Abstract
Background Vascularized soft tissue transfer may give better results of treatment of infected nonunions of the tibia.
Methods 6 patients with infected nonunion of the tibia and combined soft tissue (70–170 cm2) and bony (5–8 cm) defects underwent staged reconstruction. Initial surgery consisted of soft tissue and bone debridement, external fixation, filling of the bony defect with a gentamicin-impregnated cement spacer, and reconstruction of the soft tissue with a free microsurgical muscle flap and skin graft. Second-stage surgery consisted of removal of the cement spacer and osseous reconstruction with nonvascularized bone graft.
Results All patients except 1 achieved full weight-bearing and radiographic consolidation after 7–10 months. This patient required repeated bone grafting and internal plate fixation to heal. There were no cases of recurrence of infection at the latest follow-up, after a mean of 3 (1.5–5) years.
Interpretation Staged reconstruction with free vascularized soft tissue transfer and conventional bone grafting within a cement-induced membrane is a low-risk surgical strategy resulting in a high rate of bone healing.
▪
Recurrence of bone infection and lack of bone healing are the two major complications following operations for infected nonunion of the tibia (Weiland et al. Citation1984, Ekkernkamp et al. Citation1996).
The reasons are mainly insufficient bone debridement, incorrect selection of antibiotic, or inappropriate timing and technique for the bone reconstruction. Timing and type of bone reconstruction vary between authors (Moore and Weiland Citation1986, Maurer and Dillin Citation1987, Gordon and Chiu Citation1988, Zwipp et al. Citation1989, Maini et al. Citation2000). Vascularized soft tissue transfer has provided a major advance in the management of infected tibial nonunion surrounded by devitalized tissues (Musharafieh et al. Citation1999). The resulting improved local blood supply favors both antibiotic delivery and bone healing (Holden Citation1972). We describe 6 patients with infected nonunion of the tibia who were treated with staged surgery, including free vascularized soft tissue transfer and conventional bone graft, as first described by Masquelet et al. (Citation2000).
Patients and methods
Between 1997 and 2003, 6 patients (5 males) underwent a two-stage reconstruction to treat an infected nonunion of the tibia (). All patients were treated by the senior author (CED). The mean age at the time of the first stage of reconstruction was 49 (37–61) years. There were 2 isolated tibial fractures and 4 fractures of both the tibia and the fibula. The patients had undergone an average of 2.3 (0–4) operations before being referred to us. The delay between the occurrence of the bone infection and the treatment at our institution ranged from 1 to 6 months. The nonunion was located in the distal third of the tibia in 5 patients, and in the middle third in 1 patient. 2 patients (cases 4 and 5) had additional injuries requiring concomitant operations at our institution. Case 4 required a popliteal artery reconstruction with a saphenous vein graft because of an occlusion of the popliteal artery due to the initial injury.
Table 1. Clinical data before the first stage of reconstruction
Our treatment was performed in two stages (4 surgical interventions): the first one was to treat the infected bone and the second one to reconstruct the bony defect. After an initial thorough soft tissue and bone debridement, the tibia was stabilized with an external fixator. Deep swab cultures were taken. Following this operation, the dressing was changed and the wound copiously irrigated on a daily basis. When the culture results were known, the patients underwent a second procedure. Any remaining devitalized tissues were removed. The bony defect was filled with a Palacos gentamicin-impregnated cement spacer. The soft tissue was reconstructed with a free microsurgical muscle flap. The flap was covered with a split-thickness skin graft. Systemic antibiotic treatment was given at the time of wound coverage, and the patients were given further oral antibiotics for 3 months. Creactive protein (CRP) level was determined 5 days after cessation of antibiotic treatment. Patients proceeded with the second-stage reconstruction if CRP was less than 10 mg/L. If the CRP was greater than 10 mg/L, the patient was given oral antibiotics for 6 more weeks, and the CRP determination was then repeated.
The second-stage surgery consisted of removing the cement spacer, with preservation of the induced membrane formed at the spacer surface, and filling the bony defect with iliac crest cortico-cancellous bone graft within the membrane. Allograft was added if insufficient iliac bone graft was available. Previous antibiotic therapy was continued for 6 more weeks postoperatively. Patients were allowed to bear 10 kg of weight in the external fixator. The external fixator was removed after clear evidence of bone healing on radiographs. Complete healing was clinically defined as pain-free full weight bearing after removal of the external fixator.
Results
Deep swab cultures taken during the initial surgery were positive in all patients, and revealed the presence of Staphylococcus aureus(n = 3), Enterobacter (n = 2), Pseudomonas aeruginosa(n = 2), Clostridium difficile(n = 1), and ßhemolytic Streptococcus(n = 1). All organisms were sensitive to gentamicin. Cultures from 4 patients grew a single organism. 1 patient had 2 organisms present, and 1 patient was positive for 3 organisms. 1 patient received a broadspectrum oral antibiotic. 5 patients received oral combination therapy with ciprofioxacin and rifampicin or clindamycin.
The length of the bony defect after debridement ranged from 5 to 8 cm (). The bone defect was fully segmental in 3 patients, and in 3 patients a loose contact between the bone stumps (less than one-quarter of the diameter of the tibia) was present. The soft tissue defect ranged from 70 to 170 cm2. The choice of muscle transfer was based on the size of the defect. We used the serratus anterior in 4 cases ( and ) and the latissimus dorsi in 2 cases. All flaps and skin grafts healed uneventfully. 5 patients received autogenous bone graft from bilateral iliac crests. A mixture of 50% allograft and 50% autogenous graft was used for the other patient, because of insufficient iliac bone graft due to previous harvest. We performed additional procedures in 3 patients. This consisted of 3 ORIF of the fibula and 1 reconstruction of the peroneal nerve with a nerve graft (case 5). The mean hospital stay for the first stage of reconstruction was 28 (21–42) days. The mean time between the first and second-stage of reconstruction was 105 (91–119) days. The mean hospital stay for the second stage of reconstruction was 10 (5–14) days. The external fixators were removed after a mean period of 7.3 (7–10) months. Superficial pin infection, observed in 2 cases, healed after intensive wound care. There was no pin loosening. All patients, except case 2, achieved pain-free full weight bearing after removal of the external fixator. The range of motion of both the knee and the ankle joint was equivalent to that on the contralateral side at the time of latest follow-up. No cases had any sign of recurrence of the osteomyelitis after 3 (1.5–5) years.
Figure 1. Condition of soft tissue in case 4:chronic wound surrounded by scarred soft tissues on admission (A).Soft tissue defect after debridement and prior to coverage with a serratus anterior free flap.The cement spacer inlay has been implanted after a thorough bone debridement and stabilized with wires to the bony stumps.Tibial shaft stabilization is obtained with an external fixator (B).Complete skin graft healing over the free flap prior to removal of the cement spacer and bone reconstruction with iliac crest bone (C).
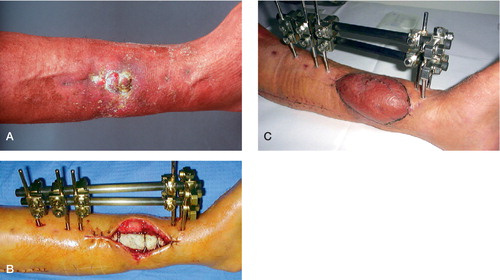
Figure 2. Case 4.Infected nonunion of the distal third of the tibia and nonunion of the fibula.The external fixator that was used initially had been removed before the patient was referred to us (A).After completion of the first-stage surgery (B).Bone healing at the last follow-up, 40 months after second-stage surgery (C).
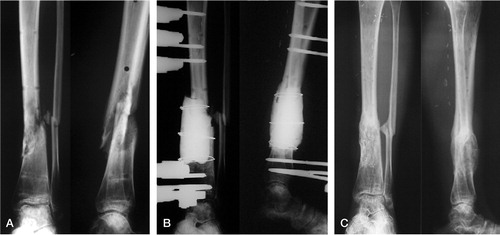
Table 2. Procedures and follow-up
There were several complications of treatment. Case 5 had a thrombosis of the free flap anastomoses, requiring revision. 3 patients developed a hematoma at the free flap recipient site, and one at the free flap donor site, all of which required operative drainage. Case 2 sustained a refracture after removal of the external fixator, 10 months after bone grafting. The patient was treated with an Ilizarov fixator for 8 months without union. 18 months after the initial procedure, the patient underwent autogenous bone grafting, harvested from both proximal tibias, and an internal fixation with a titanplate. The patient was able to bear full weight and there was radiographic consolidation at 3 months. 1 patient had a winging of the scapula due to the free serratus anterior harvest, without any functional limitation.
Discussion
An infected nonunion of the tibia requires a strategy for both curing the osteomyelitis and for creating an environment to support the healing of the reconstructed bone. Resection of the infected and devitalized tissues, in combination with high concentrations of local antibiotics, have been used with success to treat osteomyelitis—both clinically and experimentally (Buchholz and Engelbrecht Citation1970, Wahlig et al. Citation1978, Hedström et al. Citation1980, Fitzgerald Citation1983). We used commercially available gentamicin-impregnated cement to preserve the space for secondary bone reconstruction. We used gentamicin, as all organisms were sensitive based on deep swab cultures. Other antibiotics such as vancomicin can also be mixed into the cement to prepare beads or custom spacers, depending on the results of culture (Flick et al. Citation1987). We used post-operative antibiotic therapy in all patients. It was our policy to wait for the results of deep wound culture before proceeding to soft tissue reconstruction, so that an appropriate therapy was started at the time of wound coverage.
Muscle is more effective than fasciocutaneous flaps to cover infected bone (Mathes Citation1982, Mathes et al. Citation1982). Large defects or defects of the distal third of the leg—as in this series of patients— require coverage with free muscle flaps, because local flaps are unavailable or too small (Gordon et al. Citation1982).
Three main options are available to handle a bone defect of the tibia. Bone transport has been used to treat infected nonunion of the tibia, with high rates of bone healing (Cattaneo et al. Citation1992, Hosny and Shawky Citation1998). However, the mean duration of treatment exceeded 9 months in the case of segmental defect, and about one-fifth of the patients suffered recurrent postoperative drainage, meaning that the infection was not resolved. While limited bony defects may be reconstructed with autogenous iliac bone graft, free vascularized bone transplant has been recommended for reconstruction of diaphyseal defects of greater than 6–8 cm (Sowa and Weiland Citation1987). Christian et al. (Citation1989) and Masquelet et al. (Citation2000) successfully used cancellous bone grafts in tibial defects of up to 25 cm, however. Recently, it has been shown clinically that the cement spacerinduced membrane may favor healing of the cancellous bone graft placed within it (Pelissier et al. Citation2002). Moreover, in rabbits, Pelissier et al. (Citation2004) found the production of vascular endothelial growth factor, transforming growth factorß1 and bone morphogenetic protein-2 into the spacer-induced membrane. This may explain the lack of bone graft resorption and the strong bone healing observed in the 5 patients who received a bone autograft within the cementinduced membrane.
The only patient who received a mixed autograft and allograft did not heal, even after prolonged immobilization with an external fixator. Thus, in patients with previous iliac crest bone harvests, the greater trochanter and proximal tibia might be used as alternative donor sites for cancellous bone that is sufficient to bridge large diaphyseal defects (Lindequist Citation1989, Alt et al. Citation2003).
Reconstruction with vascularized free bone transfer provides immediate structural support, is rapidly incorporated and able to form new bone, and may also improve the vascularity of the recipient area (Pirela-Cruz and DeCoster Citation1994). However, unreliability of graft hypertrophy and a high rate of late fractures in free vascularized fibula transfers has been reported (DeCoster et al. Citation2004). Banic and Hertel (Citation1993) used double vascularized fibulas and additional cancellous bone grafts for reconstruction of diaphyseal defects ranging from 6 to 18 cm, to rapidly obtain stability of the reconstructed bone. This resulted in complete bone healing within 3 months in 6 of 7 patients. In 1 patient, a steal phenomenon resulting from the combined free vascularized fibula and free latissimus dorsi transfers used for the reconstruction, resulted in a progressive ischemic necrosis of the foot requiring a below-knee amputation. Composite free tissue transfers consisting of vascularized bone and muscle have been proposed to replace combined free transfers when both tissues must be reconstructed (Ueng et al. Citation1996). Composite free tissue transfers do not induce a faster rate of bone healing compared to the conventional bone graft within a cementinduced membrane, and the complication rate for vascularized bone transfers is higher than for conventional bone grafts (Pelissier et al. Citation2003).
We thank T. O’Brian and B. Fuchs for critical reading of the manuscript.
No competing interests declared.
- Alt V, Meeder P J, Seligson D, Schad A, Atienza C, Jr. The proximal tibia metaphysis: a reliable donor site for bone grafting?. Clin Orthop 2003, 414: 315–21
- Banic A, Hertel R. Double vascularized fibulas for reconstruction of large tibial defects. J Reconstr Microsurg 1993; 9: 421–8
- Buchholz H W. Engelbrecht H. Ueber die Depotwirkung einiger Antibiotica bei Vermischung mit dem Kunstharz Palacos. Chirurg 1970; 41: 511–5
- Cattaneo R, Catagni M, Johnson E E. The treatment of infected nonunions and segemntal defects of the tibia by the methods of Ilizarov. Clin Orthop 1992, 280: 143–52
- Christian E P, Bosse M J, Robb G. Reconstruction of large diaphyseal defects, without free fibular transfer, in Grade-IIIB. J Bone Joint Surg (Am) 1989; 71: 994–1004
- DeCoster T A, Gehlert R J, Mikola E A, Pirela-Cruz M A. Management of posttraumatic segmental bone defects. J Am Acad Orthop Surg 2004; 12: 28–38
- Ekkernkamp A, Muhr G, Josten C. Die infizierte Pseudar-throse. Unfallchirurg 1996; 99: 914–24
- Fitzgerald R H, Jr. Experimental osteomyelitis: description of a canine model and the role of depot administration of antibiotics in the prevention and treatment of sepsis. J Bone Joint Surg (Am) 1983; 65: 371–80
- Flick A B, Herbert J C, Goodell J, Kristiansen T. Noncommercial fabrication of antibiotic-impregnated polymethylmethacrylate beads. Technical note. Clin Orthop 1987, 223: 282–6
- Gordon L, Chiu E J. Treatment of infected non-unions and segmental defects of the tibia with staged microvascular muscle transplantation and bonegrafting. J Bone Joint Surg (Am) 1988; 70: 377–86
- Gordon L, Buncke H J, Alpert B S. Free latissimus dorsi muscle flap with split-thickness skin graft cover: a report of 16 cases. Plast Reconstr Surg 1982; 70: 173–8
- Hedström S A, Lidgren L, Torholm C, Önnerfalt R. Antibiotic containing bone cement beads in the treatment of deep muscle and skeletal infections. Acta Orthop Scand 1980; 51: 863–9
- Holden C E. The role of blood supply to soft tissue in the healing of diaphyseal fractures. An experimental study. J Bone Joint Surg (Am) 1972; 54: 993–1000
- Hosny G, Shawky M S. The treatment of infected non-union of the tibia by compression-distraction techniques using the Ilizarov external fixator. Int Orthop 1998; 22: 298–302
- Lindequist S. Bone grafting in femoral neck fractures: results in 28 cases operated on with multiple pinning and cancellous bone grafting. Arch Orthop Trauma Surg 1989; 108: 116–8
- Maini L, Chadha M, Vishwanath J, Kapoor S, Mehtani A, Dhaon B K. The Ilizarov method in infected nonunion of fractures. Injury 2000; 31: 509–17
- Masquelet A C, Fitoussi F, Begue T, Muller G P. Reconstruction des os longs par membrane induite et autogreffe spongieuse. Ann Chir Plast Esthet 2000; 45: 346–53
- Mathes S J. The muscle flap for management of osteomyelitis. N Engl J Med 1982; 306: 294–5
- Mathes S J, Alpert B S, Chang N. Use of the muscle flap in chronic osteomyelitis: experimental and clinical correlation. Plast Reconstr Surg 1982; 69: 815–29
- Maurer R C, Dillin L. Multistaged surgical management of posttraumatic segmental tibial bonre loss. Clin Orthop 1987, 216: 162–70
- Moore J R, Weiland A J. Free vascularized bone and muscle flaps for osteomyelitis. Orthopedics 1986; 9: 819–24
- Musharafieh R, Osmani O, Musharafieh U, Saghieh S, Atiyeh B. Efficacy of microsurgical free-tissue transfer in chronic osteomyelitis of the leg and foot: review of 22 cases. J Reconstr Microsurg 1999; 15: 239–44
- Pelissier P, Martin D, Baudet J, Lepreux S, Masquelet A C. Behaviour of cancellous bone graft placed in induced membranes. Br J Plast Surg 2002; 55: 596–8
- Pelissier P, Boireau P, Martin D, Baudet J. Bone reconstruction of the lower extremity: complications and outcomes. Plast Reconstr Surg 2003; 111: 2223–9
- Pelissier P, Masquelet A C, Bareille R, Pelissier S M, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004; 22: 73–9
- Pirela-Cruz M A, DeCoster T A. Vascularized bone grafts. Orthopedics 1994; 17: 407–12
- Sowa D T, Weiland A J. Clinical applications of vascularized bone autografts. Orthop Clin North Am 1987; 18: 257–73
- Ueng S W, Chuang D C, Cheng S L, Shih C H. Management of large infected tibial defects with radical debridement and staged doublerib composite free transfer. J Trauma 1996; 40: 345–50
- Wahlig H, Dingeldein E, Bergmann R, Reuss K. The release of gentamicin from polymethylmethacrylate beads. An experimental and pharmacokinetic study. J Bone Joint Surg (Br) 1978; 60: 270–5
- Weiland A J, Moore J R, Daniel R K. The efficacy of free tissue transfer in the treatment of osteomyelitis. J Bone Joint Surg (Am) 1984; 66: 181–93
- Zwipp H, Flory P, Berger A, Tscherne H. Combination of cancellous bone grafts and free microvascular bone trans-plantation in large osseous defects. Handchir Mikrochir Plast Chir 1989; 21: 235–45
