Abstract
Background A high reoperation rate has been the main reason why Gamma nailing should not be recommended for routine use in the treatment of trochanteric fractures. We compared the outcome after reoperation to the outcome after primary surgery with Gamma nailing.
Methods In a series of 554 patients, we compared the outcome in 52 patients who were reoperated with that in 502 patients who had no reoperations. We assessed mortality, pain, walking ability and habitat at follow-up.
Results The most common reason for reoperation was new fracture around the implant (17), local pain after healed fracture (11), nonunion (9) and cut-out (8). A second reoperation was required in 9/52 patients. The mortality was significantly lower in the reoperated cases at 30 days and at 1–5 years, but not at 120 days, and there were no significant differences in the other outcome parameters.
Interpretation Reoperation did not lead to a worse clinical outcome, nor to increased mortality.
The Gamma nail has been widely used for the treatment of trochanteric fractures. However, a complication rate of 3–12%, including perioperative fractures around the implant, have led to the recommendation that the Gamma nail should not be used routinely (Parker and Pryor Citation1996, Parker and Handoll Citation2005). However, little is known about the outcome after revision surgery for complications of the Gamma nail. We assessed the outcome in patients who had revision surgery because of complications after Gamma nailing for a trochanteric fracture. The outcome was compared to that in patients who did not have any complications.
Patients and methods
We studied 52 patients who had a reoperation after having been treated with a Gamma nail for a trochanteric fracture (reoperated cases). The outcome in these patients was compared to that in 502 fracture cases who were also treated with Gamma nailing but were not reoperated, and who did not have secondary surgery during the study period.
The 554 patients were treated at our hospital between September 1, 1998 and August 31, 2003. During this 5-year period, all hip fracture patients were included in a prospective observational study in which we recorded data pertaining to living conditions, walking ability, and general health as measured by ASA scores (American Society of Anesthesiologists) (Michel et al. Citation2002), as well as information about the surgery. We recorded all reoperations until August 31, 2004 and all deaths until December 31, 2004. Thus, data for survival studies were censored on December 31, 2004.
A proportion of patients did not attend followup appointments, mostly due to poor health conditions. We were able to examine 38 of 52 reoperated cases after a mean of 1 (0.3–3) year and 347 of 502 cases who were not reoperated after 0.9 (0.1– 4.1) years. All hospital records, including those of neighboring hospitals, were inspected in order to ensure that no reoperation had been missed by the investigators, even though the patient did not attend follow-up.
The fractures were classified as stable or unstable according to the classification of Evans, as modified by Jensen (Jensen and Michaelsen Citation1975). Fractures with two fragments were considered stable, whereas fractures with more than two fragments or a reverse oblique fracture line were considered unstable. Stable fractures were mostly treated with a short nail with no distal locking screw, whereas unstable fractures were treated with a short nail with distal locking screw ().
Osteosynthesis was performed on a fracture table in standard fashion. The diaphysis was overreamed by 2 mm before the insertion of an 11-mm/135-degree nail. All nails were inserted by force of hand only; the use of a hammer was prohibited. All patients had oral antibiotics and also prophylaxis against thromboembolism with a low molecular weight heparin.
The characteristics of patients who were reoperated or not reoperated are shown in .
Table 1. Background information at index operation showing age at surgery and proportion of patients in each category
Statistics
For comparing rates and proportions, the chisquared test was used. The t-test of independent samples was used for comparing means. A p-value of less the 0.05 was considered significant. For comparison of proportions in the two groups, the 95% confidence interval for proportions is given. When determining the confidence intervals, the standard error (SE) of a proportion was calculated using the formula √p(1-p)/n where p is the proportion and n is the number of persons at risk. The 95% confidence interval was then calculated by adding and subtracting 1.96 × SE (Altman Citation1991).
Data were entered into a Cox regression model using SPSS v.12 software. In this analysis, we entered presumed risk factors in order to evaluate the importance of revision as a possible predictor of increased mortality.
Results
The revision rate in the entire material was 52/554 (9.4%) (). The fracture was classified as stable in 18/52 (0.3) of reoperated cases and in 254/502 (0.5) in the cases that were not reoperated (p = 0.03; chi-square) (). The most common reason for reoperation in the 52 reoperated cases was a postoperative fracture around the implant (17), local pain after healed fracture (11), nonunion (9) and cut-out (8) (). Of the 52 reoperated cases, 9 had a second reoperation (17%). As compared to the revision rate in the entire material, this result is not significant (p = 0.07; chi-squared test).
Table 2. Type of surgery and indication for primary surgery in cases that were not reoperated (n = 502) and in reoperated cases (n = 52)
Table 3. Reason for reoperation in reoperated cases and type of surgery including revisions
Comparing the cases who were reoperated and those who were not, there was no difference in the proportion of patients living in their own home after surgery, or in the proportion of patients who had retained their ability to be independent outdoor walkers. The proportion of patients experiencing no or slight hip pain was equal in the two groups ().
Table 4. Number and proportion of patients who resided in their own home and were independent walkers at surgery and at the follow-up examination. Presented as proportions with 95% confidence interval of proportions
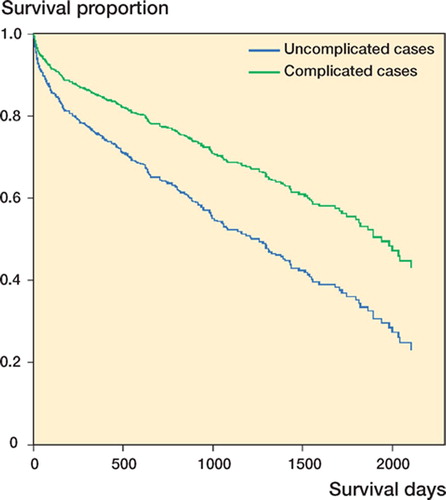
Mortality at 30 days and at 1–5 years was significantly lower in the reoperated patients than in the patients who were not reoperated, but not the mortality measured at 4 months ( and ; Figure). Cox regression analysis revealed that revision after primary surgery and female sex reduces the risk of mortality, whereas increasing age, ASA group 3–4, and living away from one's own home increased the risk of dying in this model.
Table 5. Estimated change in risk of mortality. Risk below 1 indicates less risk. All risks are significant, as confidence interval does not encompass 1
Table 6. Mortality in the cases that were reoperated and Survival proportion not reoperated, and p-values for the difference between 1.0 the groups as determined by chi-square test
Discussion
Several authors have reported a lower rate of complications using a screw-plate system, which is currently considered to be the gold standard, compared to a Gamma nail (Parker and Pryor Citation1996, Osnes et al. Citation2001, Parker and Handoll Citation2005). Also, a higher The revision rate was 52/554 (9%) which is rate of fracture around the implant has been cited somewhat higher than in previously published as the main reason why the Gamma nail should not reports (Parker and Pryor Citation1996, Adams et al. Citation2001, be used for routine treatment of trochanteric frac-Miedel et al. Citation2005). The reason for this is at least in tures. However, the goal of the treatment is to assist part due to the fact that we have chosen to include the patient in regaining the best possible function patients who had removal of hardware (11/554) and well-being, while keeping cost and suffering after the fracture had healed. Although removal of at the lowest possible level. It is therefore impor-hardware is undoubtedly a reoperation, it might not tant to know how reoperations affect the ultimate be considered a complication. The threshold of recoutcome in patients. In this study, we attempted to ommending hardware removal may vary between determine whether revision of the primary Gamma surgeons, as well as between institutions. Even so, nailing is detrimental to the final outcome. using an implant that requires a high rate of removal after fracture healing would not be beneficial to the patient—nor to the health care system—unless the implant has advantages that outweigh this. In our study, 2 of the 11 patients in the group of patients who had elective hardware removal had a second reoperation, both with hemiarthroplasty. One sustained a new fracture after a fall and the other patient was diagnosed with a nonunion 2 weeks after hardware removal. This patient might have been more correctly classified among the nonunions. This rate of complication after hardware removal is similar to what was found in a previous report (Hesse and Gächter Citation2004), in which 4 of 30 patients who had their nail removed sustained a new proximal femoral fracture.
Survival of cases that were reoperated and not reoperated, adjusted for age, sex, ASA class and habitat.
Clinical outcome after surgery, as assessed by calculating the proportion of patients who lived in their own home both at the time of surgery and at follow-up, did not reveal any differences between the patients who were reoperated and those who were not. Likewise, there was no difference in the proportion of patients who retained their ability to be independent outdoor walkers after surgery; nor was there any difference in the pain score. These results must be interpreted with caution, as the proportion of patients returning for follow-up was only 70%. However, the results lend some support to the notion that a higher rate of reoperations among the reoperated cases did not result in a worse outcome. This is in accordance with findings in reports investigating the impact of revision surgery after osteosynthesis for intracapsular hip fracture, in which the authors did not find any increase in morbidity or mortality after revision surgery (Palmer et al. Citation2000).
Mortality expressed as the proportion of patients who died within 30 days, 4 months, or 1–5 years, was lower in the reoperated cases—which does not imply a worse outcome after reoperation, a finding which is also supported by previous studies (Sipila et al. Citation2004). In the Cox regression model, it appears that revision surgery reduced the risk of mortality even after correction for sex, age, habitat, and ASA group. In any case, it seems that revision surgery does not represent a major setback to the health of the patients.
Even though the rate of complications is important in evaluating an implant, the outcome after revision surgery should also be taken into account.
Any complication or reoperation is an undesirable event, both in terms of individual suffering and in the cost to society. It appears, however, that correctional surgery after complications with the use of the Gamma nail does not significantly worsen outcome.
Contributions of authors
KB: designed the study, collected and analyzeded the data and wrote the manuscript in collaboration with OR. OR: assisted in analyzing and preparing data for publication and revised the manuscript.
- Adams C I, Robinson C M, Court-Brown C, McQueen M. M. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma 2001; 15: 394–400
- Altman D. Practical statistics for medical research. 1991
- Hesse B, Gächter A. Complications following the treatment of trochanteric fractures with the Gamma nail. Arch Orthop Trauma Surg 2004; 124: 692–8
- Jensen J S, Michaelsen M. Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand 1975; 46: 795–803
- Michel J P, Klopfenstein C, Hoffmeyer P, Stern R, Grab B. Hip fracture surgery: is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome?. Aging Clin Exp Res 2002; 14: 389–94
- Miedel R, Ponzer S, Tornkvist H, Soderqvist A, Tidermark J. The standard Gamma nail or the Medoff sliding plate for unstable trochanteric and subtrochanteric fractures. A randomised, controlled trial. J Bone Joint Surg (Br) 2005; 87: 68–75
- Osnes E K, Lofthus C M, Falch J A, Meyer H E, Stensvold I, Kristiansen I S, Nordsletten L. More postoperative femoral fractures with the Gamma nail than the sliding screw plate in the treatment of trochanteric fractures. Acta Orthop Scand 2001; 72: 252–6
- Palmer S J, Parker M J, Hollingworth W. The cost and implications of reoperation after surgery for fracture of the hip. J Bone Joint Surg (Br) 2000; 82: 864–6
- Parker M J, Handoll H H. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Revi 2005
- Parker M J, Pryor G A. Gamma versus DHS nailing for extracapsular femoral fractures. Meta-analysis of ten randomised trials. Int Orthop 1996; 20: 163–8
- Sipila J, Hyvonen P, Partanen J, Ristiniemi J, Jalovaara P. Early revision after hemiarthroplasty and osteosynthesis of cervical hip fracture: short-term function mortality unchanged in 102 patients. Acta Orthop Scand 2004; 75: 402–7
