A 32-year-old man was treated for diaphyseal osteomyelitis of the tibia, proven by an open biopsy. A drilling of the whole tibia through a proximal approach and insertion of gentamycin chains was performed, with no effect on the pain. 8 weeks later, MRI showed pathological changes of the whole tibia and a small soft tissue extension in the mid-diaphyseal area which did not affect the vessels or the nerves. Again, an open biopsy was performed and Ewing sarcoma was diagnosed. After preoperative chemotherapy according to the EURO-Ewing protocol, the patient was referred to our department for knee disarticulation.
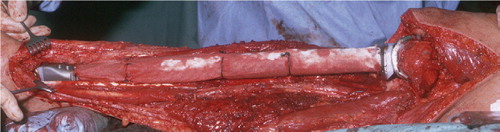
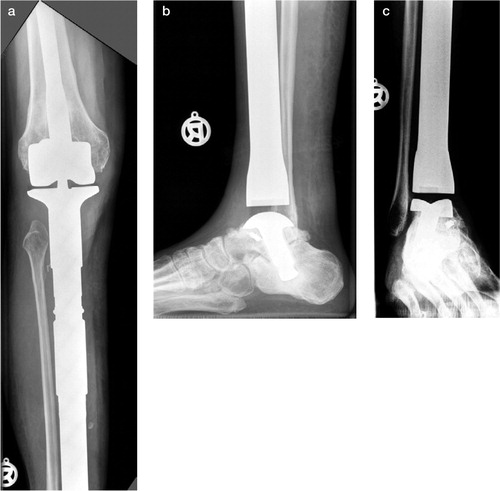
Being aware of the contamination of the whole tibia and the anterior proximal skin and soft tissue, we performed a total resection of the tibia including a skin resection of 6 × 5 cm in the proximal tibia area. The flexor digitorum longus muscle, the posterior tibialis muscle and part of the tibialis anterior muscle were left on the tibia to allow a wide margin. The neurovascular bundles, the superficial flexors, the hallucis longus flexor muscle, the extensors and peroneal muscles could be preserved. The bony defect was reconstructed with a modular endoprosthesis () of the MUTARS System (Implantcast, Buxtehude, Germany). The knee joint was reconstructed with a rotating-hinge modular system with a connection to a titanium bone replacement system (MUTARS). The ankle joint was reconstructed with an unconstrained component with a talar surface replacement stabilized with a trans-talar and trans-calcanear stem. An arthrodesis of the talo-calcanear joint was performed. The endoprosthesis was enveloped with a Trevira tube (Gosheger et al. Citation2001) for attachment of the patellar tendon and attachment of a medial and lateral gastrocnemius flaps, which were transferred to the anterior side of the endoprosthesis for soft tissue coverage (). The ventral capsule of the ankle joint was reconstructed with MITEK super anchors in combination with a Trevira Tube. A stable ankle joint could be achieved. A skin defect was covered with a skin-mesh graft on the gastrocnemius flap.
Figure 1. The modular endoprosthetic device, consisting of a rotating-hinge knee replacement and an unconstrained ankle joint replacement.

The pathological analysis of the specimen showed that the surgical margin was wide and showed spread of the tumor in the whole tibia. There was a poor response to chemotherapy.
The postoperative treatment consisted of 3 months of immobilization in an above-knee cast followed by stabilization with an orthosis, including the ankle, for 3 months more. In the distal part of the wound, a 4 × 3 × 2 cm tissue defect healed without surgery after 8 weeks. The leg was irradiated postoperatively because of the poor response to the chemotherapy.
3 months postoperatively, osteointegration of the components could be seen on radiographs. 6 months after the intervention, the patient was full-weight bearing and showed only a moderate limp. 9 months after the intervention, the patient was fully employed again as a plumber.
At the latest follow-up, 2 years after surgery, the patient had no pain. The skin grafts and muscle transfer of the medial and lateral gastrocnemius muscle led to a good soft tissue coverage (). The MSTS score (Enneking et al. Citation1993) was 25 of 30 possible points. Knee motion was 0–95° and ankle ext./flex was 5–25°. Radiographs showed a stable implantation of the stems without signs of loosening (). Arthrotic changes of the talonavicular or calcaneo-cuboidal joints could not be seen. There were no signs of local recurrence, and CT of the chest/abdomen and whole-body bone scan showed no signs of metastasis.
Discussion
The subcutaneous location and the proximity of the tibia to the neurovascular bundles and tendons make it difficult to achieve a wide excision of bone tumors with extraskeletal extension (Abudu et al. Citation1999). In cases of involvement of the neurovascular bundle, ankle joint or important tendons of the ankle and the foot, amputation is recommended.
Few tumors of the distal tibia have been reported to have been treated by resection and reconstruction. Ruggieri et al. (Citation1987) described 5 cases that were treated by resection and reconstruction by autologous bone grafting and tibiotarsal arthrodesis with fixation by a Kuntscher nail or a plate. Infection was the most frequent complication (2 cases). Casadei et al. (Citation1994) treated 12 cases of bone tumors in the distal tibia by resection and reconstruction with ankle arthrodesis. In 7 of the cases autologous bone was used, and in 5 cases this was combined with allografts. A major disadvantage of the procedures described was the long period of non-weight bearing (up to 1 year) to allow healing of the arthrodesis.
Limb salvage surgery with endoprosthetic replacement of the distal tibia and the ankle joint has been described, with good functional outcome (Abudu et al. Citation1999, Lee et al. Citation1999, Natarajan et al. Citation2000). Nevertheless, Abudu et al. (Citation1999) and Lee et al. (Citation1999) reported loosening of the resurfacing talar component, or of a talar collapse due to the talar component, in one-fifth of the patients.
For the first time, we have described a total endoprosthetic replacement of the complete tibia including a rotating-hinge knee prosthesis and a trans-talar and trans-calcanear stem. The trans-talar and trans-calcanear stem offer a high primary rotational stability which facilitates osteointegration. Early weight bearing was possible and the function was (and still is) good. Early loosening or talar collapse did not occur.
The author is grateful to Professor Karl Tillmann (Bad Bramsted) who, as an expert in ankle joint replacement, contributed to the design of the trans-talar/trans-calcanear stem.
No competing interests declared.
- Abudu A, Grimer R J, Tillman R M, Carter S R. Endoprosthetic replacement of the distal tibia and ankle joint for aggressive bone tumours. Int Orthop 1999; 23(5)291–4
- Casadei R, Ruggieri P, Giuseppe T, Biagini R, Mercuri M. Ankle resection arthrodesis in patients with bone tumors. Foot Ankle Int 1994; 15(5)242–9
- Enneking W F, Dunham W, Gebhardt M C, Malawar M, Pritchard D J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop 1993, 286: 241–6
- Gosheger G, Hillmann A, Lindner N, Rodl R, Hoffmann C, Burger H, Winkelmann W. Soft tissue reconstruction of megaprostheses using a trevira tube. Clin Orthop 2001, 393: 264–71
- Lee S H, Kim H S, Park Y B, Rhie T Y, Lee H K. Prosthetic reconstruction for tumours of the distal tibia and fibula. J Bone Joint Surg (Br) 1999; 81(5)803–7
- Natarajan M V, Annamalai K, Williams S, Selvaraj R, Rajagopal T S. Limb salvage in distal tibial osteosarcoma using a custom mega prosthesis. Int Orthop 2000; 24(5)282–4
- Ruggieri P, Capanna R, Biagini R, Casadei R, Campanacci M. Resection of the distal tibia in bone tumours. Ital J Orthop Traumatol 1987; 13(3)299–305