Abstract
Background The Kudo total elbow prosthesis (TEP) is a well-established implant with good mid-term results. The ulnar component can be placed with or without cement, and the humeral component is normally placed without cement.
Methods 89 Kudo type-5 total elbow prostheses were evaluated after a mean follow-up of 6 (1.7–11) years. The indication for joint replacement was rheumatoid arthritis in all cases. 49 prostheses were placed without cement. In 40 cases, the ulnar component was cemented and the humeral component was uncemented.
Results In the uncemented group, 7 revisions had taken place. 3 of these ulnar components were shortstemmed and 4 were long-stemmed. No revisions had been performed in the hybrid group. In the uncemented group another 7 patients showed progressive radiolucencies, while 3 patients in the hybrid group showed progressive radiolucencies.
Interpretation In this group of RA patients, the survivorship of the cemented ulnar component was better than that of the uncemented ulnar component.
The Kudo total elbow prosthesis (TEP) is a wellestablished implant with good mid-term results. This implant is used for patients with rheumatoid arthritis (RA) (Kudo et al. Citation1980, Fink et al. Citation2002, An Citation2005), hemophilic arthropathy (Chap-man-Sheath et al. 2003), and posttraumatic arthritis (An Citation2005). In the last decades, this implant has undergone several modifications; from the unstemmed type-1 implant to the fully cemented, stemmed type-3. The type-4 implant was the first that could be placed uncemented, but it had a poor outcome due to breakage of the humeral stem. The last type (type 5) has overcome the problems of stem breakage of the humeral component. The ulnar component can be placed with or without cement, and the humeral component is normally placed without cement. We report the mid-term results of the Kudo type-5 TEP and compare the results of the uncemented ulnar components to those of the cemented ulnar components. In this series only uncemented humeral implants were used. Most studies combine different types of Kudo TEP for different indications. In this series only type-5 Kudo TEPs have been included, with joint destruction due to rheumatoid arthritis being the only indication.
Patients and methods
Between 1994 and 2004, 89 Kudo type-5 prostheses (Biomet Inc., Warsaw, IN) were implanted because of joint destruction due to RA. The mean age of the patients (67 of whom were women) was 55 (21–84) years. 49 TEPs were fully uncemented and 40 were hybrid (humeral component uncemented and ulnar component cemented). Evaluation took place after an average of 5.8 (1.7–11) years of follow-up and consisted of a questionnaire, elbow function assessment (EFA), and AP and lateral radiographs in a standard way (de Boer et al. 1999). After implantation of the prosthesis, a radiograph was taken every 2 years—or sooner if the patient had any complaints.
The EFA-score (de Boer et al. 1999) is a clinical score with a maximum of 100 points; the different items are shown in .
Table 1. Elbow Function Assessment, with different items and subcategories
Statistics
The results were compared using SPSS software version 11.5. Pre-and postoperative range of motion was analyzed with the paired t-test. Pain score and EFA postoperatively were analyzed using the independent-sample t-test. A p-value
< 0.05 was considered significant. The survival of the prosthesis was calculated from the time of implant to the time of revision, or to the occurrence of radiolucencies in the radiographs.
Operative technique
All procedures were performed in a similar way by the senior orthopedic surgeons at two institutions. The elbow joint was exposed through a straight posterior incision and a u-shaped triceps flap was created. The ulnar nerve was identified and mobilized. The nerve was identified proximally and exposed by dividing the roof of the cubital tunnel between the two heads of the flexor carpi ulnaris. It was then retracted and protected during the remainder of the procedure. A transverse incision was made through the triceps aponeurosis, beginning at the intermuscular aponeurosis at a point 8–10 cm proximal to the tip of the olecranon and directed distally through the fascia covering the lateral head of the triceps and anconeus, and ending at the subcutaneous border. The triceps was split, respecting its muscle fibers. The ulnar part of the lateral collateral ligament was left intact and the annular ligament was opened to facilitate the dislocation of the radial head in slight flexion and supination; the radial head was subsequently resected and synovitis, if present, was excised. The medial collateral ligament was released subperiostally to facilitate dislocation of the ulnohumeral joint. All humeral components were inserted without the use of cement. One of the three surgeons always placed an uncemented ulnar component (n = 28), one surgeon always cemented the ulnar component (n = 37), and the third surgeon decided whether he would use cement or not during the operation. When the uncemented component was stable enough and the bone quality was good, he used an uncemented stem (n = 19); otherwise, he cemented the ulnar component (n = 3). For the uncemented ulnar components, the aim was to insert a component with a long stem in all elbows. If medullary canal size did not allow the insertion of a long ulnar stem, a short stem was inserted. When the ulnar component was cemented, a short component was always used. All ulnar components were metal-backed.
Postoperatively, all patients performed activeassisted flexion, and pro- and supination exercises with the help of a physiotherapist. Active extension was not allowed for 6 weeks; thereafter, active and passive strengthening exercises were started. Patients wore a 90° resting splint 24 hours a day for 6 weeks.
Results
5 patients, all in the hybrid group, died on average 2.9 (1–6.5) years after TEP; the cause of death was unrelated to implantation of the elbow prosthesis. At the last follow-up of these deceased patients, the TEPs were still in place. 7 revisions had taken place in the uncemented group: 1 for loosening and fracture of the (long) ulnar component and 6 for aseptic loosening of the ulnar component after a mean follow-up of 4 (1.5–6.3) years. 3 of these ulnar components were short-stemmed, and three were long-stemmed and uncemented. In the hybrid group, no revisions had yet been performed after a mean follow-up of 4.6 (1.6–10) years.
In the uncemented group, 5 other ulnar components and 2 humeral components showed progressive radiolucencies. In the hybrid group, 2 TEPs showed progressive radiolucencies around the ulnar component. Both patients have been asymptomatic. 1 patient has radiolucencies around both the ulnar and the humeral component, 1 year after implantation. An Indium-IgG scan showed marked uptake around both components, and the patient is listed for a two-stage revision.
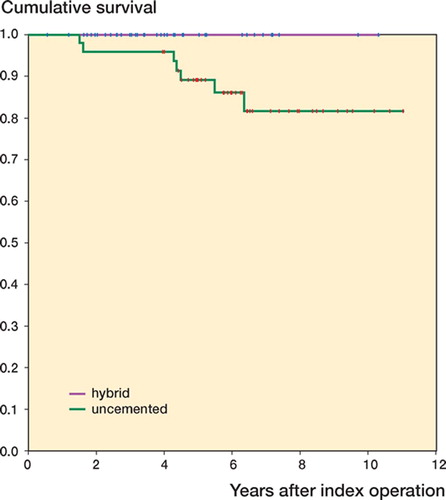
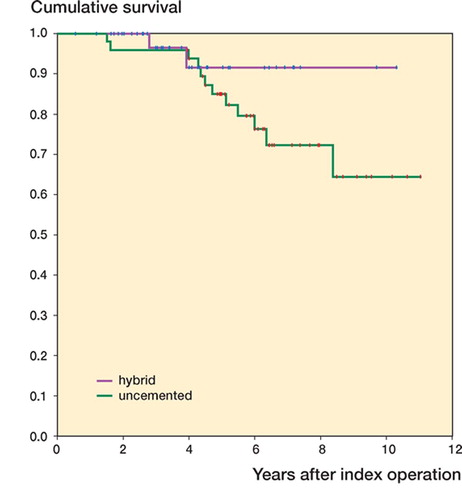
The range of motion increased postoperatively (). Pain at rest, pain with activity, and total EFA score showed a significant difference between TEPs with or without signs of loosening (). Kaplan-Meier curves with with either revision or radiolucencies as endpoint are shown in and .
Table 2. Pre- and postoperative range of motion in degrees, with standard deviation in parentheses a
Table 3. Pain at rest, pain with movement, and EFAscore (mean values) a
Discussion
In this paper we have confirmed the findings of previous studies that the ulnar component is the one most at risk of loosening (Potter et al. Citation2003, Tanaka et al. Citation2006). Furthermore, in the present series we found both revisions and radiolucencies more often in uncemented ulnar components than in cemented ones. Although the difference in results could also reflect the skills of the surgeons, and although a logistic regression analysis could not be performed because the use of cement was linked to individual surgeons, the results suggest a major role for cement. Two surgeons used uncemented ulnar components; for one surgeon 4 of 24 prosthesis were revised, and for the other surgeon 3 out of 28 were revised. For the cemented ones (n = 40), which were used by two surgeons, no revisions had been necessary.
We found the same good results as Kudo did for the humeral components (Kudo et al. Citation1980, Kudo and Iwano Citation1990). No fractures of the component and only 2 loosenings (1 infected prosthesis) contrasts sharply with published results using the type4 prosthesis, which had a fracture rate of 31% and a revision rate of 40% in Kudo’s own series (Kudo Citation1997) and comparably poor results in other studies (Reinhard et al. Citation2003).
The Kudo type-4 prosthesis was introduced for placing of an uncemented humeral component. There was, however, an unacceptably high revision rate, due especially to breakage of the humeral component at the junction of the condylar part and the stem. After modification of this junction in the type-5 prosthesis, breakage of the humeral component has been reduced.
Analyzing the type-5 Kudo prosthesis, Kudo himself found no revisions in his group with uncemented ulnar components (Kudo et al. Citation1999), but he only placed 11 uncemented components (out of a total of 43 prostheses, so 32 were cemented ulnar components) and the follow-up of mean 3 years was relatively short (Kudo et al. Citation1999). Furthermore, he found no lucency around the uncemented components (n = 11) and 2 lucencies in the cemented ones (n = 23). This contrasts with the findings of our study, the major difference between the two studies being the longer follow-up times in our study. Also, we used a metal-backed PE ulnar component in the cemented prostheses whereas Kudo used allpolyethylene components. In a recent article by Tanaka et al. (Citation2006), it was shown that all-polyeth-ylene components show less favorable results than the metal-backed ones.
Potter et al. (Citation2003) found comparably good results with cemented Kudo type-5 prostheses as we did, with only 2 of 35 ulnar components showing complete radiolucent lines after a follow-up of 5–7 years (Kudo and Iwano Citation1990). Originally, Kudo used only hybrid (humerus uncemented, ulna cemented) total elbow prostheses (Kudo et al. Citation1980), and his good results were with cemented ulnar components. Although he found no radiolucencies in the uncemented ulnar components, he still advised the use of a cemented ulnar component—which he used in 75% of the cases (Kudo et al. Citation1999).
Precise orientation of the components is essential, as the degree of motion and laxity of the elbow, wear, and loosening are significantly affected by positioning of the humeral and ulnar components, and their sizes (O'Driscoll et al. Citation1992, An Citation2005). Primary stability is a prerequisite for bone ingrowth in a cementless prosthesis. However, the primary stability of the cementless component—especially in the proximal, surface-bearing part—might often be insufficient in patients with poor bone stock due to rheumatoid arthritis. This may be the reason that these uncemented components fail more often than cemented ones. In addition, it can be assumed that with cementing of the ulnar component the surgeon is more able to place the ulnar component the way he wants; with an uncemented component, the position is harder to modify—especially the rotation.
The main achievement in this type of operation is reduction of pain (Kudo et al. Citation1994, 1999, Khatri and Stirrat Citation2005) The function after a TEP will never be the same as with a normal elbow joint (Angst et al. Citation2005, Khatri and Stirrat Citation2005), but there is a significant gain in range of motion (Kudo et al. Citation1994, 1999, Khatri and Stirrat Citation2005). A review by Little et al. (Citation2005) has shown that 38 of the 86 positive studies involving the results of implants have been from the institute of the designer of the implant. The experience of these individuals, while valuable, is not necessarily representative of the experience of orthopedic surgeons as a whole. Furthermore, many studies combine different implants (Willems and De Smet Citation2004) or different indications. In our study, only patients with RA were included and only the Kudo type-5 implants were used. The revision rate in our series is comparable to that in the review article of Little et al. (Citation2005) for the cemented ulnar component, but is much higher for the uncemented ones.
The authors wish to thank Jacques van Limbeek, M.D. Ph.D., clinical epidemiologist, for his advice concerning statistical analysis.
Contributions of authors
HH and J-MB: data collection. HH, FH, DE, and MWM: interpretation of data and statistical analysis. HH, MW, DE, FH, and MWM: preparation of the manuscript. DE and MWM: senior authors.
- An K N. Kinematics and constraint of total elbow arthroplasty. J Shoulder Elbow Surg 2005; 14: 168S–173S
- Angst F, Goldhahn J, John M, Herren D B, Simmen B R. Comparison of rheumatic and post-traumatic elbow joints after total elbow arthroplasty Comprehensive and specific evaluation of clinical picture, function, and quality of life. Orthopade 2005; 34(8)794, 796–800
- Chapman-Sheath P J, Giangrande P, Carr A J. Arthroplasty of the elbow in haemophilia. J Bone Joint Surg (Br) 2003; 85: 1138–40
- deBoer Y A, vandenEnde C H, Eygendaal D, Jolie I M, Hazes J M, Rozing P M. Clinical reliability and validity of elbow functional assessment in rheumatoid arthritis. J Rheumatol 1999; 26: 1909–17
- Fink B, Krey D, Schmielau G, Tillmann K, Ruther W. Results of elbow encloprostheses in patients with rheumatoid arthritis in correlation with previous operations. Journal of Shoulder and Elbow Surgery 2002; 11: 360–7
- Khatri M, Stirrat A N. Souter-Strathclyde total elbow arthroplasty in rheumatoid arthritis: medium-term results. J Bone Joint Surg (Br) 2005; 87: 950–4
- Kudo H. Mini-symposium: Elbow problems (i) Total elbow replacement: revision surgery, infection and biomechanics. Curr Orthop 1997; 11: 229–35
- Kudo H, Iwano K. Total elbow arthroplasty with a nonconstrained surface-replacement prosthesis in patients who have rheumatoid-arthritis. A long-term follow-up-study. J Bone Joint Surg (Am) 1990; 72: 355–62
- Kudo H, Iwano K, Watanabe S. Total replacement of the rheumatoid elbow with a hingeless prosthesis. J Bone Joint Surg (Am) 1980; 62: 277–85
- Kudo H, Iwano K, Nishino J. Cementless or hybrid total elbow arthroplasty with titanium-alloy implants. A study of interim clinical results and specific complications. J Arthroplasty 1994; 9: 269–78
- Kudo H, Iwano K, Nishino J. Total elbow arthroplasty with use of a nonconstrained humeral component inserted without cement in patients who have rheumatoid arthritis. J Bone Joint Surg (Am) 1999; 81: 1268–80
- Little C P, Carr A J, Graham A J. Total elbow arthroplasty. J Bone Joint Surg (Br) 2005; 87: 437–44
- O'Driscoll S W, An K N, Korinek S, Morrey B F. Kinematics of semi-constrained total elbow arthroplasty. J Bone Joint Surg (Br) 1992; 74: 297–9
- Potter D, Claydon P, Stanley D. Total elbow replacement using the Kudo prosthesis. Clinical and radiological review with five to seven-year follow-up. J Bone Joint Surg (Br) 2003; 85: 354–7
- Reinhard R, vander H M, deVos M J, Eygendaal D. Total elbow arthroplasty with the Kudo prosthesis. Int Orthop 2003; 27: 370–2
- Tanaka N, Sakahashi H, Ishii S, Kudo H. Comparison of two types of ulnar component in type-5 Kudo total elbow arthroplasty in patients with rheumatoid arthritis: a longterm follow-up. J Bone Joint Surg (Br) 2006; 88: 341–4
- Willems K, DeSmet L. The Kudo total elbow arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg 2004; 13: 542–7