Abstract
Introduction In the early 1960s, Charnley was cautious with his patient selection for total hip replacement. As follow-up increased and confidence in the operation grew, younger patients were selected. We present our results of the Charnley LFA in young patients with rheumatoid and juvenile rheumatoid arthritis with a followup of up to 36 years.
Patients We studied 292 Charnley low-friction arthroplasties in 195 young patients with an established diagnosis of rheumatoid arthritis. Their mean age at operation was 38 (12–50) years; 168 (58%) were receiving steroids and 79 (27%) were on non-steroidal antiinflammatory medication. The mean follow-up for the whole group was 15 (1–36) years. 24 patients could not be traced (33 hips), and 61 patients died (88 hips).
Results 25 patients (41 hips) had had a revision. The main indication for revision was cup loosening. In the 85 patients (130 hips) attending follow-up, their mean age at surgery was 36 (17–50) years and the mean follow-up was 20 (10–36) years. 98% were pain-free or had no more than occasional discomfort, 44% claimed to have normal or near-normal function, while 62% had full or almost full range of movement of the replaced hip. Radiographically, 29 cups (22%) were considered to be loose. 1 stem (1%) was definitely loose and 2 stems (2%) were probably loose. With revision for any indication as the endpoint, the survival was 74% at 25 years follow-up.
Interpretation The Charnley LFA continues to be an excellent hip replacement, even for very young rheumatoid arthritis patients. Wear and aseptic cup loosening are the main long-term problems.
When Charnley introduced the low-frictional torque arthroplasty (LFA) into clinical practice in November 1962, he was well aware of the possible long-term problems: wear of the ultra-high molecular weight polyethylene (UHMWPE) cup and loosening of the components (Charnley Citation1967). He remained cautious, both in selecting the patients for the operation and in delaying the release of the components for general use; the components were not released until the second half of 1970. (Charnley informed the past Residents by letter (Charnley Citation1970)). With time, as confidence in the method grew, indications for the operation were broadened and the results of increasing follow-up were published (Charnley Citation1972, Wroblewski Citation1992, Wroblewski et al. Citation2002). We present our results of the Charnley LFA in young patients with rheumatoid and juvenile rheumatoid arthritis (Rh/JRA) with a follow-up of up to 36 years.
Patients and methods
Our database covers a 42-year period from November 1962, and is updated regularly. For the purpose of this review, we have taken the 28-year period from November 1962 to December 1990 and have extracted the details of patients with the diagnosis of Rh/JRA who were under the age of 51 years at the time of the LFA. All patients had been under the care of a specialist rheumatology consultant.
195 patients, 158 women and 37 men, had undergone 292 LFAs. Mean age at operation was 38 (12–50) years and mean weight was 57 (30–93) kg. 97 patients (50%) had had bilateral LFAs; in 17 this had been carried out under the same general anesthetic, while 80 had had both hips replaced by December 1990. 168 patients (58%) were receiving steroid medication and 79 (27%) were on nonsteroidal anti-inflammatory drugs. 19 patients (20 hips) had had previous hip operations: 9 intertrochanteric osteotomies, 4 cup arthroplasties, and 1 open reduction with a diagnosis of juvenile rheumatoid arthritis and a developmental hip dysplasia. 6 other patients had had various other soft tissue procedures.
All operations had been carried out in the Charn-ley-Howorth clean air enclosure using total body exhaust suits. The transtrochanteric approach was used routinely. Assessment of the clinical results was according to Merle d’Aubigne and Postel (Citation1954), as modified by Charnley (Citation1972).
At the latest review (August 2005), the mean follow-up for the whole group was 15 (1–36) years. 24 patients (11%; 33 hips) could not be traced; their mean follow-up was 7 (2–23) years. 61 patients (30%; 88 hips) are known to have died; their mean follow-up was 9 (1–27) years. 25 patients (14%; 41 hips) had had a revision; their mean follow-up was 14 (3–28) years. 85 patients (45%; 130 hips) were still attending; their mean follow-up was 20 (10–36) years.
Radiographic assessment of the bone-cement interface of the cup was made on the anteroposterior radiographs (Hodgkinson et al. 1988). Loosening was defined as complete demarcation of bone-cement interface greater than 1 mm. Migration of the cup was deemed to be present if there was a change of position, as observed on serial radiographs in relation to fixed anatomical landmarks: the teardrop, the medial acetabular wall, or the angle between the inter-teardrop line and the face of the cup.
On the femoral side, the classification of Harris et al. (Citation1982) was used: the appearances on the anteroposterior radiographs, classified as indicating definite, probable, or possible stem loosening.
Wear measurements of the UHMWPE cup was made on the radiographs (Griffith et al. Citation1978). In the survivorship analysis (Kaplan and Meier Citation1958, Lettin et al. Citation1991), we took revision for any indication as endpoint (Wroblewski et al. Citation2002). Since the need for a regular and indefinite follow-up was mutually agreed upon before the LFA, we were anxious to trace all non-attendees. This was carried out at three levels—contacting patients (accepting relatives’ responses), family practitioners, and finally, if necessary, the Office of National Statistics (Southport, UK).
Results
Complications
Complications within 1 year of the LFA are shown in , late complications in , and indications for revision in . 9 hips had nonunion of the trochanter and 7 patients had a non-fatal pulmonary embolism. Not all radiographically loose cups and stems were revised. Of the 68 radiographically loose cups, only 27 had been revised for progressive loosening at the time of review. 9 of the 11 radiographically loose stems were revised; 2 were asymptomatic. All patients with radiographic changes were seen earlier in the outpatient followup clinic than those patients whose components were stable, to check radiographically whether loosening had progressed. 5 hips were revised for dislocation, 4 for infection, and 5 for a fracture of the stem. 1 hip was revised for unexplained pain. 1 fractured stem was not revised because it remained asymptomatic and there was no progressive change on the radiograph.
Table 1. Early complications (in the first postoperative year)
Table 2. Late complications (228 hips)
aSome patients had more than one complication. Included: indications for revision and radiographic appearances indicating complications. Excluded: patients (hips) lost to follow-up (n = 33) and deaths (n = 88).
Table 3. Revisions
Wear
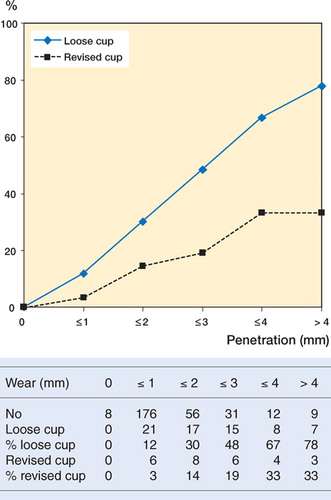
Wear of the UHMWPE cup, measured as penetration, was mean 0.08 (0.01–0.44) mm/year for the whole group and mean 0.06 (0.01–0.33) mm/year for the 85 patients attending (130 hips). Wear of the UHMWPE cup and cup migration and loosening are related; the incidence of cup migration increases with the depth of penetration of the cup (Wroblewski Citation1992). The correlation for all 292 hips is shown in .
Clinical results
At the latest follow-up or at the last follow-up before death, or on admission for a revision, 85% of patients had a pain-free hip and 8% had no more than occasional discomfort; 42% claimed to have normal or near-normal function, but only 10 patients had a strictly “single hip problem” of Charnley category A (Charnley Citation1972). The majority, 84%, were in category C and 13% were in category B. 65% had a full or almost full range of hip movement.
Of the 85 patients (130 LFAs) attending who had not had a revision, 90% had a pain-free hip and 8% had no more than occasional hip discomfort. Although 45% claimed to have normal function and 18% near-normal function, there were no patients with a strictly unilateral hip problem or no other function-restraining activities (Charnley category A): 13% were in Charnley category B and 87% were in Charnley category C. 62% had full or almost full range of movement of the hip.
Survivorship analysis
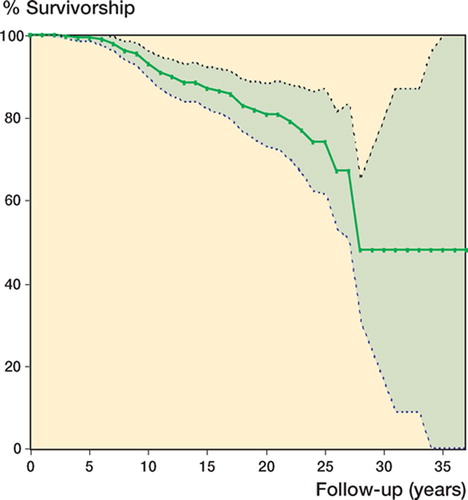
With revision for any indication as the endpoint, the survivorship was 93% (96–90) at 10 years, 87% (92–82) at 15 years, 81% (88–73) at 20 years and 74% (87–61) at 25 years, at which time 33 hips remained at risk ().
Discussion
The clinical results of the Charnley LFA are still successful—even in very young rheumatoid patients. Freedom from pain, the main indication for which the operation was designed and introduced into clinical practice, remain the central feature: 90% of patients were pain-free and 8% had no more than occasional discomfort.
Activity level, although claimed by some patients to be normal or near-normal, could not be assessed objectively as all patients had other pathologies affecting activity. Activity level after total hip arthroplasty is not a feature of a particular design, nor of the method of component fixation, provided it is secure under load; it is a reflection of the clinical skill of selecting patients with unilateral hip pathology. Patients with rheumatoid arthritis never feature as anecdotal, single-case successes.
The deep infection rate in our series (2%) was no higher than in an unselected group of patients (Wroblewski et al. Citation2002), considering that 58% of patients were receiving steroids. This is in contrast to a higher incidence of 7% reported by Schulte et al. (Citation1993), but more in line with the reports by Berry et al. (Citation2002), Lehtimaki et al. (Citation1999), Sochart et al. (Citation1997), and Lehtimaki et al. (Citation1997).
Wear of the UHMWPE cup and cup migration are related; the incidence of cup migration increases with the depth of cup penetration.
The revision rate for aseptic cup loosening found here (9%) is consistent with the series of Sochart et al. (Citation1997) and Onsten et al. (Citation1994). Although the mean rate of cup wear was lower, 0.06 (0.01–0.33) mm/year in the attending group as opposed to 0.08 (0.01–0.44) mm/year in the whole group, the large range (a factor of 44) makes any comparison difficult. Revisions for loose stem were too few to correlate to cup wear and whether wear contributed to the loosening. The mortality rate of 33% at a mean follow-up of 14 years is similar to figure of 43% at 19 years reported by Sochart et al. (Citation1997).
The Charnley LFA continues to be an excellent hip replacement even for very young rheumatoid arthritis patients. Wear and aseptic cup loosening are the main long-term problems. A combination of alumina ceramic and cross-linked polyethylene appears very promising, with the follow-up approaching 20 years (Wroblewski et al. Citation2005).
Our sincere thanks to the Office of National Statistics, Southport, UK for their help in tracing patients. This research was supported by the Peter Kershaw and John Charnley Trusts.
Contributions of authors
BMW: operated on the patients, analyzed the data and wrote the paper. PDS: organized the project, reviewed and analyzed the radiographs and clinical data and completed the statistical analysis. PAF: organized, input, validated and reviewed the clinical data and typed the manuscript.
- Berry D J, Harmsen W S, Cabanela M E, Morrey B F. Twenty five year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg (Am) 2002; 84: 171–7
- Charnley J. Total prosthetic replacement of the hip. Physiotherapy. 1967; 53: 407–9
- Charnley J. Personal communication. 1970
- Charnley J. The long term results of low-friction arthroplasty of the hip as a primary intervention. J Bone Joint Surg (Br) 1972; 54: 61–76
- Griffith M J, Seidenstein M K, Williams D, Charnley J. Socket wear in the Charnley low-friction arthroplasty of the hip. Clin Orthop 1978, 137: 37–47
- Harris W H, McCarthy J C, Jr, O'Neill D A. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg (Am) 1982; 64: 1063–7
- Hodgkinson J P, Shelley P, Wroblewski B M. The correlation between roentgenographic appearance and the operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop 1988, 228: 105–9
- Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–81
- Lehtimaki M Y, Lehto M U. K, Kautainen H, Savolainen H A, Hamalainen M M. J. Survivorship of the Charnley total hip arthroplasty in juvenile chronic arthritis. A follow-up of 186 cases for 22 years. J Bone. Joint Surg (Br) 1997; 79: 792–5
- Lehtimaki M Y, Kautainen H, Lehto M U. K, Hamalainen M M. J. Charnley low friction arthroplasty in rheumatoid arthritis. J Arthroplasty 1999; 14: 657–61
- Lettin A W. F, Ware H S, Morris R W. Survivorship analysis as assessment with reference to the Stanmore total knee replacement. J Bone Joint Surg (Br) 1991; 73: 729–31
- Merle d’Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg (Am) 1954; 36: 451–75
- Onsten I, Besjakov J, Carlsson A S. Improved radiographic survival of the Charnley prosthesis in rheumatoid arthritis and osteoarthritis. J Arthroplasty 1994; 9: 3–8
- Schulte K R, Callaghan J J, Kelley S S, Johnston R C. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty year follow-up. The results of one surgeon. J Bone Joint Surg (Am) 1993; 75: 961–75
- Sochart D H, Porter M L. P. The long term results of Charnley low friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthritis, or Rheumatoid arthritis. J Bone Joint Surg (Am) 1997; 79: 1599–1617
- Wroblewski B M. Charnley low friction arthroplasty in the young patient. Clin Orthop 1992; 285: 45–7
- Wroblewski B M, Siney P D, Fleming P A. Charnley low frictional torque arthroplasty in patients under the age of 51 years. Follow-up to 33 years. J Bone Joint Surg (Br) 2002; 84: 540–3
- Wroblewski B M, Siney P D, Fleming P A. Wear of the cup in Charnley LFA in the young patient. J Bone Joint Surg (Br) 2004; 86: 498–503
- Wroblewski B M, Siney P D, Fleming P A. Low friction arthroplasty of the hip using alumina ceramic and crosslinked polyethylene. A 17 year follow-up report. J Bone Joint Surg (Br) 2005; 87: 1220–1