Abstract
Background Factors predicting redisplacement in the cast and early complications in distal radial physeal injuries have not been analyzed before.
Patients and methodsWe analyzed 109 consecutive children with displaced physeal fractures of the distal radius treated by manipulation under anesthesia
ResultsAcute carpal tunnel syndrome developed in 2 patients. Posttraumatic swelling necessitating trimming, splitting or removal of the primary circular cast occurred in one-sixth of the patients. Half of the fractures healed in malunion despite an anatomic primary reduction in 85% of the cases. According to logistic regression models, marked initial malposition of the fracture (< 50% displacement or < 20% angulation) was an independent risk factor for complications and redisplacement. Non-anatomic reduction of the fracture was an additional independent risk factor for redisplacement.
InterpretationThe risk of an acute carpal tunnel syndrome should be remembered in patients with marked primary displacement of the fracture. To avoid redislocation, pin fixation of the fracture in patients close to skeletal maturity should be considered if there is a marked initial malposition of the fracture, or if fully anatomic reduction cannot be achieved.
▪
The distal radius is the most common location of physeal injury, comprising around one-fifth of all physeal fractures (Mizuta et al. Citation1987). Traditionally, displaced fractures of the distal radial physis are treated with closed reduction and immobilization. There is no consensus about the appropriate type and duration of immobilization and the acceptable amount of displacement. The reported redisplacement rate is under 10% (Davis and Green Citation1976) and malunited fractures have been shown to remodel well (Aitken Citation1935b). We have found no systematic analysis of factors predicting redisplacement. Serious complications have rarely been reported (Matthews Citation1983, Hernandez and Peterson Citation1986, Mizuta et al. Citation1987, Waters et al. Citation1994). We analyzed fracture characteristics, the treatment protocol, and risk factors for redisplacement and early complications in a consecutive series of distal radial physeal injuries.
Patients and methods
We studied all 109 children (68 boys) with manipulated distal physeal fractures who were treated between 1995 and early 1998 at the Women's and Children's Hospital, Adelaide. The mean age of the patients was 12 (5–16) years. Most of the injuries occurred in association with falls, ballgames or playground equipment; only 11 were caused by motor vehicle accidents. After primary treatment, 7 patients returned to their rural place of residence for further management. Follow-up ranged from 1 week to 2 years (median 6 weeks). Local patients were routinely advised about possible late complications at the time of cast removal. Only patients who were considered to have a high risk of posttraumatic growth problems were scheduled for long-term review, which was performed in 20 children for the following reasons: visible malunion (9), high energy trauma (7), late remanipulation of the fracture (1), and unclear reason (3).
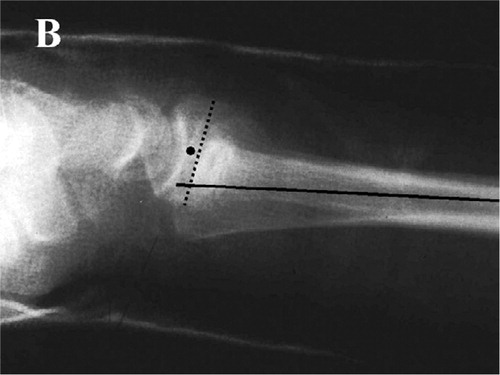
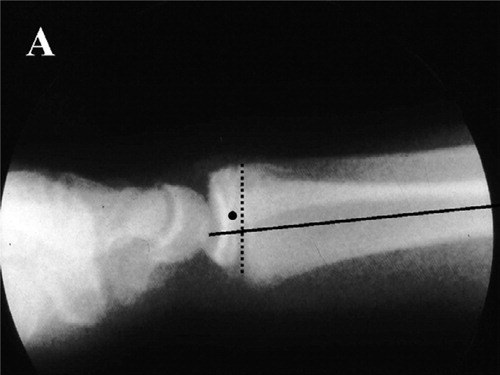
The percentage of displacement and degree of angulation of the epiphysis both in sagittal and frontal planes were measured on primary plain radiographs (). These measurements were repeated after reduction and during follow-up. Associated bony injuries to the ulna and carpal bones were recorded. Cast index defined as the sagittal cast width divided by the coronal cast width at the fracture site was measured in 100/104 patients with a circular cast according to Chess et al. (Citation1994). The position of the wrist in the sagittal plane during immobilization was recorded in lateral radiographs as the angle between the long axes of the third metacarpal bone and the radius (MCRA).
Figure A. Non-anatomic reduction of a dorsally displaced distal radial physeal injury in a 15-year-old boy (10% of dorsal displacement and 5% of dorsal angulation). B. Redisplacement in the cast (30% displacement and12% dorsal angulation), leaving a persistent malunion.
Neurovascular findings, duration of cast immobilization, number of radiographic studies and complications were recorded from case notes. The indications and the timing of fracture manipulation were also analyzed. The ethics committee of the Womem's and Children's Hospital, Adelaide, approved this study.
Differences in continuous variables were evaluated using the Mann-Whitney test. Risk factors predicting complications (compartment syndromes, cast complications and growth arrest) and redisplacement of the fracture in the cast (age, sex, initial displacement, primary reduction, cast index) were analyzed using a logistic regression model (NCSS statistical software version 6.0; NCSS Inc., Kaysville, UT). Displacement exceeding 20% or dorsal angulation of 10° or more at one week were chosen as cut-off points for definition of redisplacement. Odds ratios (OR) and their 95% confidence intervals (95% CI) are shown for each variable. Significance of the covariate terms was tested with likelihood ratio statistics and expressed as exact p-values. Two-tailed p-values of 0.05 or less were considered Significant.
Results
According to the Salter-Harris classification, type I fractures accounted for 12% of the fractures and type II for 88%. Displacement of the epiphysis occurred mainly dorsally in 85% of the fractures, volarly in 6%, and radially or radiodorsally in 9%. The mean percentage of displacement was 45% (median 42%, range 7–100%) and the mean angulation 24° (0–62) in the sagittal plane. Two-thirds of the patients had sustained an associated ulnar injury: processus styloideus avulsion in 46%, buckle fracture in 8%, greenstick fracture in 6%, complete fracture in 3% and a physeal injury in 2%. At presentation, neurapraxia of the median nerve was reported in 10% of the patients, and absent distal pulses in 1 patient.
Nearly all of the children (92%) were treated by manipulation under anesthesia and immobilization in a non-split circular above-elbow cast. A below-elbow cast was used in 4 patients. Percutaneous pin fixation was performed in 5 children (mean age 13.4 (11–15)) years for the following reasons: problems with retention (3), neurovascular compromise at presentation (1), ipsilateral supracondylar humeral fracture (1). The median time from the injury to treatment was 6 (2–84) h, except in 1 case where closed reduction was performed 10 days after the injury. The primary closed reduction under anesthesia was anatomic in 85% of the cases. The mean cast index was 0.76 (0.62–0.93) and the mean MCRA 9 apex dorsal angulation.
The mean duration of immobilization was 5.7 (4–8) weeks. Half of the fractures (48%) healed in malunion, which was usually mild. Redisplacement in the cast did not occur 2 weeks after injury. Percentage displacement at the time of union was more than 20% in 13% of cases and angulation at least 10° in 14% of cases. Age, sex, initial displacement, primary reduction, and cast index were included in logistic regression models to evaluate their independent effect on redisplacement at 1 week (Table). Marked primary displacement (< 50%) and non-anatomic reduction were significant independent risk factors for redisplacement. In addition, there was a tendency towards higher odds ratios for displacement in boys than in girls (Table).
Risk factors for redisplacement of the distal radial physeal injury at 1 week and for complications (compartment syndrome, cast complications or growth arrest) according to logistic regression models
2 urgent compartment decompressions were performed within 24 hours of injury. Both cases were caused by motorbike accidents (primary displacement of the fractures 100% and 58%, with 30° angulation in both patients): a 12-year-old boy developed a combined acute carpal tunnel and forearm compartment syndrome after closed reduction (volar forearm compartment and carpal tunnel pressures < 45 mm Hg); a 14-year-old boy experienced median neuropathy at admission which resolved after reduction and application of a circular cast only to recur within hours (carpal tunnel pressure 70 mm Hg). Circular cast treatment (n = 104) led to complications associated with swelling in 16% of the patients (the cast had to be split in 10 patients, changed in 4 and trimmed in 3). After adjusting for age, sex, primary reduction and cast index, the OR (95% CI) for complications was 19 (6.6–56) in patients with marked primary displacement (< 50%) or angulation (< 20%) as compared to patients with low primary displacement (Table).
One of the primary closed reductions was performed late at 10 days from the injury in a 10-year-old girl (initial displacement 45% and 26° angulation), resulting in clinically in Significant improvement of the position (displacement 30% and 24° angulation). 3 closed remanipulations were done later than one week after the initial treatment (at 8, 10 and 14 days, respectively) leading to improvement of the fracture alignment in the first case only. One open re-reduction was performed 3 weeks after closed reduction, and a growth arrest developed in this case. Retrospectively, 2 of the primary manipulations were deemed unnecessary, with less than 10% of primary displacement and no angulation.
In the 20 children selected for long-term follow-up, clinically Significant growth arrest occurred in a 9-year-old girl and a 12-year-old boy (primary displacement 100% and a non-anatomic reduction of the fracture in both cases). Persistent symptomatic apex volar angulation exceeded 10° in 2 boys who reached skeletal maturity within 6 months of the injury (14.7 and 15.8 years of age at presentation, healing in 20° and 14° angulation, respectively). In 4 other boys (8.6–14.7 years of age) with malunion and with 6-month follow-up radiographs available, the rate of angular correction was 1–2.7° per month.
Discussion
The mean age of occurrence of distal radial physeal injuries has been reported to be 11.9 years in boys and 10.3 in girls (Mann and Rajmaira Citation1990) with Salter-Harris type II fractures comprising most (64–100%) of the fractures (Davis and Green Citation1976, Mizuta et al. Citation1987, Mann and Rajmaira Citation1990, Peterson et al. Citation1994, Cannata et al. Citation2003). According to Aitken (Citation1935a), with few exceptions, the displacement is dorsal. The most common type of associated ulnar injury appears to be an ulnar styloid fracture (Aitken Citation1935a). The fracture characteristics and patient demographics in our series of 109 distal radial physeal injuries are in accordance with these earlier findings.
There is no consensus in the literature about the indications for closed reduction. Conclusions about indications for reduction and the potential for remodeling cannot be drawn from our study. However, 2 of our patients with incomplete remodeling were left with symptomatic clinically relevant malunion, suggesting that anatomic reduction and union of the fracture should be striven for in patients with less than one year of growth remaining. In younger patients, monthly angular correction rates of 1° or more can be expected (Friberg Citation1979).
The technique and the length of immobilization concerning injuries of the distal radial physis vary. A long arm cast is still advocated (Waters Citation2001, Cannata et al. Citation2003), although it does not seem to afford any advantages over a well-molded short arm cast (Chess et al. Citation1994). In many units, acute fractures are generally treated with splints or primary splitting of the circular cast is done routinely in order to allow room for swelling. In our series, the number of patients treated with a short arm cast (4) was too small to allow us to draw any conclusions. The reported duration of immobilization in physeal injuries of the distal radius range from 3 to 6 weeks (Davis and Green Citation1976, Waters Citation2001, Cannata et al. Citation2003).
Redisplacement in the cast has occurred in 8% of the cases reported by Davis and Green (Citation1976) and Cannata et al. (Citation2003), but in Aitkens' (Citation1935a) series over 50% patients had displaced to a poorer position of the fracture at discharge. According to Chess et al. (Citation1994), a well-molded short arm cast to the normal contours of the forearm is highly effective in maintaining reduction in distal-third forearm fractures. Pin fixation after reduction of displaced distal radial physeal fractures has been suggested in patients with Significant soft tissue swelling and symptoms or signs of median nerve dysfunction (Waters et al. Citation1994). To our knowledge, there have been no reports in the literature on complications of pin fixation for this purpose in children.
In our series, the mean cast index (0.76) was slightly higher than the optimum (0.70) (Chess et al. Citation1994). However, after controlling potential confounding factors, cast index below 0.70 did not protect against redisplacement in our series. Instead, marked primary displacement and non-anatomic primary reduction were independent risk factors for redisplacement. These findings indicate that in children with less than 1 year of growth left, percutaneous pin fixation should be considered even after anatomic reduction of the fracture—if the initial displacement has exceeded 50%. Furthermore, in this patient group we advocate percutaneous pin fixation if primary reduction is not fully anatomic.
Serious neurovascular complications, such as acute volar compartment syndrome of the fore arm and acute carpal tunnel syndrome, have been reported in skeletally immature patients with injuries of the distal radial physis (McClain and Wissinger Citation1976, Hernandez and Peterson Citation1986, Waters et al. Citation1994). Our findings confirm that markedly displaced distal radial physeal fractures are at risk of acute median nerve compression. Both of our patients with acute compartment syndromes had sustained severely displaced fractures in motor-bike accidents. Apart from the initial high-energy trauma, the application of a constrictive cast contributed to this complication in 1 of these 2 children. A routine neurological examination should be performed in all patients with distal radial physeal injuries. This examination must be repeated frequently in patients with high-energy trauma, marked swelling or abnormal initial neurological findings.
The reported incidence of growth arrest of the distal radius varies from 1% to 7% (Davis and Green Citation1976, Lee et al. Citation1984, Cannata et al. Citation2003). Aitken (Citation1935a or b?) stated that damage of the growth plate occurs at the time of injury rather than being iatrogenic, and that repeated manipulations add little, if anything, to the trauma. This is in accord with the study of Cannata et al. (Citation2003) who did not record any growth disturbances in patients with remanipulations. Valid conclusions about the incidence of growth arrest cannot be made based on our study, since routine radiographic follow-up was not performed. However, our results suggest that the incidence of growth arrest in distal physeal injuries of the radius is at least 2%.
We advocate awareness of the possibility of neurovascular complications in association with markedly displaced fractures of the distal radial physis. Percutanous pin fixation should be considered in patients close to skeletal maturity with Significant malposition of the fracture, or if fully anatomic primary reduction cannot be attained.
No competing interests declared.
- Aitken A. The end results of the fractured distal radial epiphysis. J Bone Joint Surg 1935a; 17: 302–8
- Aitken A. Further observations on the fractured distal radial epiphysis. J Bone Joint Surg 1935b; 17: 922–7
- Cannata G, De Maio F, Mancini F, Ippolito E. Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma 2003; 17: 172–80
- Chess D G, Hyndman J C, Leahey J L, Brown D C S, Sinclair A M. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop 1994:; 14: 211–3
- Davis D R, Green D P. Forearm fractures in children. Pitfalls and complications. Clin Orthop 1976, 120: 172–84
- Friberg K S I. Remodeling after distal forearm fractures in children. III. Correction of residual angulation in fractures of the radius. Acta Orthop Scand 1979; 50: 741–9
- Hernandez J, Peterson H A. Fracture of the distal radial physis complicated by compartment syndrome and premature physeal closure. J Pediatr Orthop 1986; 6: 627–30
- Lee B S, Esterhai J L, Das M. Fractures of the distal radial epiphysis. Characteristics and surgical treatment of premature, post-traumatic epiphyseal closure. Clin Orthop 1984, 185: 90–6
- Mann D C, Rajmaira S. Distribution of physeal and non-physeal fractures in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop 1990; 10: 713–6
- Matthews L S. Acute volar compartment syndrome secondary to distal radius fracture in an athletic: a case report. Am J Sports Med 1983; 11: 6–7
- McClain E J, Wissinger H A. The acute carpal tunnel syndrome: nine case reports. J Trauma 1976; 16: 75–8
- Mizuta T, Benson W M, Foster B K, Paterson D C, Morris L L. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop 1987; 7: 518–23
- Peterson H A, Madhok R, Benson J T, Ilstrup D M, Melton L J. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop 1994; 14: 423–30
- Waters P M. Distal radius and ulna fractures. Fractures in children, J H Beaty, J R Kasser. Lippincott Williams & Wilkins, Philadelphia 2001; 385–403
- Waters P M, Kolettis G J, Schwend R. Acute median neu-ropathy following physeal fractures of the distal radius. J Pediatr Orthop 1994; 14: 173–7