Abstract
Background Bone-saving hip arthroplasty techniques, which facilitate revision, are gaining importance as the number of hip replacements in younger patients increases.
Patients and methods 123 CUT femoral neck prostheses (ESKA Implants, Lübeck, Germany) were implanted in 113 patients (average age 53 years) between 1999 and 2002. After a mean follow-up of 5 (3–7) years, we determined the state of 120 prostheses; 3 patients could not be located. 97 patients with 107 prostheses, none of which had been revised, were evaluated clinically and radiographically.
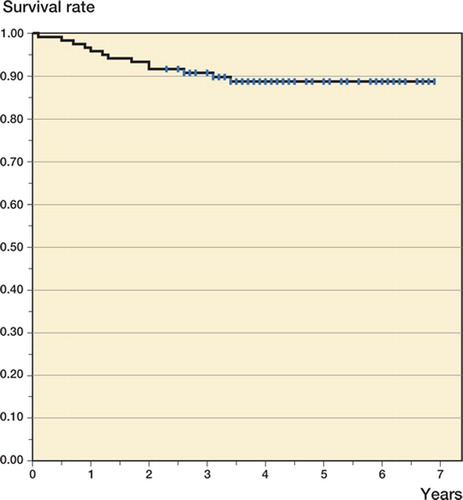
Results The median Harris hip score improved from 51 points to 92 points in the unrevised hips. 13 CUT prostheses (11%) had been revised, 7 because of aseptic loosening, 3 because of persisting thigh pain, 1 because of immediate vertical migration, and 2 because of septic loosening. The 5-year survival rate of the CUT prosthesis was 89%.
Interpretation The medium-term survival with this type of femoral component is unsatisfactory, with a high rate of aseptic loosening. The surviving prostheses had a good clinical outcome.
As the number of younger patients undergoing total hip arthroplasty is increasing, bone-saving implantations with a view to easier revisions are gaining in importance (Walker et al. Citation2005).
This has led to the development of hip prostheses that cause only slight bone loss (Birkenhauer et al. Citation2004, Hube et al. Citation2004, Thomas et al. Citation2004, Witzleb et al. Citation2004, Walker et al. Citation2005). One of them is the femoral neck prosthesis CUT (ESKA Implants, Lübeck, Germany), which was first introduced in 1998 by W. Thomas in Rome. Only short-term results have been published, however, based on a small number of patients (Thomas and Grundei Citation1999, Citation2001, Specht et al. Citation2003). We therefore report our results with 120 hips followed for at least 3 years.
Patients and methods
The CUT prosthesis is a femoral component for total hip arthroplasty with cementless metaphyseal fixation (Thomas and Grundei Citation2001, Thomas et al. Citation2004). Saving the femoral neck, only the femoral head is resected subcapitally (). Osteoporosis, coxa valga with a CCD angle of > 155°, coxa vara with a CCD angle of < 120°, heavy adiposity, and previous operations in the metaphyseal area of the proximal femur are contraindications. The prosthesis consists of two components (body and adapter), both of which are made of a titanium alloy. The surface of the prosthesis has a threedimensional spongy metal structure (tripods). The proximal part of the prosthesis is oval in shape. The distal, curved part becomes narrower at its tip. The surgeon can choose between prostheses of different sizes. The shape of the prosthesis is neutral, for use on both the left and the right side.
Figure 1. Standard anteroposterior radiograph of the pelvis with regular position of the CUT prosthesis. No signs of loosening 4 years after surgery.
Between 1999 and 2003, we implanted 123 cementless CUT femoral neck prostheses (ESKA Implants, Lübeck, Germany) at the Department of Orthopedic Surgery, Otto-von-Guericke-University, Magdeburg (56 prostheses) and at the Department of Orthopedic Surgery and Traumatology, Medical Center, Brandenburg (67 prostheses). This involved 113 patients; 10 received a CUT prosthesis bilaterally. The CUT prosthesis was combined with the following cementless cups. Press-fit-cups: 67 Standard type (ESKA Implants, Lübeck, Germany) and 38 Allofit type (Centerpulse/Zimmer, Winterthur, Switzerland); threaded cups: 12 Variall type (Centerpulse/Zimmer, Winterthur, Switzerland) and 6 Hofer-Imhof type (Endoplus, Marl, Germany). Regarding the sliding combination (acetabular liner/femoral head), ceramic/ceramic was used for 94 prostheses (76%), polyethylene/ ceramic for 4, polyethylene/metal for 17, and metal/metal for 8.
A lateral Watson-Jones approach was used in all cases. All patients were given perioperative antibiotics and postoperative thromboembolism prophylaxis with a low-molecular-weight heparin derivative. Immediate (Magdeburg) full weight bearing or partial weight bearing (50% body weight for 6 weeks, Brandenburg) was allowed from the first postoperative day. Two surgeons, well experienced in the field of total hip arthroplasty, carried out the implantations at the respective departments (WN and HG; AE and TK).
Implantation was performed because of primary osteoarthrosis in 91 cases (74%) and because of secondary osteoarthrosis in the remaining 32 cases (osteonecrosis of the femoral head in 24 cases and developmental hip dysplasia in 8). Only patients with a BMI value of < 40 kg/m2, a good bone structure, and aged under 70 were included. The average age of the 113 patients at the time of surgery was 53 (32–69) years.
3 patients (3 prostheses) were lost to follow-up and 13 prostheses had been revised before final follow-up. The remaining 97 patients (107 replacements) were evaluated clinically and radiographically after mean 5 (3–7) years. The follow-up evaluation was done independently by the first author.
Clinical evaluation was done using the Harris hip score (HHS) (Harris Citation1969). The radiographic examination included a standard anteroposterior radiograph of the pelvis under full weight bearing in both legs, with the central beam directed to symphysis, and a lateral radiograph of the operated hip. The amount of femoral neck resection, the alignment of the CUT prosthesis (varus, neutral, valgus, recommended implant angle 145°), the contact of the medial corticalis with the proximal stem, and the contact of the lateral corticalis with the distal part of the stem were evaluated. Implant migration was assessed according to Martell et al. (Citation1993) and implant stability according to Engh et al. (Citation1987), with the bone-implant interface of the stem subdivided into 5 areas for determination of radiolucent lines (< 1 mm, 1–2 mm, > 2 mm) and osteolyses (). Radiographic loosening of the implant was diagnosed when there was a change in position (migration of > 3 mm) horizontally or vertically, and/or when there was a continuous radiolucent line wider than 2 mm (Kim et al. Citation2003). We also noted changes in the corticalis (atrophy/hypertrophy) in the five zones and changes of the calcar (atrophy/hypertrophy).
Figure 2. Subdivision of the bone-stem interface into 5 zones after Gruen et al. (Citation1979) and Thomas et al. (2001).
The cups were evaluated radiographically with regard to radiolucent lines and osteolyses in the zones described by DeLee and Charnley (Citation1976). The angles of the cups were calculated according to Martell et al. (Citation1993); cup migration was determined as described by Thoren and Sahlstedt (Citation1990).
Statistics
Statistical evaluation was done using the t-test and the Chi-square test according to Pearson. All statistical calculations were based on an error probability of 5%. The survival rate was calculated according to Kaplan-Meier.
Results
The average HHS improved from 51 (10–78) points preoperatively to 92 (63–100) at the time of final follow-up. 91% (n = 97) had good or very good results (81 to 100 points). We could not find any association between the postoperative mobilization scheme (full or partial weight bearing) and outcome.
The radiographical examination showed correct resection of the femoral head (femoral neck not engaged) in 95 prostheses. 92 prostheses had an unchanged neutral stem position, 7 had an unchanged valgus position, and 2 had an unchanged varus position. In 5 cases, we noted a change from the postoperative neutral position to a varus position and in 1 case the postoperative varus position had increased (1–3°, 5 × 2°, 1 × 3°).
4 CUT prostheses had no optimal contact with the medial corticalis and 11 had no optimal contact between the tip of the stem and the lateral corticalis. These 15 prostheses had good clinical outcome and no migration.
Following Engh et al. (Citation1987), we noted fixation by bone ingrowth in 98 CUT prostheses, stable fibrous ingrowth in 7, and 2 implants were judged as being unstable (progressive migration) (> 5°).
Radiolucent lines were noted only in zones 1 and 4. An isolated radiolucent line of > 1 mm was noticed in zone 1 in 13 prostheses, and in zone 4 in 3 prostheses. A radiolucent line of 1–2 mm was noted in zones 1 and 4 in 2 prostheses, and a radiolucent line of > 2 mm was noted in 1 prosthesis. No cases had uninterrupted radiolucent lines and osteolyses around the stem. There was no association between the presence of radiolucent lines and clinical complaints (p = 0.8, t-test).
6 prostheses had horizontal stem migration, with the proximal and distal parts of the stem migrating medially and laterally, respectively. There was no vertical migration of the stem. We noted progressive stem migration with varization of the stem in 2 cases that had undergone complete resection of the femoral neck. One patient complained of chronic strain-dependent pain, whereas the second patient had only slight pain (). 4 prostheses showed no progression of the migration, and these patients had good clinical results. The femoral head was correctly resected in 3 cases, and the resection was too wide in 1 patient. None of the cups showed osteolysis or migration.
Figure 3. Standard anteroposterior radiograph of the pelvis with marked horizontal migration of CUT prosthesis with complete resection of the femoral neck 5.1 years postoperatively. The patient complained of slight pain (pain score 40 points by HHS) without any correlation with the radiographical finding. Regular position of right-sided cementless total hip replacement with standard stem.

13 revised CUT prostheses
The CUT prosthesis had to be replaced with a cementless standard stem in 11 cases, for the following reasons: strong chronic thigh pain in 3 cases (1, 1.3, and 2 years postoperatively); aseptic loosening in 7 cases (0.5–3.5 years postoperatively); and stem subsidence in 1 case (undersized prosthesis, revised on the ninth postoperative day). We found a radiographic correlation with the chronic thigh pain in only 1 case; demineralization was obvious in the medial corticalis (zone 5) and in the area of the trochanter major (zone 1). The stem was correctly positioned in all 3 cases, with no radiographic signs of loosening, and an intraoperatively the prostheses were well integrated. In 1 case, the femoral neck was resected too widely. In the 7 cases with aseptic loosening, the femoral neck had been resected in 5 cases followed by progressive horizontal migration and varization of the stem. In all of these 11 cases in which the stem was replaced, the well-fixed cups were not exchanged.
1 case was revised 2 years postoperatively because of hip pain, and synovitis was found intraoperatively during revision. Results of microbiological analysis were negative. The stem was correctly positioned without impingement; there were no radiographic signs of loosening, and intraoperatively the components were found to be well fixed. Soft tissue revision with replacement of the femoral head gave pain relief.
2 patients had to undergo soft tissue revision (2 and 4 years postoperatively) because of a heterotopic ossification (grade 4) with restricted range of motion and pain. 2 replacements had to be completely removed because of septic loosening (1 and 2 years postoperatively).
The 5- year survival rate of the CUT prosthesis was 89% with exchange as an endpoint (), and 85% with revision surgery as an endpoint.
Figure 4. Survival rate of the CUT prosthesis according to Kaplan-Meier (1958) with exchange of the CUT prosthesis as endpoint.
In 1 case, a cup had to be replaced with a cemented cup because of aseptic loosening 2.5 years postoperatively; the well-fixed CUT prosthesis was not changed.
Discussion
The CUT prosthesis had a good clinical outcome in nine-tenths of the unrevised patients. Regarding the medium-term follow-up, the cementless Zweymüller stem (Centerpulse/Zimmer, Winterthur, CH) has been reported to give clinical results similar to ours (Huo et al. Citation1995, Delaunay et al. Citation1998, Wurnig et al. Citation1999). The Zweymüller stem has also given good results during long-term followup (Traulsen et al. Citation2001, Weissinger et al. 2001, Pospischill et al. 2005).
The insertion of the CUT prosthesis is demanding, and requires resection of the femoral head but not of the femoral neck. Evaluation of all radiographs taken postoperatively (n = 123) showed that 12 (67%) of the 18 cases in whom the femoral neck was partly or fully resected were operated within the first year of introduction of the prosthesis. Thus, there seems to be a learning curve for this prosthesis— even when used by experienced surgeons.
In 6 cases, we observed horizontal stem migration (varization); in 2 of the cases this was progressive. A complete resection of the femoral neck had been done in both cases, which were subsequently revised. In the other 4 prostheses with no progression of migration, the femoral head was correctly resected in 3 cases and the resection was too wide in 1 case. We do not know whether the long-term outcome would be influenced by these deviations.
Periprosthetic radiolucent lines occurred in 18 (17%) of the stems, and they were restricted to zones 1 and 4. The majority of them were < 1 mm. Cementless standard stems show the same or higher rates of radiolucent lines after similar follow-up periods (Hösli Citation1993, Hofmann et al. Citation2000, Sinha et al. Citation2004). We found no association between the presence of radiolucent lines and clinical complaints.
13 (11%) of the 120 CUT stems whose state could be ascertained were revised (exchanged) during the follow-up period. The 89% survival rate resulting from this is unsatisfactory in comparison to the rates of 99–100% reported for cementless standard stems at medium-term follow-up (Delaunay et al. Citation1998, Eyb et al. Citation1993, Aldinger et al. Citation2003, Grübl et al. Citation2003, Jacobsen et al. Citation2003, Reikeras and Gunderson Citation2003).
The CUT prosthesis was replaced in 7 cases due to aseptic loosening (6%). Other short-stem prostheses with metaphysial fixation show similar rates of aseptic loosening at medium-term followup (Morrey et al. Citation2000, Effenberger et al. Citation2005). Considering its learning curve and the demanding implantation technique involved, the CUT prosthesis is no alternative to standard stems for young patients in the hands of a surgeon who has little experience in implanting the CUT prosthesis.
The authors state that they have had no relations with companies whose products have been mentioned in this article, or to companies selling competitive products.
Contributions of authors
SAE: coordination of the follow-up evaluation of patients from Magdeburg, and last follow-up evaluation. AM and GP: study design. JH: coordination of the follow-up evaluation of patients from Brandenburg. HG: surgeon (Magdeburg) and adviser. HWN: surgeon (Magdeburg) and senior author.
references
- Aldinger P R, Thomsen M, Mau H, Ewerbeck V, Breusch S J. Cementless Spotorno tapered titanium stem. Excellent 10-15 year survival in 141 young patients. Acta Orthop Scand 2003; 74(3)253–8
- Birkenhauer B, Kirstmacher H, Ries J. Conception and first results of the Spiron cementless femoral neck screw prosthesis. Orthopäde 2004; 33: 1259–66
- Delaunay C, Cazeau C, Kapandji A I. Cementless primary total hip replacement. Four to eight year results with the Zweymueller-Alloclassic prosthesis. Int Orthop 1998; 22: 1–5
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Effenberger H, Imhof M, Witzel U, Rehart S. Cementless stems of the hip. Current status. Orthopäde 2005; 34: 477–502
- Engh C A, Bobyn J D, Glassman A H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg (Br) 1987; 69: 45–55
- Eyb R, Kutschera H P, Schartelmueller T, Toma C, Zweymueller K. Midterm experience with the cementless Zweymüller system. Results of a minimum five-year follow-up study. Acta Orthop Belg (Suppl 1) 1993; 59: 138–43
- Grübl A, Csepan R, Delaunay C, Gördes W, Kaider A, Parzer R, Zenz P, Gottsauner-Wolf F. Six to ten year results of use of the Alloclassic hip prosthesis – a multicentre survival analysis. Z Orthop 2003; 141: 303–8
- Gruen T A, McNeice G M, Amstutz H C. Modes of failure of cemented stem-type femoral components. A radiographic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by Mold arthtoplasty. An end result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51: 737–55
- Hofmann A A, Feign M E, Klauser W, VanGorp C C, Camargo M P. Cementless primary total hip arthroplasty with a tapered, proximally porous-coated titanium prosthesis. A 4- to 8-year retrospective review. J Arthroplasty 2000; 15: 833–9
- Hösli P. Zementfreie Hüftendoprothetik: PCA-Schaftprothesen 5-7 Jahresresultate. Z Orthop 1993; 131: 518–23
- Hube R, Zaage M, Hein W, Reichel H. Early functional results with the Mayo-hip, a short stem system with metaphyseal-intertrochanteric fixation. Orthopäde 2004; 33: 1249–58
- Huo M H, Martin R P, Zatorski L E, Keggi K J. Total hip arthroplasty using the Zweymueller stem implanted without cement. A prospective study of consecutive patients with minimum 3-year follow-up period. J Arthroplasty 1995; 10: 793–9
- Jacobsen S, Jensen F K, Poulsen K, Sturup J, Retpen J B. Good performance of a titanium femoral component in cementless hip arthroplasty in younger patients: 97 arthroplasties followed for 5-11 years. Acta Orthop Scand 2003; 74(4)375–9
- Kaplan E L, Meier P. Nonparametric estimation from incomplete observation. Am Stat Ass J 1958; 53: 457–81
- Kim Y H, Oh S H, Kim J S. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg (Am) 2003; 85: 109–14
- Martell J M, Pierson R H, Jacobs J J, Rosenberg A G, Maley M, Galante O. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg (Am) 1993; 75: 554–71
- Morrey B F, Adams R A, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg (Br) 2000; 82: 952–8
- Popischill M, Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Follow-up for ten to 17 years. J Bone Joint Surg (Br) 2005; 87: 1210–15
- Reikeras O, Gunderson R B. Excellent results of HA coating on a grit-blasted stem: 245 patients followed for 8–12 years. Acta Orthop Scand 2003; 74(2)140–5
- Sinha R K, Dangy D S, Yeon H B. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg (Am) 2004; 86: 1254–61
- Specht J, Schneider T, Mecklenbeck W, Arnold W. The femoral neck prosthesis Cut 2000 – first clinical, radiological and scintigraphic results. Orthop Prax 2003; 5: 307–11
- Thomas W, Grundei H. The ESKA femoral neck prosthesis for internal fixation cut. Orthop Prax 1999; 35: 646–52
- Thomas W, Grundei H. The ESKA femoral neck prosthesis Cut for metaphyseal fixation. In: Fixation principles of total hip replacements. Wetzel R. (publisher). Publishing company Steinkopff. 2001
- Thomas W, Lucente L, Mantegna N, Grundei H. ESKA (CUT) endoprosthesis. Orthopäde 2004; 33: 1243–8
- Thoren B, Sahlstedt B. Influence of pelvic position on radiographic measurement of the prosthetic acetabular component. An experimental study on a pelvic model. Acta Radiol 1990; 31: 133–6
- Traulsen F C, Hassenpflug J, Hahne H J. Long term results with cement-free total hip prostheses (Zweymuller). Z Orthop 2001; 139: 206–11
- Walker P S, Blunn G W, Prada de D, Casas C. Design rationale and dimensional considerations for a femoral neck prosthesis. Clin Orthop 2005, 441: 313–9
- Weissinger M, Helmreich C. Langfristige Resultate mit dem zementfreien Alloclassic-Schaft nach Zweymüller. Z Orthop 2001; 139: 200–5
- Witzleb W C, Knecht A, Beichler T, Köhler T, Günther K P. Hip resurfacing arthroplasty. Orthopäde 2004; 33: 1236–42
- Wurnig C, Schwameis E, Bitzan P, Kainberger F. Six-year results of a cementless stem with prophylaxis against heterotopic bone. Clin Orthop 1999, 361: 150–8
