Abstract
Background A fracture of the distal radius is considered to indicate an increased risk of future fractures, especially a hip fracture. The main causes may be osteoporosis or a tendency to fall, separately or in combination.
Methods 93 women and 5 men with a recent radius fracture and the same number of controls were measured with a heel-DXL and asked to complete one questionnaire on their quality of life (SF-36), and one on risk factors.
Results The mean T-score of the patients was –2.1, and for the controls it was –1.9 (p = 0.3). The patients aged over 64 years had a history of falling more often than the corresponding controls (p = 0.01), but there was no difference in T-score. By contrast, patients 45-64 years of age showed a non-significant, lower T-score (p = 0.09), but there was no difference concerning their history of falling. For all other risk factors, no differences were found between the patients and the controls. There were significant differences between the patients and the controls in some of the functions in the SF-36, due to the radius fracture.
Interpretation This study indicates that the underlying cause of a distal radius fracture may be different in patients aged 45–64 years and those who are more than 64 years old.
An early, peripheral low-energy fracture is considered to be a strong indication of osteoporosis (Earnshaw et al. Citation1998) with a risk of further fractures. Patients with a distal radius fracture have been found to carry twice the risk of a later fracture of the hip (Cuddihy et al. Citation1999). The increased risk of a subsequent fracture remained even when bone loss (low bone mineral density, BMD) as a risk factor was eliminated, indicating additional risk factors (Cummings et al. Citation1995).
Young and Myers (Citation2001) listed not fewer than 13 risk factors for a future hip fracture, osteoporosis being only one of them. They also found that as the number of risk factors increased, the frequency of fractures also increased. This makes effective and individually adapted preventive strategies necessary.
A low-energy distal fracture of the radius provides an important opportunity to offer the patient a review of risk factors for further fracture. Several authors have shown a marked frequency of osteoporosis in these patients (Earnshaw et al. Citation1998, Tuck et al. Citation2002, Jutberger et al. Citation2003). Thus, efforts aimed at prevention have concentrated on the need to diagnose osteoporosis and initiate treatment (Jutberger et al. Citation2003). Considering the numerous risk factors described by Young and Myers (Citation2001), further knowledge of additional factors that can contribute to a low-energy distal radius fracture is needed.
Nordell et al. (Citation2003) found lower health-related quality of life (HRQoL) scores in patients with a distal radius fracture than would be expected from Swedish normative data, a finding that was considered to indicate underlying co-morbidity and low physical activity. The tendency to fall is more common in unhealthy and physically inactive people, and is one of the most important risk factors in low-energy fracture (Hayes et al. Citation1993, Schwartz et al. Citation1998, Palvanen et al. Citation2000).
We compared the frequency of risk factors for low-energy fracture and BMD, and also HRQoL, in patients who suffered a distal radius fracture after a low-energy trauma, with a control group matched on the basis of age, gender, and municipality of residence.
Patients and methods
All patients at Sunderby Hospital, Luleå, Sweden, who sustained a distal radius fracture after a lowenergy trauma during December 2003 through December 2004, were invited to a follow-up examination at the Department of Orthopedics 10 days after sustaining their fracture, to participate in the study. The basic data for each patient were collected from the orthopedic medical records. The controls were selected randomly from the population register of Norrbotten County. They were matched against the patients with respect to age, sex, and municipality of residence. 2 controls for each patient were selected using the random generator in SPSS version 10.1. If both controls agreed to participate, the one whose date of birth was closest to that of the patient was chosen as the control subject. The subjects gave their informed consent before participation in the study. The study was approved by the Research Ethics Committee of Umeå University.
The subjects
The 98 patients (93 women and 5 men; mean age 66 and 77 years, respectively) who met the inclusion criteria but not the exclusion criteria, participated in the study. The inclusion criteria were: women born in 1958 or earlier (i.e. 45 years of age or older on December 31, 2003), men born in 1938 or earlier (i.e. 65 years of age or older on December 31, 2003), living in their own homes, and who had had a fall in the same plane resulting in a distal radius fracture. The exclusion criteria were dementia, or impairment of mental or physical health that prevented the subjects from providing correct information or completing the questionnaires at home. Both the patients and the matched group of controls were invited to a measurement of their BMD. The invitation included the questionnaire on quality of life (SF-36), and the questionnaire on risk factors (Appendix 1). The subjects completed both questionnaires at home and returned them at the time of their BMD measurement. Patients with osteopenia or osteoporosis according to the BDM measurement were referred to the primary care service. Baseline data are shown in .
Table 1. Baseline data for patients and for controls who were matched for sex, age, and county of residence
Measurement of BMD with the heel-DXL Calscan
BMD (in g/cm2) was measured with a dual Xray and laser technique, the DXL Calscan device (Demetech AB, Stockholm, Sweden). The results are shown as T- and Z-score values of the left calcaneus. Several researchers have shown that heel DXL can be used in the measurement of BMD according to the WHO criteria for the diagnosis of normal BMD, osteopenia and osteoporosis (Hakulinen et al. Citation2003. Kullenberg and Falch Citation2003).
The health survey questionnaire, short form (SF-36)
Health-related quality of life was investigated with the SF-36 questionnaire (Persson et al. Citation1998). Also, physical health (PCS) and mental health (MCS) were assessed.
The questionnaire concerning risk factors
This questionnaire contains 11 “yes or no” questions established by the Swedish Medical Products Agency (Appendix 1). The questions address, amongst other things, loss of body height and weight compared to the values at the age of 25, previous forearm or vertebral fractures, tendency to fall, smoking habits, and medical treatment for certain diseases (e.g. rheumatoid arthritis). We also asked about heredity; in other words, whether the patient's mother or father had had a hip fracture.
Missing cases
19 patients, 15 women (mean age 72) and 4 men (mean age 79), and 29 controls (mean age 69), declined their invitation to participate in the study—mainly because of lack of time and interest. There were 27 controls matched to these patients on the basis of age, sex, and county of residence who were measured and who answered the questionnaires. They did not, however, participate in the investigation as they became supernumerary when the corresponding patients with a distal radius fracture did not respond to their calls and did not come to the BMD measurement. 10 patients (mean age 66 (52–81)) and 14 controls (mean age 68 (52–94)) declined to participate in the BMD measurement, but submitted both of their questionnaires. Finally, 3 female patients failed to hand in the questionnaires. On average, 8% of the answers in the questionnaires were missing. These cases are shown as part of the results (as missing cases).
Statistics
The analyses were computed using SPSS version 10.1 software. The independent samples t-test, and Fisher's exact test were used for statistical analysis where appropriate. The level of significance was set at 0.05. The questions in the SF-36 questionnaire were investigated according to SF-scoring instructions because these issues were not studied one by one, but by the score based on the whole battery of questions.
Results
Bone mineral density (BMD) and T-score
There were no significant differences in the mean T-score or Z-score between the patients and the controls (). The T-scores indicated the presence of osteopenia in 49% of the patients and in 38% of the controls, while 25% of both the patients and the controls were found to have osteoporosis according to the WHO criteria (). When the female subjects were divided into 2 groups according to age (45–64 years and 65 and over), in the lower age group there was a trend towards a lower T-score compared to the controls (p = 0.09), while in the older age group there was no appreciable difference in T-score between patients and controls ().
Table 2. The descriptive mean T-score and mean Zscore of BMD for all patients (n = 88) and all the controls (n = 88) assessed by the heel-DXL measurement
Table 3. The mean T-score differences (the WHO criteria) between the female patients (n = 84) and the controls (n = 80) assessed by heel-DXL measurement. The subjects were divided into classes according to age
The 36-item short form (SF-36)
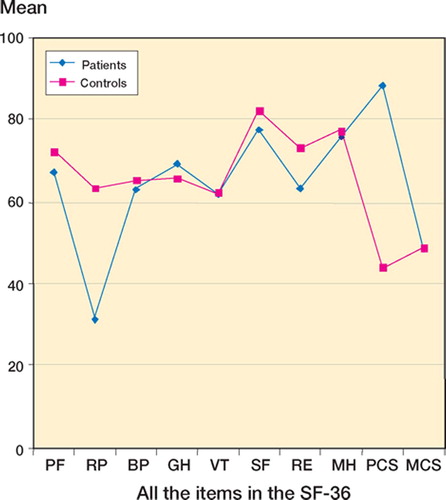
The mean score (min/max 0–100) for the factor Bodily Pain (BP) was 52 for the patients and 63 for the controls (Figure). A difference was found between the patients and the controls according to Role-Physical (RP) (p < 0.001), BP (p = 0.002) and Physical Component Summary (PCS) (p = 0.003). In the subjects with normal BMD, the patients had lower values for RP than the controls (p = 0.02). In the group with osteopenia, the patients had lower values for RP and BP (p < 0.001 and p = 0.005). No significant differences were found in the group with osteoporosis.
Figure 1. The mean scores according to the SF-36 for the patients (n = 88) and the controls (n = 84). All the items in the questionnaire are expressed: PF (Physical Function), RP (Role- Physical), BP (Bodily Pain), GH (General Health), VT (Vitality), SF (Social Function), RE (Role-Emotional) and MH (Mental Health), each with a score between 0 and 100. The sum indices of related subscores PCS (Physical Health) and MCS (Mental Health) are also shown.
The questionnaire dealing with risk factors
There were no significant differences between the patients and the controls concerning the following risk factors: previous fracture, loss of body height, cigarette smoking, or heredity—indicated by a parent with a hip fracture. However, there was a difference between the patients and the controls aged 65 years or older regarding the incidence of more than one fall in the previous year (p = 0.01, Fisher's exact test), but no such difference was found in the 45–64-year age group ().
Table 4. Breakdown of the rate of patients (n = 87) and controls (n = 82) who had more than 1 fall during the previous year. The subjects were divided into classes according to age
Discussion
This consecutive case-control study has shown that osteoporosis and osteopenia are common in the elderly, as common in those with a low-energy distal radius fracture as those in a control group matched for age, sex and municipality of residence. The similar values of BMD in the patients and controls indicate that other factors are responsible for the fracture, i.e. an increased tendency to fall. Palvanen et al. (Citation2000) showed that typical low-energy upper extremity fractures in the elderly had their typical injury mechanism, and that a tendency to fall was the most important risk factor. This is in agreement with our results, which indicate an increased tendency to fall in patients over 65 years old with a radius fracture. This was the only significant difference when these patients were compared to their matched controls. Our results are also similar to those of Lee et al. (Citation2002), who studied patients with a fracture of the proximal humerus and identified 4 predictors for fall-induced injury: a previous fall, a low level of physical activity, impaired balance, and pain in the lower extremity.
Unfortunately, the kind of fall—forward or backward, outdoors or indoors—was not documented in our study. Nevitt et al. (Citation1993) found that patients with a distal radius fracture were more likely to fall forwards or backwards, whereas those with a hip fracture were prone to fall sideways. Palvanen et al. (Citation2000) reported that patients who sustained a proximal humerus, elbow, or forearm fracture had fallen diagonally forward.
Stone et al. (Citation2003) stated that BMD predicts fractures modestly and that low BMD is not a significant risk factor for a distal radius fracture, and Hayes et al. (Citation1993) criticized the prevailing view that most hip fractures are the consequence of agerelated bone loss or osteoporosis. They showed that an increased tendency to fall is the major risk factor for fractures in the elderly. Several authors have stressed the importance of reducing risk factors for falls, in combination with exercise and increased mobility to reduce the incidence of hip fractures (Greenspan et al. Citation1994, 1998, Schwartz et al.Citation1998, Young and Myers Citation2001). Nordell et al. (Citation2005) stressed the importance of screening for fall and fracture risk, and of targeted preventive measures for patients with a distal forearm fracture, even when they appear to be healthy.
By contrast, in our patients aged 45–64 with a radius fracture, there was no significant difference in the incidence of previous falls compared to the corresponding controls. A lower, but not statistically significant T-score was noted, however. This is similar to the results of Earnshaw et al. (Citation1998), who showed that osteoporosis was more common than expected in patients under the age of 65 with a distal radius fracture, but not in patients over 65 years old. In the UK, a study on men with a distal radius fracture showed that they had a lower BMD than their healthy controls (Tuck et al. Citation2002). Kelsey et al. (Citation2005); the authors suggested that factors that protect against bone loss are likely to protect against distal radius fracture. According to our results and those of Earnshaw et al. (Citation1998), this might only be true for patients under the age of 65.
We did not find any significant differences between our patients and corresponding controls with regard to other risk factors such as a previous fracture, loss of body weight, heredity, or physical inactivity. Kannus et al. (Citation2000) showed a continuous increase in pelvic fractures related to osteoporosis in Finland. They concluded that this could not be due only to demographic changes, and they recommended urgent, effective preventive measures related to risk factors such as falling, high consumption of alcohol, smoking, and inactive life style. In our study the same proportion of patients and controls smoked cigarettes. Smoking is a risk factor for both osteoporosis and fractures. In 70-year-old women who are smokers, the risk of hip fracture increases by 41% compared to nonsmoking 70-year-old women (Law and Hackshaw Citation1997).
Health-related quality-of- questionnaires have been used previously to investigate different aspects of the clinical outcome after a distal radius fracture (McDermid et al. 2000). We found significantly lower values in the SF-36 evaluation of Role-Physical in patients with a distal forearm fracture and normal BMD or osteopenia. This difference can be ascribed—least in principle—to the radius fracture. There was, however, no significant difference between the patients with osteoporosis and a radius fracture and the controls with osteoporosis. This may indicate that among those with osteoporosis, other health-related problems are more important for their quality of life than the radius fracture. Nordell et al. (Citation2003) recommended that women with low SF-36 scores should be referred for a health review in order to prevent further falls and increased functional impairment.
The authors thank Lars Holmgren of Norrbotten County Council Research Unit, for help with the statistical analysis. This study was supported by grants from the Norrbotten County Council Research Fund (Radius fracture, U 301).
Contributions of authors
HN: collected data, performed the data analysis, and wrote the manuscript. GGP: was mainly involved in the data collection. JL: designed the study, took part in the data analysis, and revised the manuscript.
- Cuddihy M. T., Gabriel C., Crowson W., O'Fallon W., Melton L., III. Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int 1999; 9: 469–75
- Cummings S., Nevitt M., Browner S., Warren S., Stone K., Fox K., Ensrud K., Cauley J., Black D., Voigt T. Risk factors for hip fracture in white women. N Engl J Med 1995; 332: 767–73
- Earnshaw S. A., Cawte S. A., Worley A., Hosking D. J. Colle's fracture of the wrist as an indicator of underlying osteoporosis in postmenopausal woman: a prospective study of bone mineral density and bone turnover rate. Osteoporos Int 1998; 8: 53–60
- Greenspan S., Myers E., Maitland L., Resnick N., Hayes W. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. JAMA 1994; 271(2)128–33
- Greenspan S., Myers E., Kiel D., Parker R., Hayes W. Fall direction, bone mineral density, and function: Risk factors for hip fracture in frail nursing home elderly. Am J Med. 1998; 104: 539–45
- Hakulinen M., Saarakkala S., Töyräs J., Kröger H., Jurvelin J. Dual energy X-ray laser measurement of calcaneal bone mineral density. Phys Med Biol 2003; 48: 1741–52
- Hayes W., Myers E., Morris J., Gerhart T., Yett H., Lipsitz L. Impact Near the Hip Dominates Fracture Risk in Elderly Nursing Home Residents Who Fall. Calcif Tissue Int 1993; 52: 192–8
- Jutberger H., Sinclair H., Malmqvist B., Obrant K. Screening for osteoporosis. Women with distal radius fracture should be evaluated for bone density. Läkartidningen 2003; 100(1–2)31–4
- Kannus P., Palvanen M., Niemi S., Parkkari J., Järvinen M. Epidemiology of Osteoprotic Pelvic Fractures in Elderly People in Finland: Sharp Increase in 1970–1997 and Alarming Projections for the New Millennium. Osteoporos Int 2000; 11: 443–8
- Kelsey J., Prill M., Keegan T., Tanner H., Bernstein A., Quensenberry C, Jr., Sidney S. Reducing the risk for distal forearm fracture: preserve bone mass, slow down, and don't fall!. Osteoporos Int 2005; 16: 681–90
- Kullenberg R., Falch J. The Prevalence of osteoporosis using bone mineral measurements at the calcaneus by dual Xray and laser (DXL). Osteoporos Int 2003; 14: 823–7
- Law M., Hackshaw A. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ 1997; 315: 841–6
- Lee S., Dargent-Molina P. Bréart G for the EPIDOS group. Risk factors for fractures of the proximal humerus: Results of the EPIDOS prospective study. J Bone Miner Res 2002; 17: 817–25
- MacDermid J., Richards R., Donner A., Bellamy N., Roth J. Responsiveness of the short form-36, disability of the arm, shoulder and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg 2000; 25A: 330–40
- Nevitt M., Cummings S. Study of osteoporotic fractures research group. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. J Am Geriatr Soc 1993; 41: 1226–34
- Nordell E., Jarnlo G. -B, Thorngren K. G. Health-related quality of life one year after a distal forearm fracture in older women. Relationship between EQ-5D, SF-36, physical performance and comorbidity. Lund University. 2003, Thesis
- Nordell E., Kristinsdottir E., Jarnlo G.-B., Magnusson M., Thorngren K. G. Older patients with distal forearm fracture. A Challenge to future fall and fracture prevention. Aging Clin Exp Res 2005; 17(2)90–5
- Palvanen M., Kannus P., Parkkari J., Pitkäjärvi T., Pasanen M., Vuori I., Järvinen M. The injury mechanisms of osteoporotic upper extremity fractures among older adults: A controlled study of 287 consecutive patients and their 108 controls. Osteoporos Int 2000; 11: 822–31
- Persson L. O., Karlsson J., Bengtsson C., Steen B., Sullivan M. The Swedish SF-36 Health Survey II: Evaluation of clinical validity: Results from population studies of elderly women in Gothenburg. J Clin Epidemiol 1998; 51: 1095–103
- Schwartz A., Kelsey J., Sidney S., Grisso J. Characteristics of falls and risk of hip fracture in eldely men. Osteoporosis Int 1998; 8: 240–6
- Stone K., Seeley D., Lui L. Y., Cauley J., Ensrud K., Browner W., Nevitt M., Cummings S. BMD at multiple sites and risk of fracture of multiple types: Long-term results from the study of osteoporotic fractures. J Bone Miner Res 2003; 18: 1947–54
- Tuck S., Raj N., Summers G. Is distal forearm fracture in men due to osteoporosis?. Osteoporos Int 2002; 13: 630–6
- Young Y., Myers A., Provenzano G. Factors associated with time to first hip fracure. J Aging Health 2001; 13(4)511–25
Appendix 1