Abstract
Background Tension band wiring is the most common surgical procedure for fixation of fractures of the olecranon, but symptomatic hardware prominence and migration of K-wires can cause a high re-operation rate. The olecranon sled has been designed to minimize some of these problems.
Material and methods Simulated olecranon fractures were created in 6 matched pairs of cadaver arms. Each pair was fixed with tension band wiring used on the one arm and the olecranon sled being used on the other. Mechanical testing was done with the humerus rigidly fixed in a vertical position while the forearm was held at 1 of 3 angles of elbow fixation, 45°, 90° and 135°, respectively. For each angle, the triceps and the brachialis muscles were sequentially loaded with 5 kg (50 N) for 20 cycles and the amount of fracture displacement measured.
Results Loading of the brachialis muscle produced no increase in the fracture gap for either of the two fixation techniques. However, an increase in the fracture gap of up to 0.23 mm was found after cyclic loading of the triceps muscle for both techniques. The amount of increase was not significantly different between the two techniques.
Interpretation The olecranon sled appears to provide as stable fixation as tension band wiring for olecranon fractures.
Fractures of the olecranon are among the most common injuries of the upper extremity (Jupiter and Mehne Citation1992). Although there are a variety of devices and techniques to fix these fractures, the most common method is open reduction and internal fixation with tension band wiring, a principle first advocated in 1963 (Weber and Vasey) and further refined by the AO group (Müller and Allgöwer Citation1970). However, a number of complications related to the AO technique have been described, such as symptomatic hardware prominence, proximal migration of the K-wires, skin breakdown and infection, loss of extension in the elbow joint due to impingement of the K-wires, loosening or breakage of the tension band, fracture displacement with delayed union, and a high re-operation rate (Macko and Szabo Citation1985, Helm et al. Citation1987, Coleman and Warren Citation1990, Romero et al. Citation2000). Nonunion is rare in fixed olecranon fractures but nonunion rates after transolecranon osteotomy (in the treatment of distal humeral fractures) have been reported to be as high as 10%, regardless of the technique used (Henley Citation1987, Holdsworth and Mossad Citation1990, Petraco et al. Citation1996).
To avoid some of these complications, a new type of fixation device, the olecranon sled, has been designed (TriMed Inc., Valencia, CA). It consists of an outer wire loop (fixed to the ulna with a washer and two cortical screws) connected to two legs that are inserted into the fracture fragment and interdigitating intramedullary within the ulna ().
The objective of this cadaver study was to determine the stability of olecranon fracture fixation with the olecranon sled and to compare it with the standard method of tension band wiring. We used a cadaver arm model with physiological loading at standard anatomical angles, which has been used previously for evaluation of olecranon fixation (Petraco et al. Citation1996).
Material and methods
6 matched pairs of fresh-frozen arms without any clinical or radiographic evidence of injury were thawed to room temperature before use. 4 pairs were from men and 2 pairs from women (age range 40–67 years). A single, experienced surgeon (JD) performed all surgeries.
An incision of approximately 8 cm was made over the dorsal side of the elbow. The approach to the proximal ulna was performed in the standard manner for fractures in this region. A fracture of the olecranon was simulated at the midpoint of the semilunar notch between the coronoid and olecranon processes by sawing half of the outer bone and breaking the remaining part to the articular surface, by forcing an osteotome into the cut to achieve a more natural fracture pattern. The fracture was then reduced and held with a pointed reduction forceps. The paired elbows were then fixed with the following two methods varying left to right applications.
The olecranon sled group
2 parallel holes were drilled from the tip of the olecranon into the ulna medullary cavity with the help of a drill guide. The 2 free legs of the sled were then inserted into the ulna. The retaining washer was then placed with its slot over the prominence of the olecranon sled and a hole in dorsoventral direction was then drilled bicortically into the ulna, through the distal part of the proximal oval hole in the washer (). The screw, which had a length of 22–36 mm, was then tightened until adequate compression of the fracture site could be observed visually. Finally, a cortical screw was inserted in the distal washer hole to maintain fixation.
The tension band wiring group
The modified AO technique with oblique, bicortical K-wires was used. This method provides increased resistance to fracture displacement compared to the traditional technique with straight intramedullary positioning of the K-wires (Prayson et al. Citation1997). An 18-gauge, stainless steel monofilament cerclage wire was then passed through a previously drilled 1.6-mm hole in the ulna, about 3 cm distal to the fracture, and then passed around the K-wires to form a figure-of-eight. The two-knot modification of Weber and Vasey (Citation1963) was then used to tighten the wire.
Mechanical testing
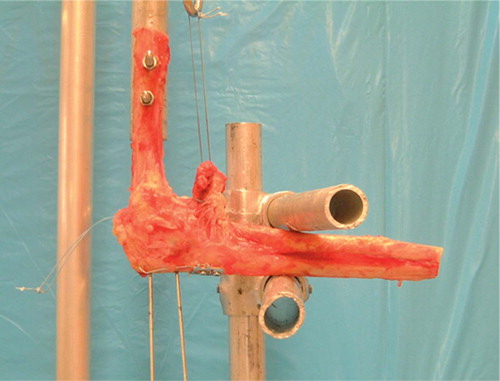
A test frame was constructed to hold the arm in controlled positions and apply simulated muscle forces (). Prior to testing, the majority of soft tissues were removed, preserving the triceps and the brachialis muscle attachments. The humerus was rigidly fixed to the frame in a vertical position, and the forearm was held at one of three angles of elbow flexion, 45°, 90° and 135°. For each angle, the triceps and the brachialis muscles were sequentially loaded with weights applied to cables sutured to the muscle attachments in a physiological direction. Each muscle was loaded with 5 kg (50 N) for 20 cycles. This load has been shown to simulate that of activities of daily living (Matsen Citation1980). To measure the amount of fracture displacement, 2 Steinman pins were drilled into either side of the fracture on the dorsal side of the olecranon and rigidly fixed with fast-setting epoxy. The distance between the ends of the pins was then measured before and after loading with calipers. The maximum gap at the fracture for each muscle load was calculated by trigonometry using the lengths of the pins, the length of the osteotomy and the displacement of the tips after loading (Tejwani et al. Citation2002-03). The estimated error in this calculation was 0.002 mm.
Statistics
A paired Student t-test was used to compare the stabilities achieved with the two devices at each test angle; p-values less than 0.05 were considered significant. A power analysis was also performed.
Results
The mean displacements at the fracture site after 20 cycles of loading were calculated (Table). There was no significant increase in the fracture gap for either technique, when cyclically loading the brachialis muscle at any of the three flexion angles (pvalues ranged from 0.3 to 0.5).
Mean displacement at fracture site after cyclic loading
Cyclic loading of the triceps muscle with the elbow at 90° flexion resulted in an average fracture gap of 0.23 mm with the olecranon sled and 0.20 mm with the tension band wiring, which was not a statistically significant difference (p = 0.3, with a power to detect a difference of 0.09 mm of 80%). Similar results were obtained for the other flexion angles. For example, for a 135° flexion angle, the fracture gap increased by an average of 0.21 mm in the olecranon sled group and by 0.19 mm in the tension band wiring group (with 80% power to detect a difference of 0.20 mm). The lower displacements at 45° are due to increased compression of the proximal fragment against the humerus due to the changed angle of the applied muscle force.
The size of fracture gaps was the same after 1 cycle and after 20 cycles, indicating that the fracture displacement was not progressive within this cycling period.
Discussion
We found no difference between the fixation stability achieved with the two operative techniques. This is probably due to similarities between the olecranon sled and the tension band wiring. Both methods act to pull together the outer aspect of the fracture (which is normally under tension) by twisting the wire in the tension band wiring or by dynamic compression with the washer and screw in the olecranon sled. Both constructs wrap around the proximal end of the ulna, providing additional support to this fragment. Both techniques use intramedullary interdigitation to prevent lateral migration or twisting of the fracture fragments relative to each other.
The difference between the two devices is that, in contrast to the intramedullary pins of the olecranon sled, the K-wires of the tension band are not physically connected to the cerclage wire, allowing relative motion between these parts which can compromise the fixation. This may result in abrasion, breakage or untwisting of the wire, or migration of the pins. The clinical consequences can be pain with soft tissue irritation, erosion through the skin, infection, fracture displacement, and nonunion that can require secondary surgical procedures. However, a 76–95% good or excellent outcome of tension band wiring has been reported (Macko and Szabo Citation1985, Karlsson et al. Citation2002). Still, one of the main problems of using tension band wiring is a rate of up to 80% of symptomatic hardware prominence (Murphy et al. Citation1987, Romero et al. Citation2000, Karlsson et al. Citation2002), mostly resulting from local pressure or migration of the K-wires, and which requires a second operation to remove the hardware. To solve this problem, Larsen and Jensen (Citation1991) tried modified Netz pins (Netz and Strömberg Citation1982) instead of K-wires in combination with tension banding and reported no case of backing-out, but finally had to remove the hardware in 70% of the patients. To avoid hardware problems with tension band wiring, some authors have recommended plating techniques (King et al. Citation1996, Tejwani et al. Citation2002-2003). Other authors have considered a plate to be too large an implant to be used, or only marginally better as a routine method of fixation for this kind of fracture (Fyfe et al. Citation1985, Morrey Citation1995, Romero et al. Citation2000). The AO principle of converting posterior tensile forces to articular compressive forces has been questioned in a mechanical test of 4 fixation techniques, which consisted of intramedullary and cortically fixed tension constructs, cancellous screw with and without a tension band (Hutchinson et al. Citation2002). None of the constructs resulted in compression across the fracture gap. A screw in conjunction with a tension band proved better fixation stability than the three other methods. In another mechanical study comparing 5 techniques of internal fixation of fractures of the olecranon, the tension band wiring with 2 tightening knots allowed minimal movement even at high loads (Fyfe et al. Citation1985). Intramedullary cancellous screw fixation gave erratic results, even with the addition of a tension band.
The olecranon sled overcomes some of the limitations of the tension band wiring by combining the intramedullary pins (legs of the sled) and the superficial wire of the sled into a single implant. The technique of insertion is simplified, and the need to remove pins because of protrusion into the soft tissues is eliminated. The problem of abrasion and movement of the point of fixation is solved by rigid fixation of the sled to the bone with screws and washer. Soft tissues may tolerate the low profile of the olecranon sled better than other designs.
Mechanical results can sometimes be difficult to apply to the clinical situation. In a previous, similar study (Petraco et al. Citation1996) the authors compared fixation stability of three different operative methods for olecranon osteotomy. They found that for all fixation techniques, total displacement caused by the brachialis load was appreciably greater than that of the triceps load. We found the opposite. This is due to the location and nature of the osteotomy. In our case, its more proximal location led to support of the ulna when loaded by the brachialis. This limits the conclusions of this study to specific fracture patterns. Another limitation was that the cyclic loading was of limited duration. It is possible that longer cycling could show other differences between the 2 techniques.
In summary, this study has shown no significant difference in the fixation stability between the tension band wiring and the olecranon sled in two-part fractures. The olecranon sled may be a good compromise between two fixation techniques, tension band wiring and plate fixation. It has the advantage of a simple fixation method, as the tension band wiring, but without the associated hardware problems. It also has the advantage of a lower profile than plating. This suggests that the olecranon sled method could be an appropriate surgical technique for fixation of olecranon fractures. The above-men-tioned advantages of the olecranon sled can only be tested and verified in clinical studies.
This study was supported by the Stig and Ragna Gorthon Foundation, Helsingborg, Sweden and by TriMed Inc., Valencia, CA. Trimed did not participate in the design of the study, in the evaluation of results or in the writing of the article.
Contributions of authors
JD performed the mechanical tests under supervision of FJK after an idea of LC. All participated in the writing of the manuscript.
- Coleman N P, Warren P J. Tension-band fixation of olecranon fractures. A cadaver study of elbow extension. Acta Orthop Scand 1990; 61(6)58–9
- Fyfe I S, Mossad M M, Holdsworth B J. Methods of fixation of olecranon fractures. An experimental mechanichal study. J Bone Joint Surg (Br) 1985; 67: 367–72
- Helm R H, Hornby R, Miller S W M. The complications of surgical treatment of displaced fractures of the olecranon. Injury 1987; 18: 48–50
- Henley M B. Intra-articular distal humeral fractures in adults. Orthop Clin North Am 1987; 18: 11–23
- Holdsworth B J, Mossad M M. Fractures of the adult distal humerus. Elbow function after internal fixation. J Bone Joint Surg (Br) 1990; 72(3)362–5
- Hutchinson D T, Horwitz D S, Ha G, Thomas C W, Bachus K N. Cyclic loading of olecranon fracture fixation constructs. J Bone Joint Surg (Am) 2002; 85(5)831–7
- Jupiter J B, Mehne D K. Trauma to the adult elbow of the distal humerus. Skeletal trauma. Fractures, dislocations, ligamentous injuries, B D Browner, J B Jupiter, A M Levine, P G Trafton. WB Saunders, Philadelphia 1992; 1: 1125–76
- Karlsson M K, Hasserius R, Besjakov J, Karlsson C, Josefsson P O. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg 2002; 11: 377–82
- King G J W, Lammens P N, Milne A D, Roth J H, Johnson J. A Plate fixation of comminuted olecranon fractures: An in vitro biomechanichal study. J Shoulder Elbow Surg 1996; 5: 437–41
- Larsen E, Jensen C M. Tension-band wiring of olecranon fractures with nonsliding pins. Report of 20 cases. Acta Orthop Scand 1991; 62: 360–2
- Macko D, Szabo R M. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg (Am) 1985; 67(9)1396–401
- Matsen F A. Biomechanics of the elbow. Basic biomechanics of the skeletal system, V H Frankel, M Nordin. Lea & Febiger, Philadelphia 1980; 243–53
- Morrey B F. Current concepts in the treatment of fractures of radial head, the olecranon, and the coronoid. J Bone Joint Surg (Am) 1995; 77: 316–27
- Müller M E, Allgöwer M. Manual of internal fixation. Techniques recommended by the AO-group. Springer, 1970, New York
- Murphy D F, Greene W B, Dameron T B, Jr. Displaced olecranon fractures in adults. Clinical evaluation. Clin Orthop 1987, 224: 215–23
- Netz P, Strömberg L. Non-sliding pins in traction absorbing wiring of fractures: a modified technique. Acta Orthop Scand 1982; 53: 2355–60
- Petraco D M, Koval K J, Kummer F J, Zuckerman J D. Fixation stability of olecranon osteotomies. Clin Orthop 1996, 333: 181–5
- Prayson M J, Williams J L, Marshall M P, Scilaris T A, Lingenfelter E J. Biomechanical comparison of fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma 1997; 11(8)565–72
- Romero J M, Miran A, Jensen C H. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci 2000; 5: 318–20
- Tejwani N C, Garnham I R, Wolinsky P R, Kummer F J, Koval F J. Posterior olecranon plating: biomechanical and clinical evaluation of a new operative technique. Bull Hosp Jt Dis 2002-03; 61(1–2)27–31
- Weber B G, Vasey H. Osteosynthese bei Olekranonfraktur. Z Unfallmed Berufskr 1963; 56: 90–6