Abstract
Background Elastic, stable intramedullary nailing (ESIN) with titanium nails is a promising minimally treatment for displaced midclavicular fractures, which may be an alternative to plate fixation (ORIF) or even nonoperative treatment. We describe the surgical technique and outcome in 87 patients.
Methods The nail was inserted at the medial inferior end of the clavicle in 83 patients and in the acromial end in 12 patients. An open fracture reduction via an additional small incision was necessary in 53 patients and closed manoeuvre was successful in 42. Implant removal was performed in 82 patients.
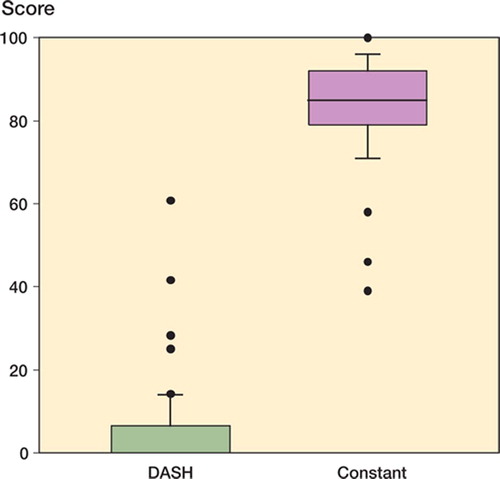
Results The functional status of 87 patients after 13 months reached 6.8 (0–43) points on the DASH score and 81 (46–100) points on the self-reported Constant score. The fracture healed in correct anatomical axis in 80 of 87 patients, 2 cases ended in a nonunion. Implant migration of the nail occurred in 4 patients, who required early implant removal. Repeated nailing was necessary in 2 patients in whom the nail missed the lateral medullar canal, and plate fixation was necessary in 2 other patients who had secondary dislocation after early nail removal.
Interpretation Flexible intramedullary nailing, a minimally invasive technique for stabilization of displaced midshaft clavicle fractures, has minor risks and complications.
Treatment of dislocated midshaft clavicle fractures is still controversial (Denard et al. Citation2005, Zlowodzki et al. Citation2005). In most cases, nonoperative treatment is favored and leads to a good result (Nordqvist et al. Citation1998). Regarding displaced midshaft fracture types, the rate of nonunion is up to 15% (Hill et al. Citation1997) and a high rate of sequelae in almost half of the patients, even after 9 years, has been reported (Nowak et al. Citation2005). Thus, operative treatment should be considered in fractures with marked shortening or gross dislocation of the clavicle. However, surgical procedures using plate fixation have shown major complications such as hematoma, infections, implant failures and nonunion (Schwarz and Hocker Citation1992, Bostman et al. Citation1997, Shen et al. Citation1999, Denard et al. Citation2005, Duncan et al. Citation2005).
We analyzed the results of a new minimally invasive procedure based on the use of elastic, stable intramedullary titanium nails.
Patients and methods
From January 2001 to September 2005, we operated 95 patients (68 men) with midshaft clavicle fractures using elastic titanium nails (Synthes, Umkirch, Germany (TEN) or DePuy, Kirkel-Lim-bach, Germany (ECMES)). The mean age of the patients was 38 (15–74) years. Inclusion criteria were displaced fractures with a displacement of more than shaft width, shortening by over 2 cm, angulations of over 30°, open fractures, or threat of skin perforations at fracture ends. 5 patients who developed progressive displacement under closed treatment had later nail fixation.
Operative technique
The patient lies supine on a radiolucent table with free range of motion of the arm. A small incision of 1–1.5 cm is made under the sternal end of the clavicle. In 83 cases, a medial entry point was selected and a lateral-dorsal entry point was chosen in only 12 patients with shorter lateral fragments. The anterior inferior edge of the cortex is opened after soft tissue dissection with an awl or a drill bit. A flexible titanium nail with an average thickness of 2.5–3.5 mm is mounted on a Jacob’s chuck, and is inserted forward in the medullary canal manually. The selection of the nail is determined according to the diaphyseal diameter.
The small and flattened tip serves for adjustment of the nail and prevents perforation through the cortex. The original curvature of the nail tip should be straightened slightly, however, in order to facilitate better gliding in the small medullary canal. With image intensification, the implant is advanced to the fracture site. When the tip reaches the fracture, reduction is performed manually or percutaneously by means of a reduction clamp, inserting the nail into the lateral fracture fragment (). If this does not succeed, the tip of the nail is introduced under direct view after performing a second small (2–3-cm) skin incision directly over the fracture site. The sparingly exposed soft tissue, which is sometimes interposed, should be closed and fixed with few fascia and periosteal sutures over the fracture after reduction. The nail is then advanced manually or gently tapped with a hammer until it is just medial to the AC joint. At the transition to the acromional end of the clavicle, the tip of the nail is likely to perforate the curved thin dorsal cortex; thus, accurate maneuvering of the tip is necessary under image intensifier control. After reaching the end position, the nail is cut close to the entry point in order to minimize soft tissue irritation, at the same time leaving sufficient surface for extraction later.
Figure 1. Percutaneous reduction of a displaced midshaft clavicle fracture (left panel) and intraoperative fluoroscopy after guiding the tip of the nail in the outer fragment (right panel).
For postoperative pain control, a sling or Gilchrist bandage is given for a few days. Active movements of the shoulder (over 90° abduction or flexion) should be limited for 6 weeks, since increasing rotational loads on the clavicle may result in proximal migration of the nail, especially in comminuted fractures. The operations were performed by 8 different surgeons. The average operation time was 53 (10–130) min. In 42 cases of closed reduction, the operation took 32 (10–75) min. An open fracture reduction was needed in 53 cases, with an average operation time of 63 (25–130) min. Excluding the 5 multiply-injured patients, the length of stay in hospital with isolated clavicle fractures was 3 (1–6) days.
Implant removal is recommended after radiographic fracture consolidation, after 10 weeks at the earliest and not later than 12 months. The implant can be removed easily with strong extraction forceps, under local or general anaesthesia depending on the patient’s desire.
Follow-up
8 patients were lost to follow-up; no early complications occurred in these patients. 87 patients were evaluated after mean 13 (6–28) months. Outcome was assessed by the standardized subjective DASH score: 0 (best) to 100 (worst) (Beaton et al. Citation2001). In addition, shoulder function was measured with the self evaluated Constant score (maximum 100 points) (Boehm et al. Citation2004). Subjective data were evaluated with reference to the cosmetic outcome (malunion, asymmetry, scar formation). In the first post-surgical radiographs in two planes, the implant position (correct, miss, perforation) and the quality of reduction (anatomical reduction, dislocation until or over shaft width) were evaluated. In the later follow-up after 6–12 weeks and also as after implant removal, the nail position (correct, dislocation, hardware removal), bone healing (nonunion, proper or hypertrophic callus) and the alignment of the clavicle (axial deviation ≤ 30°, axial deviation < 30°, fracture dislocation over shaft width or shortening) were evaluated.
Results
The mean DASH score in the 87 patients was 6.9 (0–43) points (). Only 6 patients had a DASH score result of over 10 points, due to restriction in their activities of daily living. The selfevaluated Constant score indicated a good overall result with an average of 84 (46–100) points. On average, inability to work lasted 3 weeks. 81 of the 87 patients were content with the cosmetic outcome and only 6 patients complained of irritation or scar formation at the medial entry point.
Figure 2. Box plot of the DASH score (0 = best result) and Constant score (100 = best result) for 87 elastic stable intramedullary nailings after an average of 13 months
In 2 cases, the protruding end of the nail at the medial side caused irritation. In 2 patients, the nail missed the medullary canal of the lateral fragment. 1 patient underwent a second operation to reintroduce the nail; the other refused a further operation and the fracture healed with a slight malunion.
Fracture healing occurred in correct alignment in 80 of 87 patients ( and ). 3 patients healed with angulations of over 30° and 4 had a dislocation of more than a shaft width. Shortening of more than 1 cm was found in 2 patients. This was due to intraoperative bone excision in 1 patient and overlapping bone consolidation after premature nail extraction in the other. The bone healing was judged as optimal in 81 patients, while in 4 patients a hypertrophic callus formation—but without neurological symptoms—was seen. In 2 patients a nonunion persisted. An atrophic nonunion was seen in a 42-year-old smoker with the nail in situ for 12 months; however, she remained clinically asymptomatic. A second patient with a nonunion after premature implant removal had a plate fixation after 6 months.
Figure 3. Displaced midclavicular fracture in a 27-year-old man (upper panel). Correct healing after elastic stable intramedullar nailing (middle panel) and radiograph after implant removal (lower panel).

Figure 4. Lateral nailing (ESIN) of a displaced fracture in a 32-year-old man (upper and middle panels) and after implant removal 5 months later (lower panel).

The implant was removed in 82 patients after an average of 4 (1.5–14) months. In 66 patients the implant was removed under local anesthesia.
We observed no infections or hematomas (). Soft tissue irritation at the entry point— caused by the nail—was present in 4 patients, and hypertrophic scars formed in 4. 2 patients complained about pain resulting from load over the fracture. In 4 patients nail dislocations (3 lateral, 1 medial) occurred, which made earlier implant removal necessary. In 2 of these cases overuse of the extremity was described by the patients. Due to a skiing accident, one patient refractured the consolidated clavicle 1 year after surgery. Osteosynthesis with the flexible intramedullary nail was performed with open reduction, whereby the sclerotic fracture ends had to be drilled for passage of the nail. The fracture healed uneventfully and the nail was removed after 3 months.
Table 1. Complications in 87 elastic stable intramedullary nailings
Discussion
In most non-displaced clavicular fractures, good functional results can be obtained with nonoperative treatment (Nordqvist and Petersson Citation1994, Nordqvist et al. Citation1998, Robinson Citation1998, Zlowodzki et al. Citation2005). Displacement of more than 1 cm or comminution leads to inferior results if treated nonoperatively (Zlowodzki et al. Citation2005). Unsatisfactory results in one-third of cases was reported by Hill et al. (Citation1997) and in a systematic review the rate of nonunions was found to be 15% (Zlowodzki et al. Citation2005). A prospective randomized study by Smith et al. (Citation2001) demonstrated 12 nonunions in 35 displaced clavicle fractures treated nonoperatively. Jupiter et al. (Citation1987), Wick et al. (Citation2001), and Lazarides and Zafiropoulos (Citation2006) found that complete displacement or shortening of the fracture is a predisposing factor for nonunion and they thus advocated surgery in such cases. Furthermore, Nowak et al. (Citation2005) showed in a prospective study that 93 of 222 patients (42%) still had sequelae 9 years after trauma. In cases with open clavicle fractures, threat of skin perforation by fracture ends, complete displacement or neurovascular compromise, open reduction and internal fixation is indicated (Bostman et al. Citation1997, Enneking et al. Citation1999, Denard et al. Citation2005).
Due to the high complication rate with plate fixation, such as soft tissue infection, implant failure, nonunion, and poor cosmetic appearance of the incision (Bostman et al. Citation1997), it is advisable to use intramedullary nails (Chu et al. Citation2002, Jubel et al. Citation2003). However, steel nails or wires, which were used nearly 100 years ago by A. Lambotte, are also associated with increased complications such as infection, nonunion, implant migration, or implant breakage (Schwarz and Leixnering Citation1984, Leppilahti and Jalovaara Citation1999, Grassi et al. Citation2001). Thus, this technique has not gained widespread acceptance (Jubel et al. Citation2002).
Elastic stable intramedullary nailing (ESIN) through a titanium nail with increased bending rigidity is a new concept. In constrast to Knowles pinning, predrilling of the intramedullary canal is not necessary (Chu et al. Citation2002). Jubel et al. (Citation2003) and Walz et al. (Citation2006) concluded from their treatment of small groups of patients with clavicle fractures (53 and 35, respectively) that ESIN is a minimally invasive surgical technique that leads to excellent functional and cosmetic results.
We evaluated 87 patients using these intramedullary titanium nails at an average follow-up time of 13 months. Only 2 patients showed a nonunion, and 2 other patients had a malunion. These numbers are clearly superior to the complication rate reported by Bostman et al. (Citation1997) when using a plate fixation.
The better results of ESIN as compared to plate fixation might be due to the smaller incision with less soft tissue dissection. Bending and torsional loads in the clavicle are better compensated for by an intramedullary flexible nail than a rigid plate, which is only fixed on one side of the bone. This might be the reason for the increased rate of loosening that has been reported, especially with the use of short plates (Bostman et al. Citation1997).
Other complications of plate fixation, such as soft tissue infection, hematoma, or implant breakage are uncommon with the use of a titanium nail. In our study, we found 10 complications with 4 revisions being necessary. This is in agreement with the study of Jubel et al. (Citation2003). Walz et al. (Citation2006) noted only 1 complication in 35 patients.
Compared with intramedullary nailing with unreamed or reamed steel wires, the risk of implant dislocation is lower because of a stable jamming of the flexible titanium nail in the clavicle at its flat outer end (Jubel et al. Citation2003). In order to obtain a good locking, the nail must be brought as far as possible into the lateral fragment. Thus, difficulties may develop with short lateral fragments or comminuted fractures with intermediary fragments (Stotzer Citation2005). Perforation of the tip, which could result in a lateral dislocation of the implant, just at the thin dorsolateral cortex should be prevented. Thus, appropriate preforming of the tip and accurate intraoperative image intensification in a minimum of 2 planes is advisable. The risks described—as well as disturbing irritation at the entry point—are reduced or entirely avoidable if correct intraoperative technique is followed. If close reduction does not succeed, the tip of the implant should be guided directly over a small skin incision. Compared to plate removal, nail extraction is a simple intervention and can be performed as an outpatient procedure in most patients under local anesthesia.
We advocate this minimally invasive method as a reliable technique for the treatment of displaced midclavicular fractures without bone contact.
We thank Dr Amarnath Surath, Dr K. Karthik Narayan, and Dr. Markus Tingart for reviewing the manuscript.
No benefits in any form were received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributions of authors
MKe, MS and WM: main surgeons. VB and MKö: performed part of clinical and radiographic follow-up. All authors participated in the design of the study, interpretation of the results, and in elaboration of the manuscript. MKe: mainly responsible for designing the study and writing the paper, incorporating input from all authors.
References
- Beaton D E, Katz J N, Fossel A H, Wright J G, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther 2001; 14: 128–46
- Boehm D, Wollmerstedt N, Doesch M, Handwerker M, Mehling E, Gohlke F. Development of a questionnaire based on the Constant-Murley-Score for self-evaluation of shoulder function by patients. Unfallchirurg 2004; 107: 397–402
- Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 1997; 43: 778–83
- Chu C M, Wang S J, Lin L C. Fixation of mid-third clavicular fractures with knowles pins: 78 patients followed for 2-7 years. Acta Orthop Scand 2002; 73: 134–9
- Denard P J, Koval K J, Cantu R V, Weinstein J N. Management of midshaft clavicle fractures in adults. Am J Orthop 2005; 34: 527–36
- Duncan S F, Sperling J W, Steinmann S. Infection after clavicle fractures. Clin Orthop 2005, 439: 74–8
- Enneking T J, Hartlief M T, Fontijne W P. Rushpin fixation for midshaft clavicular nonunions: good results in 13/14 cases. Acta Orthop Scand 1999; 70: 514–6
- Grassi F A, Tajana M S, D'Angelo F. Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma 2001; 50: 1096–100
- Hill J M, McGuire M H, Crosby L A. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg (Br) 1997; 79: 537–9
- Jubel A, Andermahr J, Schiffer G, Rehm K E. Technique of intramedullary osteosynthesis of the clavicle with elastic titanium nails. Unfallchirurg 2002; 105: 511–6
- Jubel A, Andermahr J, Schiffer G, Tsironis K, Rehm K E. Elastic stable intramedullary nailing of midclavicular fractures with a titanium nail. Clin Orthop 2003, 408: 279–85
- Jupiter J B, Leffert R D. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg (Am) 1987; 69: 753–60
- Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg 2006; 15: 191–4
- Leppilahti J, Jalovaara P. Migration of Kirschner wires following fixation of the clavicle-a report of 2 cases. Acta Orthop Scand 1999; 70: 517–9
- Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop 1994, 300: 127–32
- Nordqvist A, Petersson C J. Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma 1998; 12: 572–6
- Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: a prospective study of 222 patients. Acta Orthop 2005; 76: 496–502
- Robinson C M. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg (Br) 1998; 80: 476–84
- Schwarz N, Hocker K. Osteosynthesis of irreducible fractures of the clavicle with 2.7-MM ASIF plates. J Trauma 1992; 33: 179–83
- Schwarz N, Leixnering M. Failures of clavicular intramedullary wire fixation and their causes. Aktuelle Traumatol 1984; 14: 159–63
- Shen W J, Liu T J, Shen Y S. Plate fixation of fresh displaced midshaft clavicle fractures. Injury 1999; 30: 497–500
- Smith C A R J, Crosby L A. Results of operative versus nonoperative treatment of 100% displaced mid-shaft clavicle fractures (abstract). Proceedings From the 68th Annual Meeting of the AAOS, San Francisco, 2001
- Stotzer J. Thoracic inlet syndrome after ESIN of comminuted clavicular fracture. Unfallchirurg 2005; 108: 507–10
- Walz M, Kolbow B, Auerbach F. Elastic, stable intramedullary nailing in midclavicular fractures - a change in treatment strategies?. Unfallchirurg 2006; 109: 200–11
- Wick M, Muller E J, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg 2001; 121: 207–11
- Zlowodzki M, Zelle B A, Cole P A, Jeray K, McKee M D. Treatment of acute midshaft clavicle fractures. J Orthop Trauma. systematic review of 2144 fractures: on behalf of the Evidence–Based Orthopaedic Trauma Working Group. 2005; 19: 504–7
