Abstract
Background No data exist regarding mortality rate in young patients with a first–time anterior shoulder dislocation. A cohort of 255 patients aged 12–40 years had a primary anterior shoulder dislocation during the years 1978 and 1979. After 10 years, 9 of the patients had died—which is a high figure for this cohort of patients. The question thus arose as to whether these patients had an increased mortality rate. In this study we have examined the mortality rate in these patients 25 years after the primary dislocation, relative to that of the Swedish population in general.
Patients and methods In 1978 and 1979, 255 patients aged 12–40 years (257 shoulders) with first–time anterior shoulder dislocation were treated with or without immobilization. During 2003 and 2004, a follow-up of all patients who were alive was undertaken and the certificates of causes of death of 27 deceased patients were also analyzed.
Results The mortality rate (SMR) for the patients in this study was more than double that of the general Swedish population (p < 0.001). A higher proportion of the deceased patients had etiology other than sportsrelated activity as a cause of their initial dislocation (p = 0.04). 11 of the 27 who were deceased had died from injury or intoxication (S00–T98, ICD10), which was more than expected relative to the causes of death for the general Swedish population in 2003 and 2004 (p < 0.001)
Interpretation The doubled mortality rate in our cohort of patients is most probably explained by the inclusion of a disproportionate number of patients with alcoholic behavior, which may affect the long-term outcome in trauma series.
When this study started in 1978, the intention was to evaluate whether immobilization of first-time anterior shoulder dislocations would give a better prognosis with respect to recurrences than just symptomatic treatment. The study has resulted in 4 earlier publications covering the 2–, 5–, and 10–year follow-ups (Hovelius et al. Citation1983a, Citationb, Citation1996, Hovelius Citation1987). The present 25–year follow-up started in March 2003 and ended in February 2005, and showed that a relatively high number of patients had died (Hovelius et al. Citation2006).
The main aim of the present study was to determine whether the patients had an increased mortality rate compared to the general Swedish population, and if so, to find a possible explanation for the high death rate by examining the certificates of causes of death. We also wanted to establish whether the patients who died had differed in any way on entering the study from those who were still alive.
Patients and methods
In 1977, one of us (LH) initiated a prospective study to evaluate the results of treatment of primary anterior dislocation of the glenohumeral joint in patients aged 40 years or younger. 27 hospitals located in different urban and rural areas of Sweden participated in the study. During the years 1978–1979, 255 patients (257 shoulders) were included in the study, after excluding 3 alcoholics for whom only second-hand information at the 2 year follow-up was available. 112 shoulders were immobilized for 3–4 weeks (group 1) and a sling was used for 104 shoulders for as long as required (i.e. until the patient was comfortable without it) (group 2). Early in the study, a third group (group 3) was established. In this group, we included patients who had initially been allocated to group 1 but who had not, however, completed the immobilization for at least 21 days (30 patients, 30 shoulders) or who had shoulders that for various other reasons could not be allocated to groups 1 or 2 (41 patients, 41 shoulders). 2 of the latter patients were considered to be alcoholics1. Of the 30 patients who were excluded from group 1 and allocated to group 3 (30 shoulders), 20 had abandoned the treatment by their own initiative, and in 10 cases it was because of wrong information from the doctor.
Of the 257 dislocations originally, 205 (80%) were in male patients. The primary dislocation was related to any kind of sports activity in 128 cases (50%) (Hovelius Citation1982).
The first follow-up was performed after 2 years (Hovelius et al. Citation1983a) and the second after 5 years. 1 patient had died by then (Hovelius Citation1987). 10 years (± 6 months) after the primary dislocation, we started the third follow-up. 8 other patients then died by then (Hovelius et al. Citation1996).
The 25–year follow-up started in 2003 for those shoulders that had dislocated in 1978, and went on during the year 2004 for the patients who had had their primary dislocation in 1979. By February 2005, all patients who were alive had had the 25year follow-up. 19 more patients had died since the 10–year follow-up. 1 of these was excluded from this analysis since the patient had lived in Denmark when he entered the study. Thus, this report covers 227 living patients (229 shoulders since 2 patients were included in the study with both of their shoulders dislocated) and 27 deceased patients.
During the 5–, 10– and 25–year follow-ups (Hovelius Citation1987, Hovelius et al. Citation1996, Citation2006) we realized that some of the patients who were difficult to follow up were alcoholics or drug addicts. Consequently, the patients were also classified in four categories at 25 years: (1) those known by us to be alcoholics, (2) those known by us to be drug addicts, (3) those known by us to be addicted to both alcohol and drugs, and (4) patients for whom we had no indications of any alcohol or drug abuse.
5 patients were classified as pure alcoholics, 1 patient was addicted to mainly drugs, and 3 patients were both alcoholics and drug addicts at the 25year follow-up. In the analysis of the results, all 9 addicts were considered to be alcoholics.
Certificates regarding causes of death were ordered for all dead patients. We also registered whether alcohol was mentioned as a cause of or contributing factor to death. Finally, we made a classification according to the ISD10 system.
Statistics
When standardized mortality rate (SMR) was calculated, we used indirect standardization. The reference population was the whole Swedish population administered by Statistics Sweden (SBC), taking account of age, sex, and calender time. When we calculated “causes of death”, we compared our series with the causes of death for both sexes and all ages in Sweden during 2003 and 2004 (mean value for 2003–2004; Statistics Sweden).
Statistical analysis was performed with Chisquared test. A p-value of < 0.05 was considered significant.
Results
Time of follow-up
Mean follow-up was 25 (24.2–26.4) years. Twothirds of the patients had follow-up of more than 25 years after the primary dislocation; thus, the mortality rate was also analyzed after 26 years. Of our original cohorts of age groups, 4/102 patients originally in the age group 12–22 years, 5/65 in the age group 23–29 years, and 18/95 in the age group 30–40 had died (, ). The increased risk of dying within 25 years was 108% (CI: 33– 208) (p < 0.001).
Numbers of death among the patients who entered this study in 1978 and 1979 (pink) compared to the expected numbers of death based on the general Swedish population taking account to gender, age and calender year (blue).
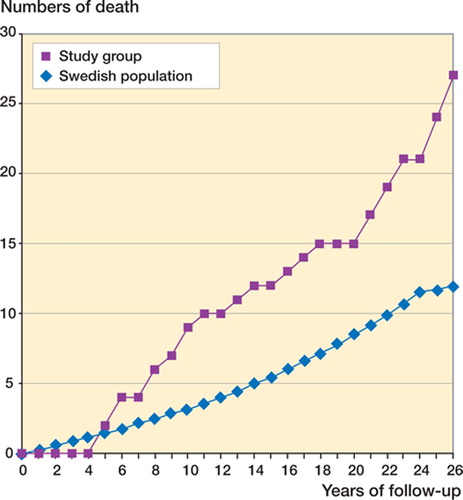
Table 1. Number of expected and documented deceased patients 1–26 years after entering the study
Causes of death
11 of 27 patients had died from injury or poisoning (S00–T98, ). 8/11 that died from injury or poisoning had an anamnesis of alcohol abuse, compared to 3/16 that died by other causes (p = 0.02). In our series of 27 deceased patients, a higher proportion died from “injury and poisoning” and unknown causes than in the general population (p < 0.001). This difference still remained when the 2 patients initially known as alcoholics were excluded (p < 0.001)
Table 2. Causes of death according to ICD10 classification in our series and for the general population during the years 2003–2004 (Statistics Sweden)
Other observations
A higher proportion of deceased patients with the ICD10 diagnosis “injury and poisoning” had been allocated to group 3 (p = 0.06). When both series were analyzed together with respect to these parameters, a higher proportion of shoulders in patients with alcoholic behavior—detected during the different follow-ups or in the death certificates—had been allocated to group 3 when the study was initiated in 1978–1979 (p < 0.001) ().
Table 3. Cause of death according to whether there was an ICD10 diagnosis of S00-T98 (injury or intoxification) or evidence of alcohol addiction at the 25-year follow-up, broken down according to the allocation to treatment groups when this study was initiated
Of the 27 patients who died, an etiology other than athletic activity was recorded for their primary dislocation in 18 cases. This contrasts with the patients who survived, where the first-time dislocation was associated with sports in 128/227 cases (p = 0.04). Furthermore, when we analyzed the patients who died from injury and poisoning (n = 11) together with those classified as addicts in the 25–year follow-up (n = 9), only 3 of the 20 had sports annotated as being the etiology of the primary dislocation, as compared to 134/234 for those for whom there was no evidence of addiction (p < 0.001).
Discussion
This study has shown that 12–40–year–old patients treated at our emergency units in Sweden during the years 1978–1979 because of a first-time anterior shoulder dislocation had a lower survival rate than the general Swedish population. Almost half of those who died did so because of injury or poisoning, or they had a history of alcoholic abuse in their follow-up records. This is much higher than the 5–10% incidence of alcoholism in the general population, which matches that of our survival group (9/229, 4%). Diagnoses of injury or poisoning at death are often related to alcohol abuse, and a higher proportion of patients died from these diagnoses in our study than in the general population during 2003 and 2004. In our opinion, this explains the doubled mortality rate in the present cohort of first-time dislocations.
Furthermore, our study has shown that in the group of patients who died, the cause of the initial dislocation was most often not sports-related. Thus, our conclusion is that a higher-than-average proportion of patients with alcohol-related behavior may be included when a study of this kind is set up. Although we initially classified 5 patients as being alcoholics and excluded 3 patients at 2 years because of uncertainty about their follow-up information (Hovelius et al. Citation1983a), it is difficult to avoid including such patients. The first dislocation may be due to a single bout of drinking; however, a patient's drinking habits may increase with time. 20 patients (15%) did not complete the immobilization treatment by their own initiative, and in some of these cases alcohol-related behavior may have been the explanation for not following our treatment regime. It is also probable that when intoxicated, alcoholics dislocate their shoulders because of falling more often than the general population. Muscular relaxation may contribute to an increased rate of dislocations in this group.
An association between alcoholism and shoulder injuries has already been described by Nordqvist and Petersson (Citation1996). They found that in men between 30 and 64 years of age, almost half of the proximal humerus fractures and shoulder dislocations recorded were sustained by alcohol abusers. Olsson et al. (Citation2003) found an increased mortality rate in patients with a fracture of the surgical neck of the humerus, but they did not attribute this to alcoholic abuse.
In our study it was possible to identify all patients who were still alive after 25 years. Alcoholic patients are, however, extremely difficult to trace in long-term follow-ups and they are often registered as dropouts. The completeness of our study therefore gives us new information regarding the relation between alcoholism and shoulder dislocation.
Contributions of authors
LH has been involved with this study since it started and has also mainly contributed to the 25 years follow-up and the writing of the manuscript. J-ÅN has done all the statistical analyses and together with AN been advisor for the designing of the paper. AN has also considerably contributed to the writing of the manuscript.
- Hovelius L. Anterior dislocation of the shoulder. A clinical study on incidence, prognosis and operative treatment with the Bristow-Latarjet procedure. Linköping University, LinköpingSweden 1982, Thesis 139
- Hovelius L. Anterior dislocation of the shoulder in teenagers and young adults. Five-year prognosis. J Bone Joint Surg (Am) 1987; 69: 393–9
- Hovelius L, Eriksson K, Fredin H, Hagberg G, Hussenius Å, Lind B, Thorling J, Weckström J. Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. J Bone Joint Surg (Am) 1983a; 65: 343–9
- Hovelius L, Lind B, Thorling J. Primary dislocation of the shoulder. Factors affecting the two-year prognosis. Clin Orthop 1983b; 176: 181–5
- Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg (Am) 1996; 78: 1677–84
- Hovelius L, Sandström B, Saebö M, Augustini B-G, Krantz L, Fredin H, Tillander B, Skoglund U, Sennerby U, Salomonsson B, Nowak J. Long-term prognosis of first time anterior shoulder dislocation in the young. 229 shoulders prospectively followed for 25 years. Presented at AAOS, Meeting Chicago. March, 2006
- Nordqvist A, Petersson C J. Shoulder girdle injuries common in alcoholics- An analysis of 413 injuries. Acta Orthop Scand 1996; 67: 364–6
- Olsson C, Nordquist A, Pettersson C. Increased mortality after fracture of the surgical neck of the humerus. A casecontrol study of 253 patients with a 12–year follow-up. Acta Orthop Scand 2003; 74: 709–12
