In January 1997, a 62-year-old man was diagnosed with a hypernephroma of the right kidney and bilateral pulmonary metastases. He underwent a right nephrectomy as initial surgery. Histology showed a 16-mm granular cell renal carcinoma of the lower part of the right kidney. He received chemotherapy with α-interferon for the following 11 months. In November 1999, CT showed a 4-cm osteolytic lesion from the right posterior inferior iliac spine to the roof of the acetabulum. The medial and lateral bony borders were partially destroyed and the lesion was therefore classified as class III according to Harrington (Citation1981).
The patient underwent local radiation therapy in December 1999, and a second course of chemotherapy with vinblastine. Immune modulation therapy with α-interferon showed a partial remission of the pulmonary metastases. In addition, he received intravenous treatment with bisphosphonates.
In February 2000, the patient sustained a pathological fracture of the right iliac wing with medial and cranial dislocation of the entire acetabulum.A second course of radiation therapy was given in August 2000.
In April 2001, the patient presented with an advanced right periacetabular fracture (). A periacetabular reconstruction and a total hip arthroplasty was performed. A reinforcement cage (Burch-Schneider, Protek, Switzerland) was combined with a cemented standard stem with a 28-mm metal ball head and cemented polyethylene inlay. After reduction of the fracture, structural continuity was achieved and reinforced with 3 Steinmann pins using the compound osteosynthesis technique, i.e. the pins were entirely covered with bone cement, which filled the gap. 1 pin was inserted from the superior iliac crest to the cranial part of the acetabulum, and 2 pins through the center of the acetabulum. One of these pins was unthreaded (). The pins were cut off flush with the iliac crest.
Figure 1. Preoperatively, advanced metastatic destruction of the right acetabulum with a pathological fracture and medial and cranial dislocation of the acetabulum.

Figure 2. Periacetabular reconstruction with modified Harrington technique and total hip replacement. Unthreaded pin is marked with an arrow.

The patient quickly regained pain-free walking using 2 crutches. At routine follow-up (6 months), he was satisfied with the functional result ().
Figure 3. Six months postoperatively: note the appearance of the most medial pin projecting beyond the medial acetabular border (marked with an arrow). There was no definite pin migration at that point.

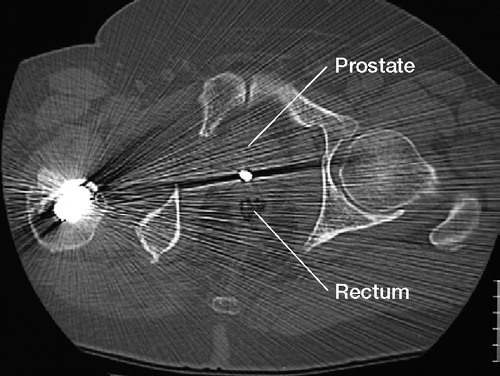
In November 2001, the patient suffered an episode of transient hematuria and was treated under the suspicion of urinary tract infection. An abdominal sonography showed mild hepatic steatosis but no other abnormalities. 9 months after surgery, a routine pelvic radiograph () showed migration of one of the Steinmann pins. A CT scan was performed, which showed the dislocation of the pin into the pelvic cavity very close to the bladder, the anterior side of the rectum and the prostate (). There was no sign of any penetration of the neighbouring organs. The dislocated pin was removed under general anesthesia by a modified ilioinguinal approach without difficulty. The histological findings showed no signs of local tumor recurrence. The peri- and postoperative recovery was unremarkable, and the patient was discharged 7 days later.
Figure 5. CT scan 10 months after surgery; transverse plane of the pelvis just below the level of the hip joint. Note the projection of the tip of the Steinmann pin crossing the narrow space between rectum and prostate, overlapped with mental artefacts of the pin.
When the patient was latest seen, 13 months postoperatively, he was painfree and walked without crutches.
Discussion
Metastatic bone destruction of the acetabulum is classified by most authors according to Harrington (Citation1981). Class III is a lesion with deficiencies in the lateral cortices and the superior part of the wall, as in our case. A number of reconstruction techniques have been described with total hip arthroplasty using support rings or other materials such as the saddle prosthesis, with or without reinforcement with pelvic pins and bone cement, allografts and autografts (Harrington Citation1981, Citation1992, Levy et al. Citation1982, Walker Citation1993, Aboulafia et al. Citation1995, Allan et al. Citation1995, Stark and Bauer Citation1996, Kusuzaki et al. Citation1998, Durr et al. Citation1999, Citation2002, Vena et al. Citation1999, Nilsson et al. Citation2000).
In 1981, Harrington described his cement and pin technique for surgical treatment of patients with periacetabular metastatic disease (class III). Since Harrington's report, several authors have published their experience of his technique (Walker Citation1993, Vena et al. Citation1999, Kunisada and Choong Citation2000, Marco et al. Citation2000, Nilsson et al. Citation2000). In all reports, either threaded Steinman pins or cancellous screws were used and none of the authors found a pin dislocation. We usually use threaded Steinmann pins only. In this case, we used an unthreaded pin because of lack of availability of other pins at the time of surgery. We conclude that unthreaded pins should not be used in the treatment of metastatic pelvic destruction.
- Aboulafia A J, Buch R, Mathews J, Li W, Malawer M M. Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumors. Clin Orthop 1995, 314: 203–13
- Allan D G, Bell R S, Davis A, Langer F. Complex acetabular reconstruction for metastatic tumor. J Arthroplasty 1995, 10: 301–6
- Durr H R, Maier M, Pfahler M, Baur A, Refior H J. Surgical treatment of osseous metastases in patients with renal cell carcinoma. Clin Orthop 1999, 367: 283–90
- Durr H R, Muller P E, Lenz T, Baur A, Jansson V, Refior H J. Surgical treatment of bone metastases in patients with breast cancer. Clin Orthop 2002, 396: 191–6
- Harrington K D. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg (Am) 1981; 63: 653–64
- Harrington K D. The use of hemipelvic allografts or auto-claved grafts for reconstruction after wide resections of malignant tumors of the pelvis. J Bone Joint Surg (Am) 1992; 74: 331–41
- Kunisada T, Choong P F. Major reconstruction for periacetabular metastasis: early complications and outcome following surgical treatment in 40 hips. Acta Orthop Scand 2000; 71: 585–90
- Kusuzaki K, Shinjo H, Kim W, Nakamura S, Murata H, Hirasawa Y. Resection hip arthroplasty for malignant pelvic tumor. Outcome in 5 patients followed more than 2 years. Acta Orthop Scand 1998; 69: 642–51
- Levy R N, Sherry H S, Siffert R S. Surgical management of metastatic disease of bone at the hip. Clin Orthop 1982, 169: 62–9
- Marco R A, Sheth D S, Boland P J, Wunder J S, Siegel J A, Healey J H. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg (Am) 2000; 82: 642–51
- Nilsson J, Gustafson P, Fornander P, Ornstein E. The Harrington reconstruction for advanced periacetabular meta-static destruction: good outcome in 32 patients. Acta Orthop Scand 2000; 71: 591–6
- Stark A, Bauer H C. Reconstruction in metastatic destruction of the acetabulum. Support rings and arthroplasty in 12 patients. Acta Orthop Scand 1996; 67: 435–8
- Vena V E, Hsu J, Rosier R N, O'Keefe R J. Pelvic reconstruction for severe periacetabular metastatic disease. Clin Orthop 1999, 362: 171–80
- Walker R H. Pelvic reconstruction/total hip arthroplasty for metastatic acetabular insufficiency. Clin Orthop 1993, 294: 170–5

