduction is indicated when repeated attempts at closed reduction are unsuccessful, in cases of open injury or circulatory involvement (Gruber and Healy Citation1996). For open reduction, a variety of approaches have been suggested. An anterior approach has been advocated by Carcassonne et al. (Citation1972), Kekomaki et al. (Citation1984) and Aronson et al. (Citation1993). For irreducible, severely displaced supracondylar fractures of the humerus with gross swelling, we used a minimal anterior approach with reduction of the fracture fragments by thumb manipulation or using a small suction tip and stabilization of the fractures with K-wires. We report our experience of these techniques in 78 children.
Patients and methods
We reviewed 304 supracondylar fractures of the humerus retrospectively; all of them had been treated at two institutions from 1994 to 2002. The fractures were classified according to Gartland (Citation1959). 165 of these fractures were Gartland type III, among them 84 requiring open reduction. The others were managed by closed methods. Indications for open reduction included failure of 3 attempts at closed reduction, open fractures or interference with the circulation.
We retrospectively studied the children undergoing open reduction. 6 children were lost to follow up. The other 78 children (58 boys) had a follow-up of at least 3 years. We divided these children into two groups. Before 1994–1997, all children (n = 36) in both institutions of the senior authors (HRS and CWO) underwent an open reduction through a small incision in the cubital fossa and reduction of the fracture fragments by manipulation with the surgeon's thumb (thumb reduction technique). From 1997 through 2002, all children (n = 42) in the institution of HRS underwent a procedure which entailed a small stab incision and reduction of the fracture fragments by manipulating them with a small-sized suction tip (joystick reduction technique). However, all the children who underwent these procedures in the hospital to which CWO is affiliated continued to be treated by the thumb reduction technique.
The average age of the 36 children who were treated by the thumb reduction technique group was 6.4 (2–11) years and that of the 42 children treated by the joystick reduction technique was 5.4 (2.6–12) years. The average time of admission to hospital after the injury was 8 (3–20) h. All the fractures were due to extension injury with a fall on the outstretched hand during various activities. In the thumb reduction technique group, 3 patients had median nerve injury, 1 had a radial nerve injury and 1 had a fracture of the distal end of the radius. 34 of the fractures were closed and 2 were open. In the joystick reduction technique group, 1 patient had a median nerve injury and 1 had a fracture of the distal end of the radius. 40 fractures were closed and 2 fractures were open. In all patients who underwent these procedures, 3 attempts at achieving reduction by closed manipulation failed.
Techniques
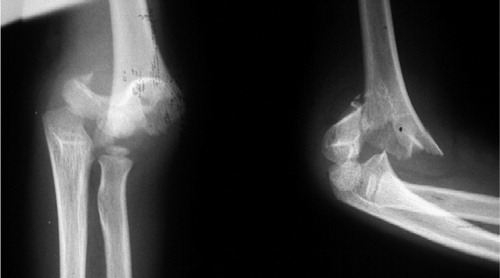
In the thumb reduction technique, we used a 2-cm transverse anteromedial incision to reach the fracture site ( and ). The plane between the brachialis and the biceps brachii muscle was dissected bluntly. In most cases, the fracture was easily approached through the already ruptured brachialis muscle (by the anteriorly displaced medial beak of the proximal fragment). The hematoma was evacuated through the wound and the interposed tissue, if any, was separated from the ends of the fracture.
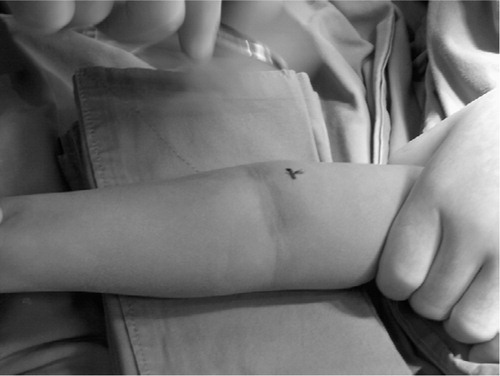
Figure 1. A 2-cm transverse incison was made on the medial side of the cubital fossa (arrow). Note associated skin blisters.

Figure 2. Reduction of the fracture through an anteromedial mini-incision. Thumb pressure is applied over the spike of the proximal fragment for control of rotation of the fragment and simultaneous traction is applied to the foream using the other hand.

In the joystick reduction technique, a 2–3-mm small nick incision (just enough to introduce a small-size suction tip percutaneously) was made using a stab knife blade at the anteromedial aspect of the anticubital fossa ( and ). The suction tip was inserted through this percutaneous route, and was used as a joystick to apply anterior pressure on the spike of the proximal fragment. The reason for using the suction tip is convenience of holding its curved base portion, while manipulating the fracture. Also, its tip is blunt—eliminating the risk of iatrogenic neurovascular injury.
Figure 4. Manipulation of the proximal fragment with the suction tip by the operating surgeon, as the assistant prepares to pass the lateral K-wire.

The reduction in the two techniques was done under image intensifier control. Pressure was applied over the spike of the proximal fragment for control of rotation of the fragment, and simultaneous traction was applied to the forearm with the other hand for reduction. During this maneuver, the elbow was flexed 90° and the distal fragment was manipulated to correct the coronal tilting, translation and rotation. The reduction was confirmed in two ways: by palpation of a step or a gap, if any, and observation under the image intensifier.
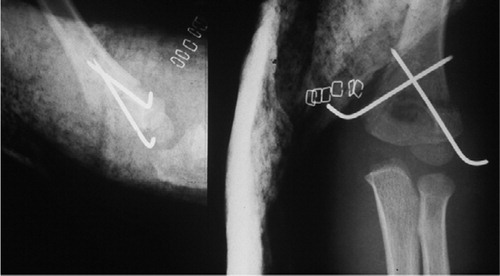
Once anatomical reduction was achieved, it was secured with 1.6-mm Kirschner wires (2 wires in 22 fractures and 3 wires in 20 fractures) ( and ) inserted percutaneously under image intensifier control, either through the medial and lateral condyles (cross manner, 24 fractures) or through the lateral condyle (parallel fashion, 12 fractures) to the opposite cortex, by an assistant. When the crossed K-wire technique was used, the lateral wire was inserted first. The wire ends were cut, bent and kept outside the skin. The elbow was splinted with a plaster slab in 30–60° of flexion and neutral rotation.
In all cases, plasters were removed after 3 weeks and active movements were allowed. The K-wires were removed without anesthesia after another week. The patients were followed up at 3 weeks, 4 weeks, 3 months, 6 months and then at yearly intervals and radiograms were taken. The Baumann's angle (1973) was measured on the radiographs and the final results were assessed according to the criteria of Flynn and Matthew (Flynn et al. Citation1974). The average follow-up period was 3.3 (3–5.5) years.
Results
The average surgical time was 34 (28–66) min in the thumb reduction technique group and 25 (15–46) min in the joystick reduction technique group. In the thumb reduction technique group, there was no loss of reduction in the cross-pinned fractures, but 2 fractures with lateral pinning had loss of reduction and developed varus angulation which persisted on further follow-up with minimal or negligible remodeling. The carrying angle was 16° and 18° at the last follow-up—at 3.5 and 5 years, respectively.
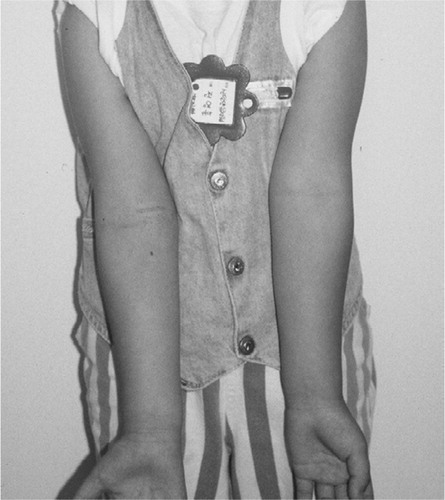
All the fractures united. There was full elbow motion in all the cases at the final follow-up. According to the criteria of Flynn and Matthew, 34 patients had excellent results () while 2 patients had poor results. In the joystick reduction technique group, none of the patients had loss of reduction. All fractures united. There was full elbow motion in all cases at the final follow-up. All 42 patients showed excellent results.
Figure 7. Full extension of the elbow with a minimal, barely visible scar (arrow) at follow-up. Carring angle is the same on the opposite side.
There was 1 superficial wire infection in the thumb reduction technique group and 3 superficial wire infections in the joystick reduction technique group. The wire infections were treated with local antibiotic dressing and healed uneventfully after the wires were removed. None of the patients in either of the groups had skin necrosis, myositis ossificans or Volkmann's contractures. All the nerve injuries had completely recovered on follow-up.
Discussion
Some of the severely displaced supracondylar fractures in children can be satisfactorily treated by closed reduction and percutaneous K-wire fixation (Flynn et al. Citation1974). Failed closed reduction after repeated manipulations makes further manipulative reduction risky, adds to soft tissue injury and may necessitate open reduction, which can be performed using different approaches (Nassar and Chater Citation1976).
A lateral approach is usually safe, but control of rotation may be difficult (Gates Citation1982). A posterior approach has been claimed to be advantageous by some authors (Sibly et al. Citation1991, Gruber and Healey Citation1996), but may damage the intact posterior extensor muscles and result in postoperative elbow stiffness (Celiker et al. Citation1990, Gennari et al. Citation1998).
An anterior approach was first described by Hagenbeck in 1894 (Carcassonne et al. Citation1972), and later modified by Carcassonne et al. (Citation1972). It provides excellent exposure of the fracture site and in cases of associated neurovascular injury, direct access for repair can be achieved by extending the skin incision medially (Carcassonne et al. Citation1972, Kekomaki et al. Citation1984, Aronson et al. Citation1993, Kasser and Beaty Citation2001).
To avoid a long scar in the anterior fossa, we used a small 2-cm incision, which is sufficient to insert the thumb for reduction in the initial group of patients. However, after having gained experience in both techniques, we feel that the joystick reduction technique is as efficacious as the thumb reduction technique—and both have the added advantage of a smaller incision compared to the conventional open reduction techniques. The three components (coronal tilting, translation and rotation) of the distal fragment are easily corrected by pressure on the medial spike with the thumb or a suction tip and traction applied to the forearm simultaneously. The spike of the fracture fragment is mostly just beneath the skin (due to the ruptured brachial muscle), and hence the fracture can be easily approached and reduced after removal of any intervening soft tissue (Gennari et al. Citation1998). Alternately, the suction tip can be interposed between the soft tissue and the fractured fragment in order to free the latter. The other advantage is that the fracture hematoma is removed and the compartment is decompressed, which minimizes the risk of development of Volkmann's contracture (Mubarak and Carroll Citation1979).
Feared iatrogenic neurovascular injury (Gosens and Bongers Citation2003), and myositis ossificans (Celiker et al. Citation1990) were not found in our series. In the thumb reduction technique, while reducing the fracture, the thumb protects the median nerve and the brachial artery from the sharp fragment. In the joystick technique, the spike of the proximal fragment is pressed down with the suction tip to control the rotation at the fracture siteand is thus always under the control of the surgeon. Hence, the possibility of neurovascular injury is low.
The 2 poor results in our study were due to loss of reduction postoperatively in 2 small children (aged 2.6 and 3.2 years) treated by lateral percutaneous pinning. Mazda et al. (Citation2001) found loss of reduction in 3 of 90 patients treated with lateral percutaneous pinning. We agree with Mostafavi and Spero (Citation2000) and O'Hara et al. (Citation2000) who found that crossedpin fixation of supracondylar humeral fractures is a safe and effective way of maintaining skeletal stability in children, as none of our cases stabilized by this method had any redisplacement. We fully agree with Fleuriau-Chateau et al. (Citation1998), who stated that open reduction of supracondylar fractures is a safe and effective procedure, and we suggest that this should be done through a minimal incision anteromedially or through a stab incision, and using a small suction tip to joystick the proximal fragment. Stabilization can be performed with two crossed Kirschner wires. In our experience, the anteromedial mini-incision and thumb-assisted technique or the minimally invasive joystick reduction technique have advantages over the conventional open reduction techniques advocated for the management of supracondylar fractures of the humerus in children. The results are comparable, with minimal risk of complications.
No competing interests declared
- Aronson D C, Van Vollenhoven E, Meeuwis J D. K-wire fixation of supracondylar humeral fractures in Children: results of Open Reduction via a ventral approach in comparison with closed treatment. Injury 1993; 24: 179–81
- Baumann E. Mutilation of hand and arm with Volkmann's ischaemic contracture following a compound Monteggia fracture treated by circular plaster cast. Ther Umsch 1973; 30: 877–80
- Carcassonne M, Bergoin M, Hornung H. Results of operative treatement of severe supracondylar fractures of the elbow in children. J Pediatr Surg 1972; 7: 676–9
- Celiker O, Pestici F I, Tuzuner M. Supracondylar fractures of the humerus in children: analysis of the results in 142 patients. J Orthop Trauma 1990; 4(3)265–9
- Fleuriau-Chateau P, McIntyre W, Letts M. An analysis of open reduction of irreducible supracondylar fractures of the humerus in children. Can J Surg 1998; 41(2)112–8
- Flynn J C, Matthews J G, Benoit R L. Blind pinning of displaced supracondylar fractures of the humerus in children. J Bone Joint Surg (Am) 1974; 56: 263–72
- Gartland J J. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959; 109: 145–54
- Gates D J. Supracondylar fracture of humerus: problem in children managed with open reduction. Orthop Rev 1982; 11: 91–8
- Gennari J M, Merrot T, Picklet B, Bergoin M. Anterior approach versus posterior approach to surgical treatment of children's supracondylar fractures: comparative study of thirty cases in each series. J Pediatric Orthop (B) 1998; 7(4)307–13
- Gosens T, Bongers K J. Neurovascular complications and functional outcome in displaced supracondylar fractures of the humerus in children. Injury 2003; 34(4)267–73
- Gruber M A, Healy W A. The posterior approach to the elbow revisited. J Pediatr Orthop 1996; 16(2)215–9
- Kasser J R, Beaty J H. Supracondylar fractures of the distal humerus. Rockwood and Wilkins' Fractures in children, J Beaty, J Kasser. Lippincott Williams & Wilkins, Philadelphia 2001; 577–624
- Kekomaki M, Luoma R, Rikalainen H, Vilkki P. Operative Reduction and Fixation of a Difficult Supracondylar Extension Fracture of the Humerus. J Pediatr Orthop 1984; 4: 3–5
- Mazda K, Boggione C, Fitoussi F, Pennecot G. Systematic pinning of displaced extension-type supracondylar fractures of the humerus in children: a prospective study of 116 consecutive patients. J Bone Joint Surg (Br) 2001; 83(6)888–93
- Mostafavi H, Spero C. Crossed pin fixation of displaced supracondylar humerus fractures in children. Clin Orthop 2000, 376: 56–61
- Mubarak S J, Carroll N C. Volkmann's fracture in children; aetology and prevention. J Bone Joint Surg (Br) 1979; 61: 285–93
- Nassar A, Chater E. Open reduction and Kirschner wire fixation for supracondylar fracture of the humerus. J Bone Joint Surg (Br) 1976; 58: 135–6
- O'Hara L J, Barlow J W, Clarke N M P. Displaced supracondylar fractures of the humerus in children: audit changes practice. J Bone Joint Surg (Br) 2000; 82(2)2004–10
- Reitman R D, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop 2001; 21(2)157–61
- Sibly T F, Briggs P J, Gibson M J. Supracondylar fractures of the humerus in childhood: range of movement following the posterior approach to open reduction. Injury 1991; 22: 456–8