Abstract
Introduction Today, percutaneous or open arthrodesis of the ankle, using one or several screws for fixation, is a common method for treatment of the rheumatic ankle. However, there is very little information in the literature on the reliability of the method.
Methods We performed a retrospective radiographic and clinical study on 35 ankles of 35 patients. Function was evaluated using the Mazur and AOFAS scores. For evaluation of activity of the rheumatic disease, we used the HAQ score.
Results 31 ankles had healed—26 at the first attempt and 5 after repeat arthrodesis. There was no difference between 13 cases operated on percutaneously and 22 cases operated on with open technique with respect to radiographic healing. Mean AOFAS total score was 56 of possible 86 points. The AOFAS total score correlated with the severity of the rheumatic disease. 20 patients were satisfied with the result, 12 were somewhat satisfied and 3 patients were dissatisfied although the ankle in 2 of these 3 patients had fused.
Interpretation The use of compression screws for fusion of the rheumatic ankle does not appear to give acceptable results regarding healing and function.
▪
Percutaneous or open arthrodesis of the ankle using one or several screws for fixation is currently a common method for treatment of the rheumatic ankle (Lauge-Pedersen et al. Citation1998, Mann and Rongstad Citation1998, Kennedy et al. Citation2003). The reason for this is that external fixation methods mean a more complicated rehabilitation including pin tract infection. However, after both external fixation and the use of compression screws, reported fusion rates in rheumatic ankles have been found to vary between 65% and 97% (Miehlke et al. Citation1997, Nassar and Cracchiolo Citation2001).
We evaluated the mid-term results of primary ankle fusion in rheumatoid arthritis using internal fixation by multiple compression screws—either performed by a percutaneous procedure or an open procedure. We studied the number of healed arthrodeses, hind foot position, wound healing problems, patient satisfaction, and activity.
Patients and methods
Between 1991 and 2002, 57 ankles from 51 patients with rheumatoid arthritis were operated on with an ankle arthrodesis using 2 or 3 compression screws (primary operation). The diagnosis was confirmed in all cases by an experienced rheumatologist using the A.C.R. criteria (Arnett Citation1989). As expected, almost all patients had more or less advanced destruction of the subtalar and mid-tarsal joints.
13 patients (with 14 rheumatoid ankles) had already died by the time of this review, which was undertaken during 2002-2005. 1 patient was unwilling to attend, and 2 patients (with 3 rheumatoid ankles) had not been examined radiographically any later than 6 months after surgery, and had died before a new examination could be performed.
Of the remaining 35 patients, 4 had undergone bilateral ankle arthrodesis with a compression screw technique. We used the MATLAB software to randomly exclude 1 ankle of each patient operated on bilaterally. In 3 of these patients, both ankles had healed, but 1 patient had 1 healed ankle and 1 unhealed. The randomization procedure excluded the healed ankle.
Thus, our study dealt with 35 ankles in 35 patients (30 women) who underwent a complete clinical and radiographic follow-up. The mean age at surgery was 56 (24–76) years. The average clinical examination took place at mean 7 (2–12) years after surgery and the radiographic examination at 6 (1–14) years. Demographic data are presented in the Table.
Surgical technique
All 35 operations were performed at the University Hospital of Lund by 10 different surgeons. 3 surgeons had performed between 6 and 11 procedures each, whereas 6 surgeons had performed only between 1 and 3. In 13 cases, surgery was undertaken as a percutaneous procedure and in 22 as an open procedure ().
Figure 1. Ankle no.12.Radiographs (A and B) obtained 5 years after percutaneous surgery.The ankle has not become fused.
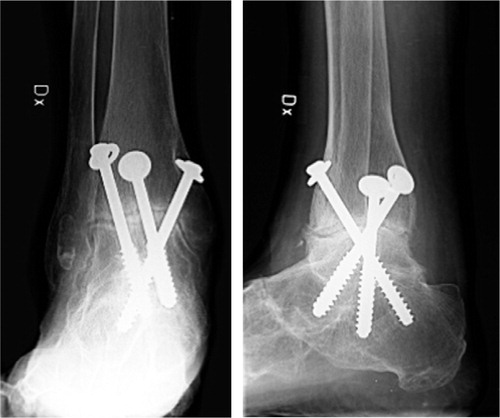
Figure 2. Ankle no.6.Radiographs (A and B) obtained 6 years after percutaneous surgery.The ankle is fused.

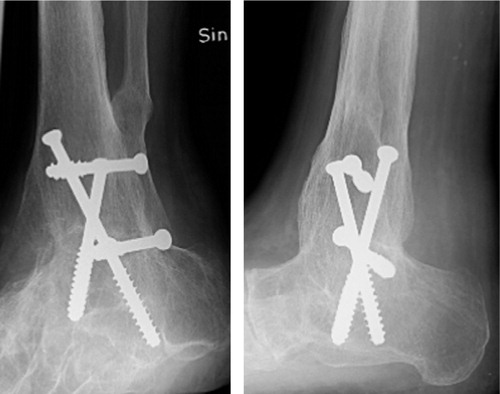
Figure 3. Ankle no.20.Radiographs (A and B) obtained 2 years after open surgery. The ankle is fused.
Surgery was performed using a tourniquet and with the patient in supine position. When the ankle was considered well aligned, screw fixation was performed by a percutaneous technique. Using an image-intensifier, 2 small skin incisions were made. One was placed medially and one laterally, both approximately 10 cm above the ankle joint. Two guide wires were passed trough the joint with the ankle in neutral position, crossing the joint in an oblique mediolateral and lateromedial direction. Two cannulated 7.0-mm, partially threaded, cancellous screws were then introduced over the guide wires. If the fixation was not considered to be stable, one additional screw was inserted from behind and directed anteriorly.
When the ankle was considered unsuitable for percutaneous operation due to valgus or varus malalignment, open surgery was undertaken. In such cases, the joint was exposed through 2 incisions—one longitudinal medial and one curved lateral incision, i.e. according to a modified Adam's technique (Adams Citation1948). The screws were introduced as described above for the closed technique. However, in 2 cases (nos. 14 and 28) the screws were introduced in a retrograde fashion, i.e. from the calcaneus into the tibia. In 11 of the 13 ankles that were operated on with percutaneous technique, the subtalar joints were already radiographically anchylotic or had been destroyed by the rheumatic disease. In 4 of these 11 cases and in the 2 cases with essentially normal subtalar joints, the screws were only fixated in the talus.
In 19 of the 22 ankles operated on with open technique, the subtalar joint was already radiographically anchylotic or had been destroyed by the rheumatic disease. In 8 of these 19 cases, the screws passed the talus into the calcaneus, and in 11 cases they did not. In the 3 cases with essentially normal subtalar joints, the screws were only fixated in the talus. Bone was resected in order to align the ankle and adapt the surfaces. After surgery, the ankle was placed in a lower leg plaster cast for mean 11 (8–14) weeks. Full weight bearing was allowed after 6 (4–10) weeks.
Follow-up
In 2003, a clinical follow-up was undertaken by one of the authors (PM), who had not taken part in any of the operations. The Mazur (Citation1979) and AOFAS (American Orthopaedic Foot and Ankle Society) (Kitaoka Citation1994) ankle scoring systems were used simultaneously. The maximum total and pain scores in the Mazur system are 90 and 50, respectively, and in the AOFAS system 86 and 40 points, respectively. Patient satisfaction was reported as satisfied, somewhat satisfied or dissatisfied according to Makwana et al. (Citation1995). For evaluation of the current activity of rheumatic disease, the HAQ score (Health Assessment Questionnaire) (Fries et al. Citation1980) was used. The maximum HAQ score can reach 3.0, which implies a very disabled person. A zero value implies a person without any handicap.
The radiographs were evaluated by one of the other authors (JB), who was unaware of the clinical results at the time of evaluation. He classified the ankles as fused or not fused, based on the presence of bridging bone or not.
Statistics
Descriptive statistics were calculated by Statistica 6.1 software. Mann-Whitney U-test was used for calculation of differences between groups regarding outcome scores. Fisher's exact test was used for comparison of differences in healing rates between groups. A linear regression equation was used to estimate the correlation between the HAQ and AOFAS scores.
Demographic data and outcome of surgery
Results
The results of the clinical and radiographic examinations are presented in the Table.
31 ankles had healed—26 at the first attempt and 5 after repeat arthrodesis. Of the 22 ankles operated on with open technique, 16 healed primarily and 5 after repeat arthrodesis. Of the 13 ankles that were operated on with percutaneous technique, 10 healed after the operation and none of the 3 unhealed cases were reoperated. There was no statistically significant difference between the cases operated on with percutaneous technique and those operated on with open technique in terms of either primary healing or final radiographic healing (p = 0.6 and 0.1, respectively). Whether or not the screws passed the talar bone into the calcaneus did not influence primary healing (p = 0.5).
The mean Mazur total score for all 35 cases was 55 (23–73) of 90 possible points, and the corresponding pain score was 40 (10–50) out of 50 possible points. The mean AOFAS total score was 56 points (15–85) of 86 possible and the corresponding pain score was 29 (0–40) out of 40 possible. The mean HAQ score was 1.8 (0.1–2.9) points. The severity of the rheumatic disease, expressed as HAQ points, was not significantly different between those who had undergone percutaneous surgery and those who had undergone open surgery (p = 0.2).
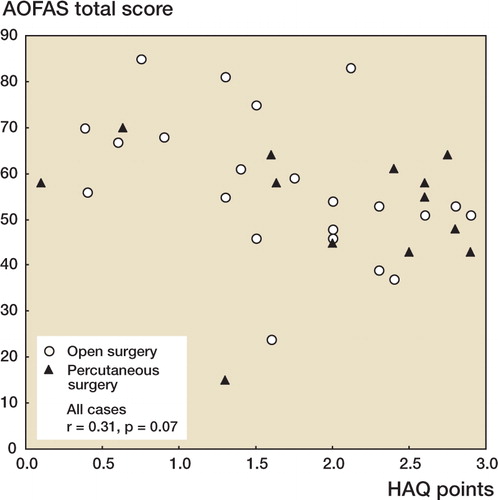
With all 35 cases included, AOFAS total score tended to be correlated with HAQ points (r = 0.31; p = 0.07) (). However, when the 2 outliers were excluded (cases no. 13 and 29), the correlation became statistically significant (r = 0.49; p = 0.004). Case 13 did not heal and had an extremely low total score. Also, this was the only case with a zero pain score. Case 29 had undergone repeat arthrodesis, but healed thereafter.
Figure 4. Scatter plot demonstrating the correlation between the HAQ points and the AOFAS total pain score.Filled symbols represent cases that have undergone percutaneous surgery and unfilled symbols represent those that have undergone open surgery.The outliers are the 2 cases (nos.13 and 29) with an AOFAS score of 15 and 24, respectively.
20 patients were satisfied with the result; of these, 2 had an ankle that had not fused. 12 patients were somewhat satisfied, and of these, 2 had an ankle that was not fused. 3 patients were dissatisfied, even though the ankle was fused in 2 of them. In total, at follow-up there were 8 ankles with a varus malposition between 8° and 10° and 7 ankles with a valgus malposition between 7° and 20°. The angles were measured in supine position with a goniometer. After percutaneous surgery, we observed a malposition in 3 of 13 cases, and in 12 of 22 cases after open surgery.
Complications
Reoperations due to nonhealing:
Patient 14. Reoperated after 21 months with a retrograde intramedullary nail, after which the ankle healed.
Patient 24. Reoperated after 15 months with plates and cannulated screws. Autologous bone was used. The ankle fused.
Patient 28. Reoperated twice before final fusion, the first time after 17 months due to a deep infection and using external fixation. The infection healed, but the ankle did not fuse. It was therefore reoperated a second time 18 months later with a retrograde intramedullary nail. The ankle fused 51 months after the primary operation.
Patient 29. Reoperated on after 16 months, with 2 cannulated screws and the use of autologous bone transplant. The ankle became fused.
Patient 33. Reoperated on after 15 months. 5 cannulated screws were used for fixation of the ankle using both a solid autologous and cancellous bone graft. The ankle healed thereafter.
Other complications:
Patient 19. The patient sustained a spontaneous fracture of the distal tibia, located at the entrance of one of the screws, 6 months postoperatively. The fracture healed under conservative treatment.
Patient 21. A deep infection necessitated removal of the screws, antibiotic treatment and transplantation of a skin graft. The ankle fused without further surgery and the patient reported satisfaction.
Discussion
During the last 2 decades, internal fixation with compression screws has been the main technique for fusion of the ankle joint. However, the reported healing rate of 88–100% refers mainly to patients operated on due to posttraumatic osteoarthrosis (Morgan et al. Citation1985, Scranton Citation1985, Mann et al. Citation1998). There have only been 2 papers dealing specifically with compression screw arthrodesis in patients with rheumatoid arthritis. Crachiolo et al. (Citation1992) reported 13 cases, of which 10 cases resulted in a fused ankle. Kennedy et al. (Citation2003) reported 18 of 20 ankles being fused at the first attempt and another ankle being fused after repeat arthrodesis.
Our results are inferior to those reported by Kennedy et al. (Citation2003). One explanation for this difference may be that in the earlier report, a single surgeon had performed all the operations, whereas 10 surgeons had been involved in our series. Ankle fusion is usually a demanding procedure which would probably benefit from the use of a limited number of well-experienced surgeons.
The number of primarily healed arthrodeses in our series—26 of 35—is also lower than the result obtained after retrograde intramedullary nailing. With the latter technique, we obtained primary healing in 25 of 26 ankles despite the fact that many surgeons were involved (Anderson et al. Citation2005).
There was a negative and significant correlation between functional scores and the activity of the rheumatic disease. This confirms the observations found by our group in a previous study (Anderson et al. Citation2005). The most commonly used scoring systems are thus not ideal for evaluation of foot function in the rheumatic patient.
The mean AOFAS and Mazur total scores at follow-up were both about 10 points lower in the present series than the scores observed after retrograde intramedullary nailing (Anderson et al. Citation2005). Also, the number of satisfied patients was considerably lower in the present series. One may therefore conclude that the method using compression screws is inferior to retrograde intramedullary nailing in this group of patients, especially as the mean HAQ score, reflecting the severity of the rheumatic disease, was 1.8, i.e. the same in both series. One explanation for the superiority of retrograde intramedullary nailing may be that it results in a mechanically more stable fixation than with the use of compression screws (Berend Citation1997).
Funding for this study was received from the Skane County Council's Research and Development Grants.
No competing interests declared.
- Adams C J. Arthrodesis of the ankle joint. J Bone Joint Surg (Br) 1948; 30: 506–11
- Anderson T, Linder, Rydholm U, Montgomery F, Besjakov J, Carlson Å. Tibiotalocalcaneal arthrodesis as a primary procedure using a retrograde intramedullary nail. A report on 26 patients with rheumatoid arthritis. Acta Orthop 2005
- Arnett F C. Revised criteria for the classification of rheumatoid arthritis. Bull Rheum Dis 1989; 38: 1–6
- Berend M E, Glisson R R, Nunley J A. A biomechanical comparison of intramedullary nail and crossed lag screw fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int 1997; 18: 639–43
- Crachiolo A, 3rd, Cimino W R, Lian G. Arthrodesis of the ankle in patients who have rheumatoid arthritis. J Bone Joint Surg (Am) 1992; 74: 903–9
- Fries J F, Spitz P, Kraines R G, Holman H R. Measurement of patient outcome in arthritis. Arthritis Rheum 1980; 23: 137–45
- Kennedy J G, HartyJ A, Casey K, Jan W, Quinlan W B. Out-come after single technique ankle arthrodesis in patients with rheumatoid arthritis. Clin Orthop 2003, 412: 131–8
- Kitaoka H B, Alexander I J, Adelaar R S, Nunley J A, Myer-son M S, Sanders M. Clinical rating system for the ankle– hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int 1994; 15: 349–53
- Lauge-Pedersen H, Knutson K, Rydholm U. Percutaneus ankle arthrodesis in the rheumatoid patient without debridement of the joint. The Foot 1998; 8: 226–9
- Makwana N K, Morrison P, Jones C B, Kirkup J. Salvage operations after failed total ankle replacement. The Foot 1995; 5: 180–4
- Mann R A, Rongstad K M. Arthrodesis of the ankle: A critical analysis. Foot Ankle Int 1998; 19: 3–9
- Mazur J M, Schwartz E, Simon S R. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg (Am) 1979; 61: 964–75
- Miehlke W, Geschwend N, Rippstein P, Simmen B R. Compression arthrodesis of the rheumatoid ankle and hindfoot. Clin Orthop 1997, 340: 75–86
- Morgan C D, Henke J A Bailey R W, Kaufer H. Long-term results of tibiotalar arthrodesis. J Bone Joint Surg (Am) 1985; 67: 546–50
- Nassar J, Cracchiolo A III. Complications in surgery of the foot and ankle in patients with rheumatoid arthritis. Clin Orthop 2001, 391: 140–52
- Scranton P E, Jr. Use of internal compression in arthrodesis of the ankle. J Bone Joint Surg (Am) 1985; 67: 550–5
