Abstract
Background In the presence of additional disruption of the distal radioulnar ligaments, the interosseous membrane, or the lateral- and/or medial collateral ligament, radial head fractures treated by resection will result in valgus elbow instability, proximal radial migration and/or posterolateral rotatory instability. Radial head replacement has been used to treat or prevent this. We report our experience with the Judet CRF II radial head prosthesis.
Patients and methods We treated 11 patients with a bipolar radial head prosthesis because of elbow instability after previous treatment for Mason-Johnston type III or IV radial head fractures. The outcome was assessed clinically using two standardized elbow function assessment scales, and radiographically after a mean follow-up of 2 years.
Results Clinical outcome was either good or excellent in all patients; all elbows were stable. Radiographically, there were no signs of loosening, fracture or heterotopic ossification. 2 patients required reoperation for subluxation of the prosthesis; both were treated by reducing the size of the modular head of the prosthesis. There was erosion of the capitellum in 1 patient.
Interpretation Bipolar radial head replacement can be used successfully for treatment of the sequelae of radial head fractures. The long-term outcome is, however, unknown.
▪
Fractures of the radial head account for 2–5% of all fractures, and 33% of elbow fractures in adults (Mason Citation1954). The choice of treatment is dictated by additional soft tissue injuries and/or other fractures. Type I fractures, defined according to the Mason-Johnston classification () (Mason Citation1954, Johnston Citation1962), can be successfully treated nonoperatively. Displaced type II fractures should be treated with open reduction and internal fixation (ORIF) (Judet et al. Citation1996). Type III and IV fractures are treated by an attempt at ORIF; if this fails, the radial head is excised.
If there are additional lesions of stabilizing soft-tissue structures of the forearm such as the distal radioulnar ligaments (DRUL) (which are the primary stabilizers of the distal radioulnar joint and part of the triangular fibro-cartilage complex (TFCC)), the interosseous membrane (IM), or the medial- and/or lateral collateral ligament (MCL, LCL), replacement of the radial head is indicated. Radial head resection without replacement in these situations will result in valgus elbow instability, proximal radial migration or posterolateral rotatory instability (Essex-Lopresti Citation1951, Wagner Citation1955, McDougall and White Citation1957, Mikic and Vukadinovic Citation1983, Sowa et al. Citation1995, Janssen and Vegter Citation1998). Radial head replacement is used in an attempt to prevent or treat these complications (Judet et al. Citation1996). We report our experience with the Judet CRF II bipolar radial head prosthesis () for treatment of persistent instability following treatment of Mason-Johnston type III or IV radial head fractures resulting from untreated additional ligamentous injuries.
Table 1. Mason Johnston classification of radial head fractures
Patients and methods
Between 1999 and 2003, we inserted 11 bipolar radial head prostheses (Judet CRF II; Tornier SA, Saint-Ismier, France) in 11 patients (8 men; mean age 43 (26–61) years) who had been treated previously with ORIF (that had subsequently failed; 4 patients) and/or radial head resection (7 patients), for a type III or IV radial head fracture. The patients were evaluated before surgery, and after a mean follow-up time of 2 (1–4) years, using the Elbow Function Assessment Scale (EFA) (de Boer et al. Citation1999, Citation2001) and the Modified Andrews Elbow Scoring System (Timmerman and Andrews Citation1994). All patients were available for follow-up and the clinical outcome at the time of follow-up was assessed by an independent observer. The mean time between the initial trauma and insertion of the prosthesis was 8 years (range 2 weeks to 31 years). Patients reported various complaints, including elbow or wrist pain, and a limited range of motion and/or instability. 3 patients reported instability, 4 reported severe elbow pain with activity and 6 patients reported wrist pain, with proximal radial migration in 4 ().
Table 2. Pre-operative details and details at follow-up of the 11 patients in this series treated with radial head replacement
Operative technique
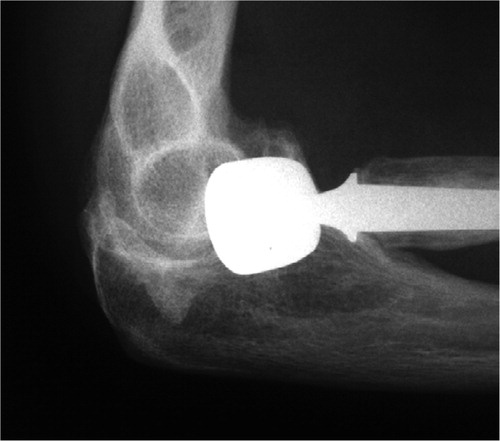
The radial head is exposed through a posterolateral incision, the annular ligament is opened and the radial neck is identified just above the bicipital tuberosity. The medulary canal is prepared using rasps and the size of the implant is determined using trial stems. Trial heads are used to assess stability and impingement against the humerus. A small bone plug and pulse lavage is used and the definitive prosthesis is cemented. Repair or reconstruction of the MCL was performed in 3 patients because the elbow remained unstable after the head replacement (). In 2 patients, adjuvant surgical procedures were performed: an LCL reconstruction in 1 (), and a DRUL reconstruction in the other ().
Figure 2. Lateral radiograph of the bipolar radial head prosthesis: case 1 at 12-month follow-up. Note the anchor used in the LCL repair.
Postoperatively, all patients performed active-assisted motion exercises with the help of a physiotherapist, except for the patient who had wrist surgery, and wore a 90° resting splint during day-time and at night. After 6 weeks, active and passive stretching was allowed and strengthening exercises were started.
Results ()
There were 4 complications, 2 of them requiring reoperation. 2 patients had a limited range of motion, at 2 weeks and 3 months postoperatively, and were come as reflected by the EFA and Andrews score. 1 patient who required reoperation (case 7) had a subluxation of the prosthesis radiographically and lateral instability of the elbow clinically, and was treated 5 months postoperatively with downsizing of the modular head of the prosthesis and reconstruction of the annular ligament. Further recovery in this patient was uncomplicated. The other patient (case 11) also had a subluxation of the prosthesis, and a symptomatic extension deficit that had developed slowly over time. The patient was also treated by downsizing of the modular head, combined with arthrolysis, 12 months postoperatively. Afterwards, the patient's range of motion again got worse over time and at the time of follow-up there was an extension deficit of 40°. Radiographically, however, there were no signs of malposition of the prosthesis.
At the time of follow-up, all patients had a good or excellent outcome as reflected by their EFA and Andrews scores (), including the 2 patients who had a reoperation. Pain decreased in all patients, but they suffered from some pain on activity, and 1 patient still had minor wrist pain. There was no symptomatic elbow instability, but there was some minor medial laxity in 4 patients on clinical examination.
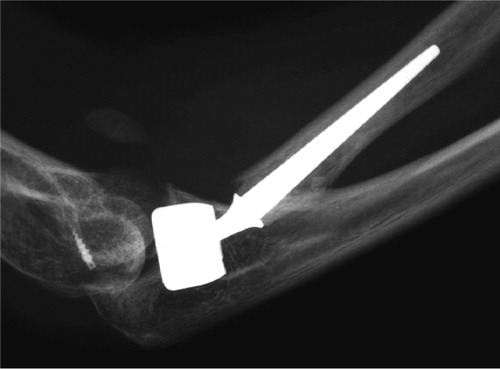
On examination by anteroposterior and lateral radiographs, 10 prostheses had a congruent articulation with the capitellum and the proximal ulna at the time of follow-up. There were no signs of loosening, fracture, heterotopic ossification, or arthrosis. 1 patient (case 7) had erosion of the capitellum at the 30-month follow-up (), but had no clinical symptoms.
Discussion
Commonly used classification systems for radial head fractures do not account for soft tissue injury. However, in patients with complex and severe trauma of the elbow, careful assessment of the ligamentous structures of the elbow, forearm and wrist is essential in treatment planning. Diagnosis of acute ligamentous disruption, however, is difficult. The wrist should be examined for the presence of a dorsal ulnar or ulnocarpal dislocation and plain radiographs of the wrist to assess the DRUL must be taken. Pain and swelling of the forearm may indicate the presence of an IM rupture and pain and a hematoma on the medial side of the elbow may indicate an MCL rupture. In the acutely injured patient, stability of the elbow and wrist joint can only be tested adequately under anesthesia. MR arthrography or ultrasound studies can aid in the diagnosis. Furthermore, patients should also be examined for the presence of fractures of the coronoid process, olecranon and/or capitellum, which can be diagnosed on plain radiographs or by CT scanning.
Radial head resection has been the treatment of choice in cases where ORIF is not feasible due to severe fracture comminution (Radin and Riseborough Citation1966). Complications such as valgus instability, flexion contracture, posterolateral rotatory instability, proximal radial migration and secondary degenerative ulnohumeral arthrosis, however, have been documented in 10–80% of patients after radial head resection (Wagner Citation1955, Mikic and Vukadinovic Citation1983, Sowa et al. Citation1995, Janssen and Vegter Citation1998).
Various kinds of radial head prosthesis have been designed, using various materials: acrylic (Cherry Citation1953), vitallium (Carr and Howard Citation1951) and silicone rubber (Swanson et al. Citation1981). Early results reported for these types of prostheses were favorable; however, a large number of complications have since been reported, including mechanical failure and pathological reactions, synovial and bony inflammation, reactive synovitis, and inflammatory arthritis (Mayhall et al. Citation1981, Gordon and Bullough Citation1982, Worsing Jr. et al. Citation1982, Vander-wilde et al. 1994).
‘Second-generation’ radial head prostheses have been developed, such as the monobloc titanium prosthesis and bipolar vitallium prosthesis. In cadaver studies, both types of prosthesis provide equal stability in MCL-deficient elbows, but not to the same degree as the native radial head (Pomianowski et al. Citation2001). The titanium monobloc prosthesis is nonanatomic in design; problems with sizing have been reported and the wear characteristics of titanium are not ideal (Ashwood et al. Citation2004). The bipolar prosthesis, as used in our study, has an articulation between the stem and the head, which allows free rotation in an arc of 35° of movement in any direction and reduces forces between the radial head and the capitellum. Stem and head size can be selected independently. There is no deformation of the prosthesis under stress loading, and the prosthesis is believed to be able to withstand physiological loading across the radio-humeral joint (Judet et al. Citation1994, 1996). In spite of these differences, the clinical results appear to be similar with both types of prosthesis.
Moro et al. (Citation2001) reported capitellar osteopenia and radiolucency surrounding the implant stem in 20 and 17 of implants, after a mean follow-up in a series of 25 patients with an acute unreconstructable radial head fracture treated with a cement-less monobloc titanium prosthesis. The long-term implications of these findings are unknown. At the time of follow-up, 17 patients had a good or excellent result and 8 had a fair or poor result. Ashwood et al. (Citation2004) reported a series of 16 patients who were also treated with a titanium monoblock prosthesis. They reported good or excellent results in 13 patients and fair results in 3 patients. They reported no radiolucency around the stem, and no capitellar erosion at 3-year follow-up.
Judet et al. (Citation1996) reported a series of 12 patients who were treated with a cemented bipolar prosthesis for Mason type III fractures. At an average follow-up time of 4 years, no radiolucency or capitellar erosion was seen. Results were good or excellent in 10 patients, and fair in 2. Smets et al. (Citation2000) reported a series of 15 patients, 13 of whom were treated for an acute type III fracture. The 2 remaining patients were treated for chronic problems after radial head fracture. Overall, they reported good or excellent results in 10 patients, and fair or poor results in 5 at a mean follow-up of 2 years. In 1 patient, the prosthesis was removed because of severely reduced elbow function. There were no signs of loosening, subluxation or fracture of the prosthesis, but 3 patients developed wrist pain. Long-term bipolar radial head prosthesis survival rates are currently not available.
Conclusion
All patients in our series had clinical signs of severe elbow instability after previous radial head resection and/or failed ORIF for a type III or IV radial head fracture. Clinically and radiographically, our results are similar to those reported in the literature, and suggest that in the short term, radial head prosthesis is a viable option for patients with instability after failed ORIF or radial head resection for radial head fractures. All patients in our study will be reevaluated after 5 and 10 years. Longer-term follow-up will be required in order to come to more definitive conclusions regarding the use of the bipolar radial head prosthesis.
No competing interests declared.
- Ashwood N, Bain G I, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. J Bone Joint Surg (Am) 2004; 86: 274–80
- Carr C R, Howard J W. Metallic cap replacement of radial head following fracture. West J Surg Obstet Gynecol 1951; 59: 539–46
- Cherry J C. Use of acrylic prosthesis in the treatment of fracture of the head of the radius. J Bone Joint Surg (Br) 1953; 35-B: 70–1
- de Boer Y A, van den Ende C H, Eygendaal D, Jolie I M, Hazes J M, Rozing P M. Clinical reliability and validity of elbow functional assessment in rheumatoid arthritis. J Rheumatol 1999; 26: 1909–17
- de Boer Y A, Hazes J M, Winia P C, Brand R, Rozing P M. Comparative responsiveness of four elbow scoring instruments in patients with rheumatoid arthritis. J Rheumatol 2001; 28: 2616–23
- Essex-Lopresti P. Fractures of the radial head with distal radioulnar dislocation; report of two cases. J Bone Joint Surg (Br) 1951; 33: 244–7
- Gordon M, Bullough P G. Synovial and osseous inflammation in failed silicone-rubber prostheses. J Bone Joint Surg (Am) 1982; 64: 574–80
- Janssen R P, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg (Br) 1998; 80: 231–3
- Johnston G W. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J 1962; 31: 51–6
- Judet T, Massin P, Bayeh P. J. Radial head prosthesis with floating cup in recent and old injuries of the elbow: preliminary results. Rev Chir Orthop Reparatrice Appar Mot 1994; 80: 123–30
- Judet T, Garreau d L, Piriou P, Charnley G. A floating prosthesis for radial-head fractures. J Bone Joint Surg (Br) 1996; 78: 244–9
- Mason M L. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 1954; 42: 123–32
- Mayhall W S, Tiley F T, Paluska D J. Fracture of silastic radial-head prosthesis. Case report. J Bone Joint Surg (Am) 1981; 63: 459–60
- McDougall A, White J. Subluxation of the inferior radioulnar joint complicating fracture of the radial head. J Bone Joint Surg (Br) 1957; 39: 278–87
- Mikic Z D, Vukadinovic S M. Late results in fractures of the radial head treated by excision. Clin Orthop 1983, 181: 220–8
- Moro J K, Werier J, MacDermid J C, Patterson S D, King G J. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg (Am) 2001; 83: 1201–11
- Pomianowski S, Morrey B F, Neale P G, Park M J, O'Driscoll S W. An K N. Contribution of monoblock and bipolar radial head prostheses to valgus stability of the elbow. J Bone Joint Surg (Am) 2001; 83: 1829–34
- Radin E L, Riseborough E J. Fractures of the radial head. A review of eighty-eight cases and analysis of the indications for excision of the radial head and non-operative treatment. J Bone Joint Surg (Am) 1966; 48: 1055–64
- Smets S, Govaers K, Jansen N, Van Riet R, Schaap M, Van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: a multicentric study. Acta Orthop Belg 2000; 66: 353–8
- Sowa D T, Hotchkiss R N, Weiland A J. Symptomatic proximal translation of the radius following radial head resection. Clin Orthop 1995, 317: 106–13
- Swanson A B, Jaeger S H, La Rochelle D. Comminuted fractures of the radial head. The role of silicone-implant replacement arthroplasty. J Bone Joint Surg (Am) 1981; 63: 1039–49
- Timmerman L A, Andrews J R. Arthroscopic treatment of posttraumatic elbow pain and stiffness. Am J Sports Med 1994; 22: 230–5
- Vanderwilde R S, Morrey B F, Melberg M W, Vinh T N. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg (Br) 1994; 76: 78–81
- Wagner C J. Fractures of the head of the radius. Am J Surg 1955; 89: 911–8
- Worsing R A, Jr., Engber W D, Lange T A. Reactive synovitis from particulate silastic. J Bone Joint Surg (Am) 1982; 64: 581–5